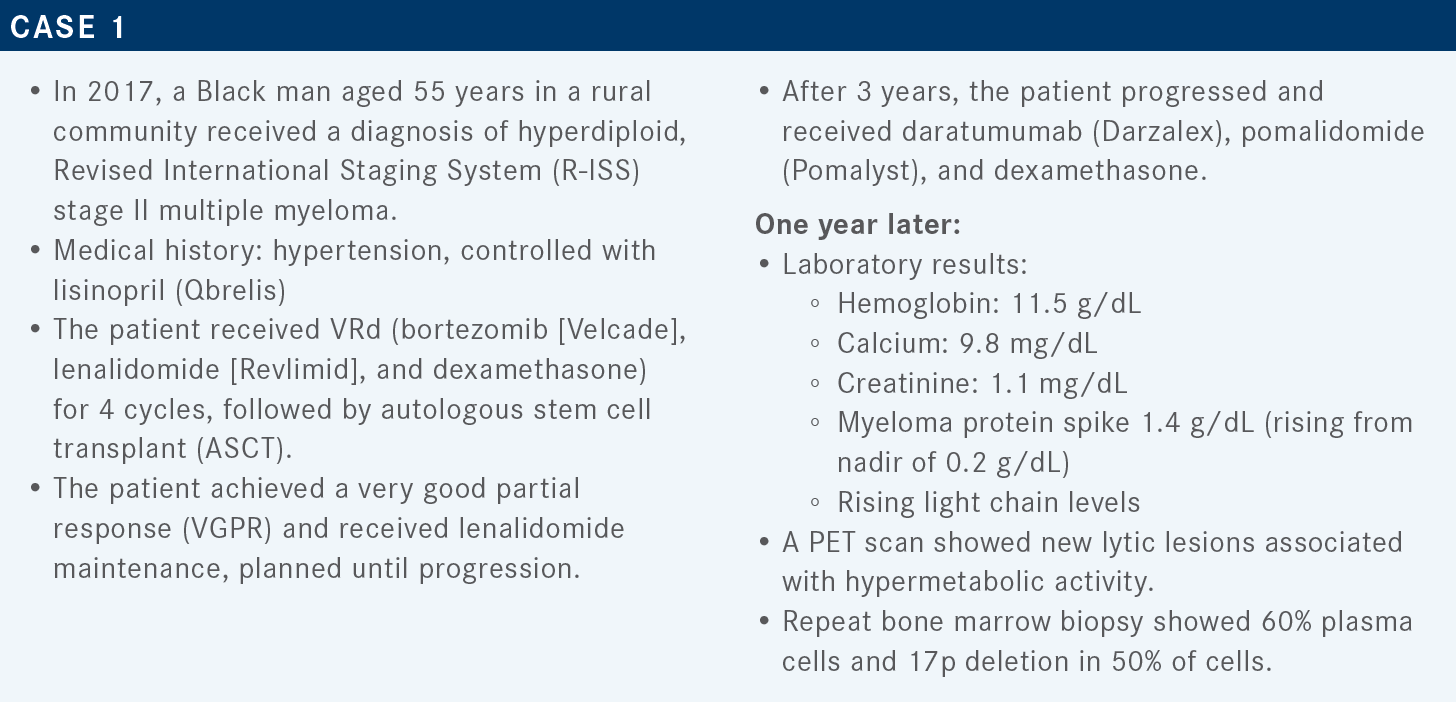
Rifkin and Forsberg Review Trials of BCMA-Targeted Therapies for Relapsed/Refractory Multiple Myeloma
During a Targeted Oncology case-based roundtable event, Peter Forsberg, MD and Robert M. Rifkin, MD, FACP, discussed the trials supporting the use of BCMA-targeted agents for relapsed/refractory multiple myeloma.
Peter Forsberg, MD
Associate Professor, Medicine- Hematology
University of Colorado School of Medicine
Denver, CO

Robert M. Rifkin, MD, FACP
Medical Oncologist/Hematologist
Rocky Mountain Cancer Centers
Denver, CO
Targeted OncologyTM: What role does B-cell maturation antigen (BCMA) play in the pathogenesis and treatment of multiple myeloma?
RIFKIN: [This receptor] is highly expressed in normal and malignant plasma cells, and it’s on the surface of nearly all myeloma cell lines. Malignant plasma cells tend to have a lot more BCMA than do normal ones. Increased BCMA levels are associated with poorer outcomes, and upregulated expression during myeloma pathogenesis and evolution [progresses] from a normal [state to] monoclonal gammopathy of undetermined significance, then to smoldering multiple myeloma, and [finally to] active multiple myeloma.1
I think [many physicians] are becoming more familiar with BCMA-targeted therapy. [In the case of therapy with] an antibody-drug conjugate [ADC], the ADC is internalized; the linker is hydrolyzed, and the payload is released to cause cell death. [In the case of BCMA-targeted chimeric antigen receptor (CAR) T-cell therapy], CAR T cells binding to BCMA on the myeloma cell surface leads to CAR T-cell activation, cytotoxic cytokine release, and myeloma cell death. And finally, bispecific antibodies link BCMA on multiple myeloma cells and CD3 [on T cells], [triggering T-cell activation], release of cytotoxic cytokines, and then multiple myeloma cell death. So, BCMA is going to be an extraordinarily important target.1
What therapies do the National Comprehensive Care Network (NCCN) guidelines recommend for patients who have received more than 3 prior therapies?
[It is important to note that] we’re coming into an era in which we have late relapses; that is, relapses in patients who have received more than 3 prior therapies. [According to the NCCN], after at least 4 prior therapies—including an anti-CD38 monoclonal [antibody], a proteasome inhibitor [PI], and an immunomodulatory drug [IMiD]—you could consider belantamab mafodotin [Blenrep], and you could consider idecabtagene vicleucel [ide-cel; Abecma] or ciltacabtagene autoleucel [cilta-cel; Carvykti]. For patients who have received more than 1 PI, more than 1 IMiD, and an anti-CD38 monoclonal antibody, you could consider selinexor [Xpovio] plus dexamethasone.2
What resources exist for choosing options after the second or subsequent lines of therapy?
The European Hematology Association and the European Society for Medical Oncology3 and the International Myeloma Working Group [IMWG]4 also offer guidelines for treating refractory or relapsed multiple myeloma [RRMM] after the second or subsequent line of therapy. [According to IMWG], when daratumumab, carfilzomib [Kyprolis], or elotuzumab [Empliciti] are not available, patients can receive [pomalidomide plus dexamethasone, with or without cyclophosphamide (Cytoxan)].
There are [also many] alternatives that have been approved, including selinexor, panobinostat [Farydak], oral PIs, and for slightly older patients, we can remember giving VdT-PACE [bortezomib, dexamethasone, and thalidomide (Thalomid), plus cisplatin, doxorubicin (Adriamycin), cyclophosphamide, and etoposide], which ended up landing a lot of patients in the hospital but was effective. Other investigational agents include, melphalan flufenamide [Pepaxto], BCMA-targeted agents [including CAR T cells and bispecific antibodies], and, for a small subset of patients, venetoclax [Venclexta]. Venetoclax is an option in patients who have translocation t(11;14) or high expression of BCL2.4
What data support the use of belantamab mafodotin for RRMM after 3 or more prior lines of therapy?
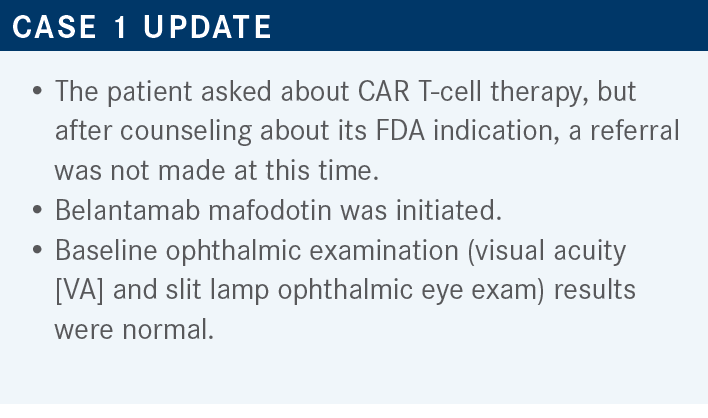
Those data come from the DREAMM-2 trial [NCT03525678]. In this trial, patients were treated until disease progression or unacceptable toxicity, with a primary outcome of overall response rate [ORR]. Secondary end points [included duration of response (DOR) as well as other efficacy outcomes and safety].
Patients had to have measurable disease, a decent performance status, and 3 or more [prior] lines of therapy. Also, patients had to be refractory and not [previously] exposed to a BCMA-targeted therapy. Prior ASCT was allowed; [allogeneic stem cell transplants were excluded].5,6 The baseline characteristics of the 2.5 mg/kg cohort show that it was a representative population. [The median] number of prior therapies [was 7]. The ISS stages I, II, and III [were represented by 22%, 34%, and 43% of the cohort, respectively].6
At the 13-month data cutoff, the ORR in this heavily pretreated population was about 32%. There were a few complete responses [CRs] and stringent CRs [5% and 2%, respectively], and a lot of stable disease [28%], PRs [13%], and VGPRs [11%]. This was not unexpected in this group. Responses did deepen over time. And [among patients with] high-risk cytogenetics or renal impairment, the response and survival outcomes were consistent with those of their [respective] populations. Not surprisingly, as we’re learning now, outcomes were poorer in patients with extramedullary disease.6
The most common adverse events [AEs] included keratopathy; significant cytopenias, a very rare infusion-related reaction; fatigue; and some neutropenia—a variety of things that were not totally unexpected.6
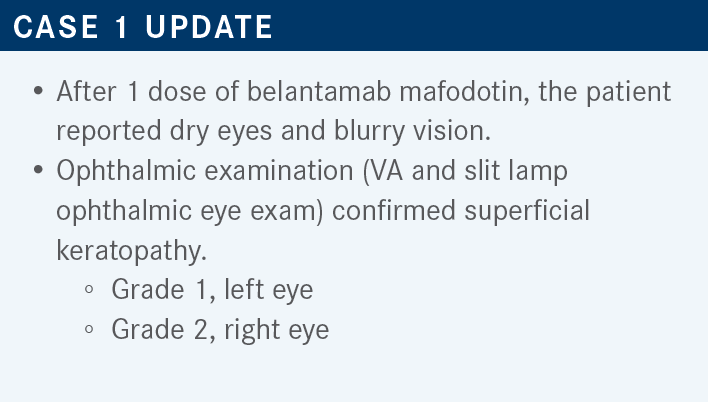
What are some considerations for managing keratopathy?
Considerations include how to best interact with your patient’s eye care provider, [implementation of] the Risk Evaluation and Mitigation Strategies program, the frequency of ophthalmologic examinations, and resources for managing ocular toxicity.
Keratopathy [can present] with or without symptoms. In the paper by Sagar Lonial, MD, [72% of patients in DREAMM-2] had any symptomatic or asymptomatic keratopathy, [56% of patients] were symptomatic, and [18% of patients] had VA changes. [Alternately, 82% of patients did not have] a clinically significant VA change. Discontinuation due to corneal AEs was not high [in 3% of patients]. There was 1 patient with a corneal ulcer.7
There is a significant warning about treatment-related corneal events [that arise from treatment with belantamab mafodotin]. Baseline examination is required, along with follow-ups. And you do have to delay treatment until improvement. You resume at [the same dose or at a] reduced dose, and you may even consider permanently discontinuing [treatment] based on severity.8
In my experience, the patients will hold up the stop sign when they’re ready to stop. And [when treating], you should go through the available data [when advising patients]. We ask patients to use preservative-free lubricant eye drops 4 or more times a day. Contact lenses should only be used with [the supervision of] an ophthalmologist, and those can be corneal bandages. We do worry about [VA and] difficulty driving or operating machinery.8
There are recommended dose modifications [for stepwise decreases in best corrected VA (BCVA)]. Importantly, when you get to [a BCVA of] grade 2 and beyond, you should start to withhold the belantamab mafodotin until the patient experiences an improvement in corneal findings and an [improvement in VA to grade 1 or less]. When the patient is at grade 4, you should [consider] permanent discontinuation, and [if you do continue treatment], you would require a substantial treatment delay. The interesting thing about this drug is it produces deep responses, and they can be long-lasting enough that you can spread out and reduce the dose of belantamab mafodotin.9
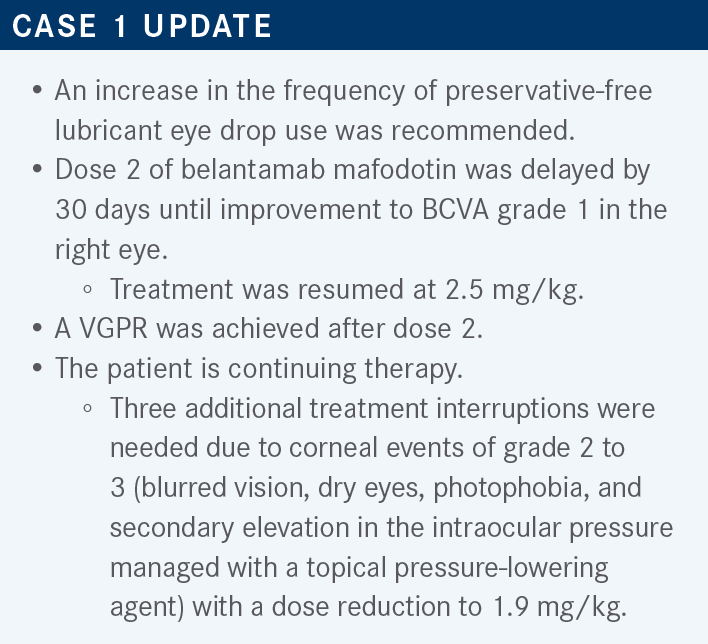
How does this compare with the DREAMM-2 trial?
Among the clinical responders [in DREAMM-2], even with [88% experiencing] clinical benefit in the first dose delay, 38% deepened their response, and keratopathy was the most frequent reason for the dose delays.6
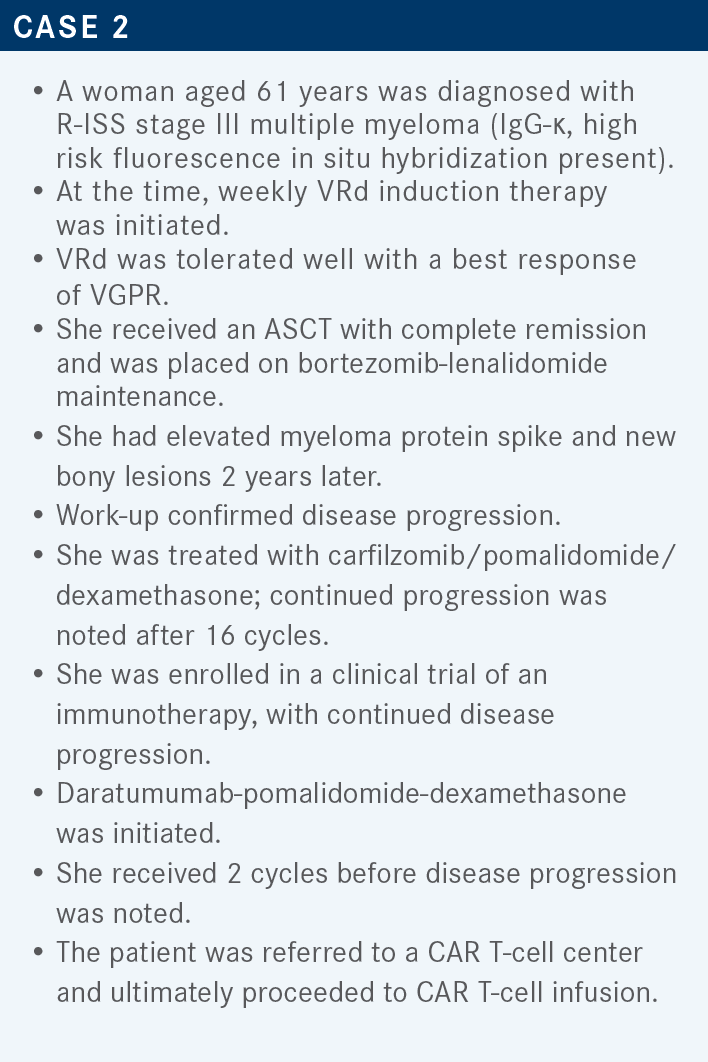
Targeted OncologyTM: What data supported the approval of ide-cel, the first approved CAR T-cell therapy?
FORSBERG: [That approval was based on the data from] the pivotal phase 2 KarMMa trial [NCT03361748].10 This therapy was developed first by bluebird bio, then Celgene. This was studied in a heavily pretreated patient population [in which patients had received] more than 3 prior lines of therapy, including a prior IMiD, a PI, and an anti-CD38 therapy; this shaped the approval indication.11
These patients were treated with 3 days of lymphodepleting chemotherapy, which was fludarabine and cyclophosphamide, on days −5, −4, and −3, which is a standard lymphodepletion approach. Then, patients were infused with the CAR T cells that had been manufactured, [a process requiring] about a month. There was a range of cell doses that patients received, and the primary end point was ORR.11
It is notable that [the tumor response] was cell dose dependent. The relatively small number of patients who got a modest dose of 150 × 106 CAR T cells had an ORR of about 50%. In the larger group of patients who got 300 × 106 cells, the ORR was about 70%, and in the patients who got 450 × 106 [cells], [the ORR] was 81%. So, predictability of those cell yields is a bit harder to achieve, but it did impact how deep the ORR was and how many patients achieved things like VGPR, CR, or better.11
Cell dose also impacted how durable the responses were. Not surprisingly, patients who got deeper responses had more durable responses. Patients who achieved a VGPR had a median DOR of [10.4 months; 95% CI, 5.1-11.3]. The median DOR was [19.0 months; 95% CI, 11.3–not estimable (NE)] in patients with a CR. For patients who only achieved a PR, the median DOR was only 4.5 months [95% CI, 2.9-6.7], which is suboptimal.11
In patients who got the highest cell dose, 450 × 106, the median progression-free survival [PFS] was [12.1 months; 95% CI, 8.8-12.3] vs only [5.8 months; 95% CI, 4.2-8.9] in the 300 × 106 cell-dose group, and only [2.8 months; 95% CI, 1.0–NE] in the 150 × 106 cell-dose group. So, for patients who got a suboptimal cell dose, and who got a suboptimal response, those remissions ended up not being all that durable, whereas if patients got a better cell dose and a better depth of response, they did have more stable remission. We see that essentially all patients have demonstrated progression on this KarMMa trial of ide-cel in relapsed, heavily pretreated patients.11
The [toxicity profile in this trial includes] the AEs you think about most often when we’re thinking of a CAR T-cell therapy, such as cytokine release syndrome [CRS]. When I counsel patients, I tell them that they’re almost assuredly going to get CRS. In this trial, 84% of patients had CRS, and only 5% of patients had CRS of grade 3 or 4. So, we don’t [see] much high-grade or life-threatening CRS. Neurotoxic effects occurred at a relatively low rate.
This [consisted mostly of] classical immune effector cell–associated neurotoxicity syndrome [ICANS], the type of neurotoxicity that is most characterized with CAR T-cell therapy. About 18% of patients experienced neurotoxic effects of any grade, and about 3% had neurotoxic effects of grade 3 or higher. Some of the other AEs that we commonly see include higher-grade myelosuppression in the setting of the lymphodepleting chemotherapy that the patients receive.11
What data supported the subsequent approval of cilta-cel CAR T-cell therapy?
Both [ide-cel10 and cilta-cel12] were approved based on single-arm phase 2 trials. [Cilta-cel was approved based on the phase 1b/2] CARTITUDE-1 study [NCT03548207].12 CARTITUDE-1 was similar in design to KarMMa; patients needed to have received 3 or more prior lines of therapy, including a prior PI, an IMiD, and an anti-CD38 monoclonal antibody.
The patients went through similar apheresis, followed by bridging as needed; neither of the studies mandated bridging therapy. Then, patients received fludarabine and cyclophosphamide lymphodepletion, and then cell infusion. [There was a] lower potential cell-dose target with cilta-cel, and similar structured follow-up.11,13,14
In both [KarMMa and CARTITUDE-1, the patients] were heavily pretreated. [In CARTITUDE-1], the patients had received a median of 6 prior lines of therapy. Most of these patients [66%] had greater than 5 prior lines of therapy, [87.6%] were triple-class refractory, and [42.3%] were penta-drug refractory, meaning they were refractory to lenalidomide, pomalidomide, bortezomib, carfilzomib, and daratumumab. And unfortunately, as in many of these CAR T-cell trials, Black patients were underrepresented, which has been an unfortunate characteristic of a lot of these studies. A decent number of patients, [13.4%] had extramedullary disease. [This was a smaller percentage] than in KarMMa, which physicians sometimes point to [as a cause] of the difference between the activity profiles [of the respective therapies], but it’s hard to say [whether that is truly a cause].11,14
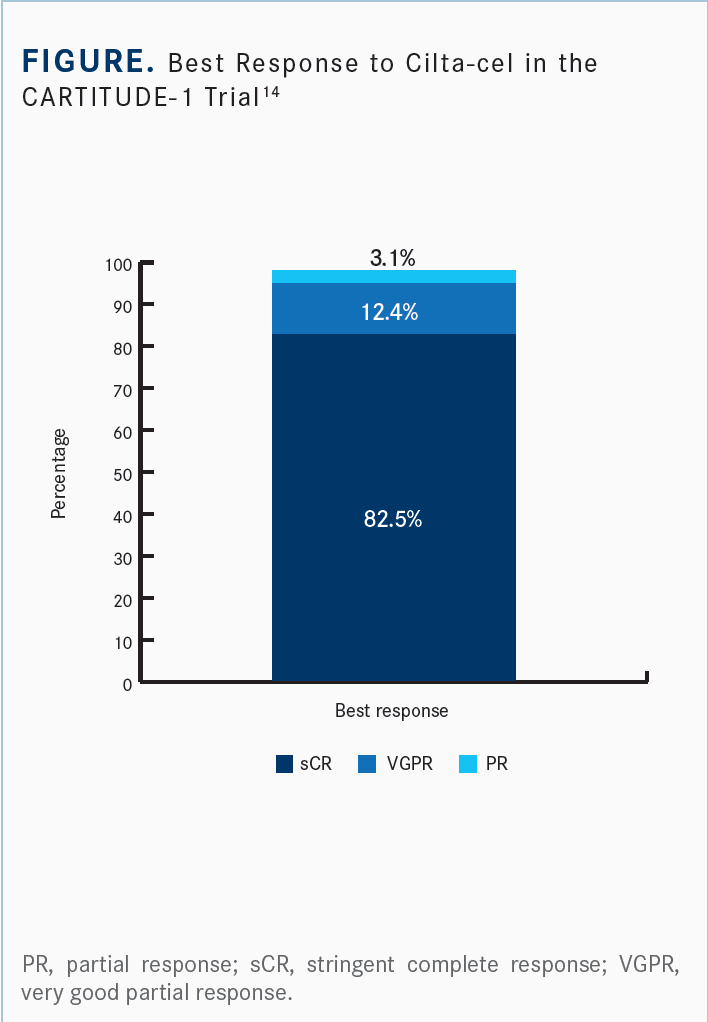
The efficacy profile that we have to date is from the American Society of Hematology Annual Meeting and Exposition in 2021 [Figure14]. The ORR was [97.9%], and a robust percentage of patients achieved a CR or better: 82.5% achieved stringent CR, and [94.9%] achieved VGPR or better. Median DOR has not yet been achieved. As with most CAR T-cell profiles in myeloma, the [median] time to first response was brisk [1 month; range, 0.9-10.7].14 The median time to best response [2.6 months; range, 0.9-17.8] is probably a [reflection] of how long it takes to clear out [the] paraprotein in the blood. Marrow responses are even faster than what you see in the blood; these patients often get their deepest response in the marrow quickly.
The survival [data are] a little different, [in my opinion], from what we saw with KarMMa. After a 2-year median follow-up, the median PFS with cilta-cel [had not been reached],14 unlike ide-cel, which produced a median PFS in the 8-month to 10-month range.11 With cilta-cel, [60.5%] of patients had not progressed [at 2 years]. And, in patients who achieved a deeper response, including the large portion of patients who achieved minimal residual disease negativity [92%], the response was even more durable. So, cilta-cel [produced] impressive DOR and depth of response.14
[There were many] different toxicities associated [with this treatment]; high-grade hematologic toxicities were common. Recovery from this is much [closer to] what you’d see with regular semi-intensive chemotherapy, [rather than] what we see with myeloablative conditioning for transplant or even some infusional intensive chemotherapy with VdT-PACE and [similar regimens]. CRS was, again, experienced by 95% of patients, but [there was a] very low percentage of CRS events of grade 3 or higher [4%].13,14
A different neurotoxicity profile is one of the important things to note about the CARTITUDE-1 data13,14 vs the KarMMa data.11 In CARTITUDE-1, 21% of patients experienced neurotoxicity, and 9% had high-grade neurotoxicity. This [neurotoxicity] included both ICANS, the classical CAR T-cell–associated toxicity, as well as some other neurotoxicities, which included neurocognitive and kinetic issues in about 12 patients.13,14
REFERENCES
1. Yu B, Jiang T, Liu D. BCMA-targeted immunotherapy for multiple myeloma. J Hematol Oncol. 2020;13(1):125. doi:10.1186/s13045-020-00962-7
2. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 5.2022. Accessed July 3, 2022. https://bit.ly/2T0mDYS
3. Dimopoulos MA, Moreau P, Terpos E, et al; EHA Guidelines Committee; ESMO Guidelines Committee. Multiple myeloma: EHA-ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32(3):309-322. doi:10.1016/j.annonc.2020.11.014
4. Moreau P, Kumar SK, San Miguel J, et al. Treatment of relapsed and refractory multiple myeloma: recommendations from the International Myeloma Working Group. Lancet Oncol. 2021;22(3):e105-e118. doi:10.1016/ S1470-2045(20)30756-7
5. Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21(2):207-221. doi:10.1016/S1470-2045(19)30788-0
6. Lonial S, Lee HC, Badros A, et al. Longer term outcomes with single-agent belantamab mafodotin in patients with relapsed or refractory multiple myeloma: 13-month follow-up from the pivotal DREAMM-2 study. Cancer. 2021;127(22):4198-4212. doi:10.1002/cncr.33809
7. Lonial S, Nooka A, Thulasi P, et al. Recovery of ocular events with longer-term follow-up in the DREAMM-2 study of single-agent belantamab mafodotin (Belamaf) in patients with relapsed or refractory multiple myeloma (RRMM). Paper presented at: 62nd American Society of Hematology Annual Meeting and Exposition; December 5-8, 2020; virtual. Abstract 3224. Accessed July 5, 2022. https://bit.ly/3c9xr1K
8. Blenrep. Prescribing information. GlaxoSmithKline; 2022. Accessed July 5, 2022. https://bit.ly/3O1fsIe
9. Risk Evaluation and Mitigation Strategy (REMS) document: Blenrep (belantamab mafodotin) REMS program. FDA. Accessed July 5, 2022. https://bit. ly/3cap2v9
10. FDA approves first cell-based gene therapy for adult patients with multiple myeloma. News release. FDA. March 27, 2021. Accessed July 6, 2022. https:// bit.ly/3PEjSpR
11. Munshi NC, Anderson LD Jr, Shah N, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705-716. doi:10.1056/NEJMoa2024850
12. FDA approves ciltacabtagene autoleucel for relapsed or refractory multiple myeloma. FDA. Updated March 7, 2022. Accessed July 7, 2022. https://bit. ly/3uDjzU3
13. Berdeja JG, Madduri D, Usmani SZ, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398(10297):314-324. doi:10.1016/ S0140-6736(21)00933-8
14. Martin T, Usmani SZ, Berdeja JG, et al. Updated results from CARTITUDE-1: phase 1b/2 study of ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T cell therapy, in patients with relapsed/ refractory multiple myeloma. Presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 9-16, 2021; Atlanta, GA. Abstract 549. Accessed July 7, 2022. https://bit.ly/3z04kHh