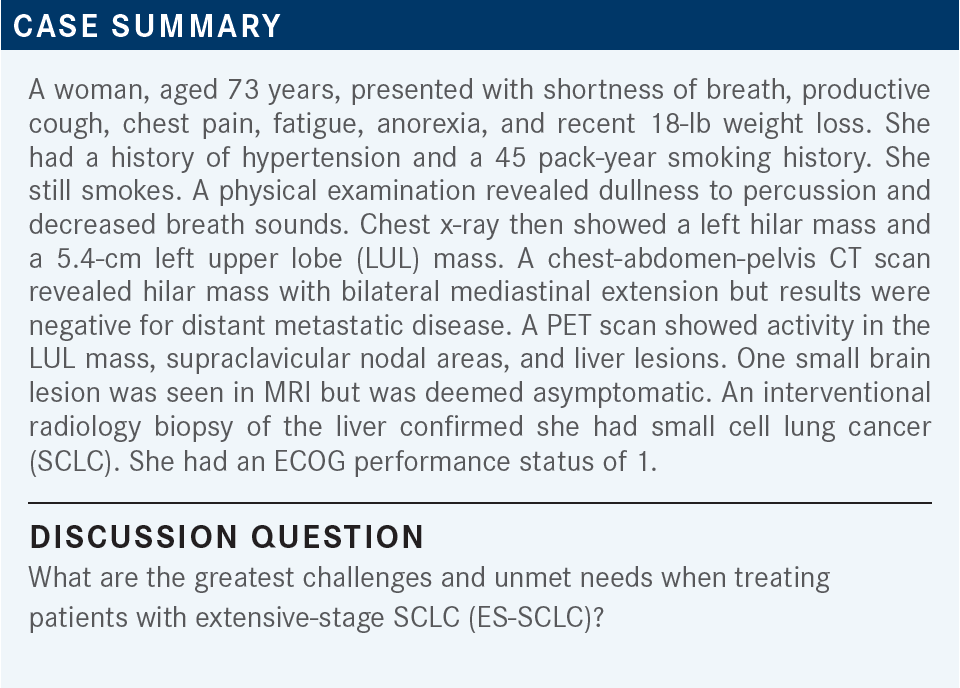
Roundtable Discussion: Kandra Explores Benefit of Chemoimmunotherapy for Small Cell Lung Cancer
During a Targeted Oncology case-based roundtable event, Ajay Kandra, MD, discussed with participants the challenges and treatment options for a patient with extensive-stage small cell lung cancer.
Ajay Kandra, MD (Moderator)
Medical Oncologist/Hematologist
King's Daughters' Health Cancer Treatment Center
Madison, IN

BADIN: One major thing we do not have is a target we can go after, unlike with non–small cell lung cancer [NSCLC]. We do have a driver mutation and subtypes. Today, we still lump all SCLCs under 1 umbrella. I am hoping that soon, for clinical research purposes, we can have better understanding, better subtyping, targeted treatments, and appropriate treatments for patients. Another challenge is these patients are usually sicker than patients with NSCLC.
All of them are smokers with multiple comorbidities. The prevalence of CNS [central nervous system] disease and brain metastases is also a challenge. It is a very difficult disease to treat in general, so [there are] a lot of unmet needs there.
KONALA: The only reason is if I need to start a patient and if we need to treat them in the hospital. I then use chemotherapy first and start immunotherapy from the second cycle. Other than that, most patients I treat in my clinic get immunotherapy up front.
KANDRA: Excellent point. So, you basically add immunotherapy at a later point, not in the hospital?
KONALA: Yes. You cannot use it in the hospital.
KANDRA: That is a fairly common problem because you cannot get immunotherapy from the inpatient pharmacy inventory. Part of it is the cost associated with that.
MULHERIN: The only thing I think of is whether they had a severe autoimmune disease where you would not consider giving immunotherapy. I have never seen that in SCLC. I have seen a couple of patients with NSCLC who might have had granulomatosis with polyangiitis, or I had a patient who had lupus cerebritis—very unfortunate. But never in SCLC. It does not tend to go together.
MUTHUSAMY: We do come across patients with rheumatoid arthritis or lupus getting lung cancer. You must be careful treating them.
MULHERIN: You should be careful and have a risk-benefit discussion with a rheumatologist so everyone is informed and they can be monitored. In general, before I consider not giving immunotherapy, it must be a severe condition.
MUTHUSAMY: I treated a patient with rheumatoid arthritis. He did not have any exacerbation of the rheumatoid arthritis with the immunotherapy. I do not know how common exacerbation of the autoimmune disease is. Does anybody else have experiences like that?
MULHERIN: I have with NSCLC but not with SCLC.
KANDRA: That seems to be the case for well-controlled rheumatoid arthritis without any active immunosuppression. That seems reasonable to try considering the risks and benefits if you have a discussion with the patient, but when patients are on strong immunosuppressive therapy for rheumatoid arthritis, you are talking about a different scenario. With those cases, I doubt we would be pushing for immunotherapy.
MUTHUSAMY: Prednisone at about 10 mg should be a cutoff point. If anything, it is OK to give immunotherapy to patients taking less than 10 mg of prednisone. That seems to be the rule of engagement.
WALLING: I have had 2 patients with MS [multiple sclerosis], if you consider that an autoimmune condition, 1 with NSCLC, and 1 with ES-SCLC. Our doctors of pharmacy did not recommend giving immunotherapy because there were case reports of deaths with MS.1 I do not know about rheumatoid arthritis, even though they were not included in the anyalsis.
KANDRA: Absolutely. It is a rare situation to see patients with MS, but there are contraindications, and I have not used immunotherapy in that setting.
ANWAR: That is my experience too. I do not have any patients with an autoimmune disease, but in my discussions with colleagues, MS is a total contraindication, as is anything that involves the brain or high immunosuppressive medication. Otherwise, for controlled rheumatoid arthritis, [individuals] have used it.
MULHERIN: Another one might be if they have had a solid organ transplant. They had immunosuppressants. So obviously, many of those patients were excluded from trials. In our center [Hematology Oncology of Indiana], there is a large renal transplant program, for example. There are case reports of these patients experiencing rapid allograft rejection. Again, it is SCLC, so a risk-benefit discussion with the transplanting physician is needed.
KANDRA: You are right. And they do have these on the black box warnings, on the labels, for all these immunotherapy drugs at this point. So, all excellent points.
BADIN: Sometimes, for small cell cancer of the GI [gastrointestinal] tract or GU [genitourinary] primary cancer, it might be challenging to get it approved by the insurance. I know we are discussing lung cancer, but we all sometimes see small cell cancer of the prostate and small cell cancer of the colon, and the insurance may not want to cover it sometimes.
MUTHUSAMY: [Most work-up] was already done, including an MRI of the brain. Maybe a PET scan [should be done]?
KANDRA: If it were not SCLC, I am sure we would all be doing something different. We would be ordering more molecular studies, correct?
MUTHUSAMY: Correct.
MULHERIN: Right, but for SCLC there is little else to do unless you are going to send the patient for a clinical trial.
MUTHUSAMY: This patient did not have PET scans. Is there any role for a PET scan under the circumstances? She already has stage IV disease with a solitary asymptomatic brain metastasis smaller than 2 cm.
MAHESHWARI: It all depends on what kind of diagnosis we put in the computer. If we write “SCLC,” insurance will not approve it. If we write “lung cancer,” then they will approve the PET scan.
MUTHUSAMY: Yes, the International Classification of Diseases [ICD] code makes a difference. The artificial intelligence is not that good to discriminate all these things.
“Lung cancer” will be the generic global ICD code that might get you through a lot of things, yes.
KANDRA: I think you are all correct. It is difficult to get approval, but another thing I found helpful is if you put it as a high-grade neuroendocrine [tumor], they will accept it, and you can get that scan done. We have been in those situations where we felt like a PET scan would be helpful in defining whether that adrenal lesion or that liver lesion is hypermetabolic, and we wanted to avoid another biopsy.
KONALA: Choosing either atezolizumab [Tecentriq] or durvalumab [Imfinzi] is fine. But in the clinical trials, the difference is that you use 4 cycles of chemotherapy with atezolizumab and you can go up to 6 cycles with durvalumab.
I think [the IMpower133 trial (NCT02763579) of atezolizumab] did not include patients with brain metastases. I would use a chemoimmunotherapy combination. I do not know how many are using trilaciclib [Cosela], or sometimes we use growth factors in these patients.
MULHERIN: In the CASPIAN trial [NCT03043872] of durvalumab, you could have your choice of platinum-based agents, whether cisplatin or carboplatin.2
I do not use cisplatin if they have metastatic disease—if they are not going to be cured. It is not going to change things substantially. It is probably whatever you feel most comfortable with. Maybe insurance has a preference. I think the data are comparable.
MUTHUSAMY: I think there aren’t any trials with 3-year data available. Even the atezolizumab trial does not have those data published yet.
KANDRA: We have the choice of these 2 immunotherapies, as you all mentioned.
MUTHUSAMY: But I think we all have more experience with atezolizumab than with durvalumab, unless you were in the trial, because durvalumab was just approved in the last couple of years.
KANDRA: Yes, I think it is more like a habit. The first one you start using, you become very comfortable with it. You see some good results. You want to keep going. You do not want to change anything.
How do you decide between carboplatin and cisplatin when using an immune checkpoint inhibitor [ICI]-chemotherapy regimen for SCLC? How important is the platinum agent in your regimen selection?
ANWAR: I think most oncologists in the United States use carboplatin in metastatic settings, just for lesser toxicity.
KANDRA: Absolutely. Less renal toxicity, less ototoxicity, and less nausea with the carboplatin.
MULHERIN: There are no data [suggesting] that they are going to have improved survival in this disease by using cisplatin. So, it is far more toxic.
KANDRA: Absolutely. The only advantage of cisplatin over carboplatin, I would say, is less myelosuppression, and I do not know whether you run into that scenario as much in the first line.

MUTHUSAMY: Progression-free survival [PFS] is increased in both trials.2,3 So, combined chemoimmunotherapy seems to be better than chemotherapy alone. It offers better PFS.
MAHESHWARI: Should we give 4 cycles or 6 cycles?
MUTHUSAMY: I just follow the protocol, so 4 cycles is the standard protocol unless the patients keep responding.4 At least for old-timers like me, if the patients keep responding, I may give additional cycles.
MAHESHWARI: The general rule is, if the patient has significant residual disease and has been responding with a partial response [PR] after 4 cycles, I personally push for 5 or 6 cycles.
MUTHUSAMY: If the patient’s performance status and protoplasm [are] good enough, they may be able to handle 2 more cycles. We should push for minimal disease, theoretically, we can assume immunotherapy is very effective if you have a low tumor burden.
MAHESHWARI: I have 2 patients [for whom] immunotherapy caused a significant disseminated skin rash. I had to stop treatment. Those patients are around 2 years out, still living. I still believe anybody who has a great response but a lot of toxicity from immunotherapy will probably have long or durable responses.
KANDRA: These are excellent points, and we come across this question so often, whether to stop at 4 cycles or go off protocol and do 6.
We know that for some patients with tremendous tumor burden, bad paraneoplastic syndromes, and high-volume disease, that chemotherapy works. But if you follow the data from the trials, we are supposed to do 4 cycles, but I have certainly seen a lot of oncologists go up to 6 cycles in certain patients.
MAHESHWARI: I do not give [patients only] 4 cycles in ES-SCLC. I treat to the maximum response, 4, 5, or 6 cycles.
KANDRA: The protocols recommend a CT scan at the end of 4 cycles. That may be a point where you reassess, see what the disease burden is, and then make an individualized decision with the patient and explain that the trial says 4 cycles of chemotherapy but we can decide to do 6.
Again, that would be considered off-label. Anything else? Dr Raghavan, I am sure you have had a lot of experience.
RAGHAVAN: I would say not with immunotherapy; 4 cycles of chemotherapy is probably because you are using maintenance with the immunotherapy anyway. When we did not have immunotherapy, we were giving 4 and 6 cycles of chemotherapy.
ZAYDAN: Do you have any idea how they decided on 4 cycles when they designed the study?
KANDRA: I never understood the logic behind that. The standard is 4 to 6 cycles, and maybe they are trying to avoid extra toxicities by adding the immunotherapy.
Maybe they were not as sure about the volume of treatment the patient can tolerate when adding something. The strategy might be to cut back on something else.
ANWAR: It may be interesting to see whether the control arm had 4 cycles or 4 to 6 cycles.
KANDRA: CASPIAN [NCT03043872] allowed 6 cycles whereas IMpower133 only allowed 4 cycles in the control arm.3
MUTHUSAMY: We want something rather than the current chemotherapy, but it is not a fantastic home run; the HRs were all close to 1, [including] 0.96 [for a subgroup]. I am not sure what that means; the average is [0.76] and the P value is .01.6 I am not sure whether the HR means anything if the P value is .01.
KANDRA: You raise a valid point. Yes, we need something more in SCLC; there are so many unmet needs in SCLC, and that reflects in our opinions on the results of these trials. We certainly want to see more substantial benefit and even more drastic HRs, but that has not happened. Yes, the HR is close to 1 in the subgroup of patients with brain metastases.
MUTHUSAMY: Even the overall HR [of 0.76] has a P value of .01, [meaning that] even if 2 patients got better, it would look like the HR is good. But the P value should be [more] significant. The P value in this study is .01. [However], the 1-year and 2-year overall survival [OS] rates are better than chemotherapy, and that is very encouraging.6
KANDRA: When we look at those subgroups, we cannot draw statistical conclusions. The trials are not powered to have strong statistical data. We use them to [ask], “Are we learning something in each of these subgroups? Can we apply these data into our practice? Or can we do more trials to know more about what we are seeing?”
MULHERIN: It is depressing that this is probably the biggest advance in SCLC in the past 30 years. That is a 2-month OS advantage. [The chemotherapy regimen] is from the 1980s and probably the most significant advantage is the improvement in supportive medications like antiemetics.
[Chemoimmunotherapy] is better, and I was enthusiastic when I started using it, but patients with brain metastases do worse overall. Is that because they are on steroids? Are the steroids negating the treatment?
There are all kinds of things you could try to analyze, but regardless, it is what it is. These are the best tools we have available. If they have brain metastases, they need to get radiotherapy.
MUTHUSAMY: Yes. That is why we are using this regimen.
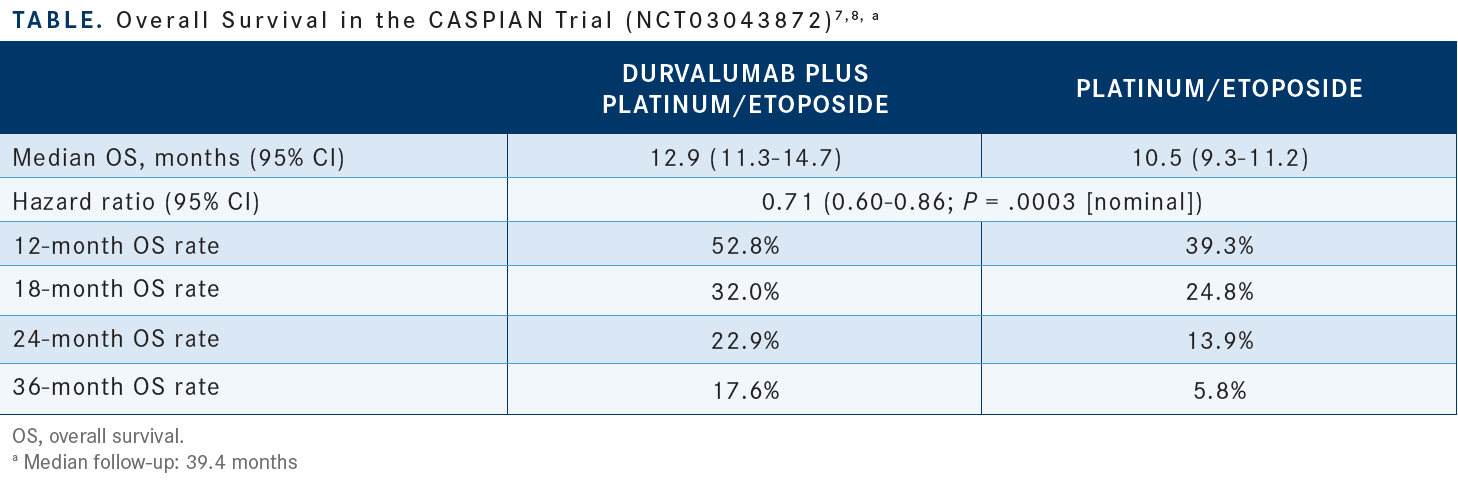
MUTHUSAMY: They have clear 3-year data, and the Kaplan- Meier curve is much more open than the IMpower133 Kaplan-Meier curve. I can see much more separation [between experimental and control arms] in CASPIAN than in IMpower133.6,7 I think durvalumab seems to be appealing based on this 3-year report [Table2,7]. Hopefully, the atezolizumab data will be released soon enough, so we can see the differences between those 2 regimens.
KANDRA: Yes, I would be very eager to look at what the latter part of the follow-up shows.
NIDHIRY: I agree that there is a longer follow-up with CASPIAN and durvalumab, but I feel that the benefits are still comparable. Although it is not a head-to-head study, there is some modest benefit with addition of immunotherapy to chemotherapy in this disease, but the overall outcome is still poor. We reach for that because we do not have better treatment options. We go with what we have. I feel that either option will be reasonable in the setting.
KANDRA: Do you have other input as to the data about the brain metastases? Do you think one is superior to the other?
BARAI: The survival data certainly seem interesting with this combination. I think I will tend to give it a use, and a longer-term follow-up is also appropriate to see the benefits.
KANDRA: What does anyone think about using 6 cycles vs 4 cycles in the control arm? Is that important when you are making any conclusions as to what the real-world experience is?
BARAI: That depends on the patient situation. It is understandable that when a clinical trial is going on, you want to have a certain defined [duration]. During the actual patient situation, if the patient has an 80% or so response with heavy disease, you are not going to stop at 4 cycles [if] the benefit is continuing to accrue and the patient is able to tolerate it. Sometimes we try to blindly follow the trial data, but the trial has a certain defined situation when they want to be able to analyze it.
ANWAR: You can make the other case too. The control arm got 6 cycles, while the immunotherapy arm got 4 cycles, and still those 6 cycles did not show any improvement. If you look at the 2 trials, the PFS was the same with atezolizumab as well as with durvalumab.2,3 So, I am not sure whether the addition of 2 cycles is making any difference in the treatment. You can use it in certain cases.
MUTHUSAMY: Did they look at the stratification of complete responses [CRs] and PRs? Did they do any differently between each arm?
KANDRA: They did break it down to CRs vs PRs. I believe patients with CRs are still less than 10% in both trials.2,3 But the [PR rate] is much higher in the durvalumab trial at around 66%.
MUTHUSAMY: Did the patients with CRs do a lot better than those with PRs? If it is a 10% response, only 26 out of 260 patients would have CRs in the trial.
KANDRA: I think based on our overall experiences with any other cancers or any other trials, generally patients with CRs tend to have much longer disease-free intervals and better overall outcomes. I do not think we can [conclude] a lot about these specific data, but in general we all like CRs.
REFERENCES
1. Garcia CR, Jayswal R, Adams V, Anthony LB, Villano JL. Multiple sclerosis outcomes after cancer immunotherapy. Clin Transl Oncol. 2019;21(10):1336-1342. doi:10.1007/s12094-019-02060-8
2. Paz-Ares L, Dvorkin M, Chen Y, et al; CASPIAN investigators. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929-1939. doi:10.1016/S0140-6736(19)32222-6
3. Horn L, Mansfield AS, Szczęsna A, et al; IMpower133 Study Group. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220-2229. doi:10.1056/NEJMoa1809064
4. NCCN. Clinical Practice Guidelines in Oncology. Small cell lung cancer, version 2.2022. Accessed July 20, 2022. https://bit.ly/2JTv4zC
5. Reck M, Liu SV, Mansfield AS, et al. IMpower133: updated overall survival (OS) analysis of first-line (1L) atezolizumab (atezo) + carboplatin + etoposide in extensive-stage SCLC (ES-SCLC). Ann Oncol. 2019;30(suppl 5):v710-v711. doi:10.1093/annonc/mdz264
6. Liu SV, Reck M, Mansfield AS, et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J Clin Oncol. 2021;39(6):619-630. doi:10.1200/JCO.20.01055
7. Paz-Ares L, Chen Y, Reinmuth N, et al. LBA61 - Durvalumab ± tremelimumab + platinum-etoposide in first-line extensive-stage SCLC (ES-SCLC): 3-year overall survival update from the phase III CASPIAN study. Ann Oncol. 2021;32(suppl_5):S1283-1346. doi:10.1016/annonc/annonc741