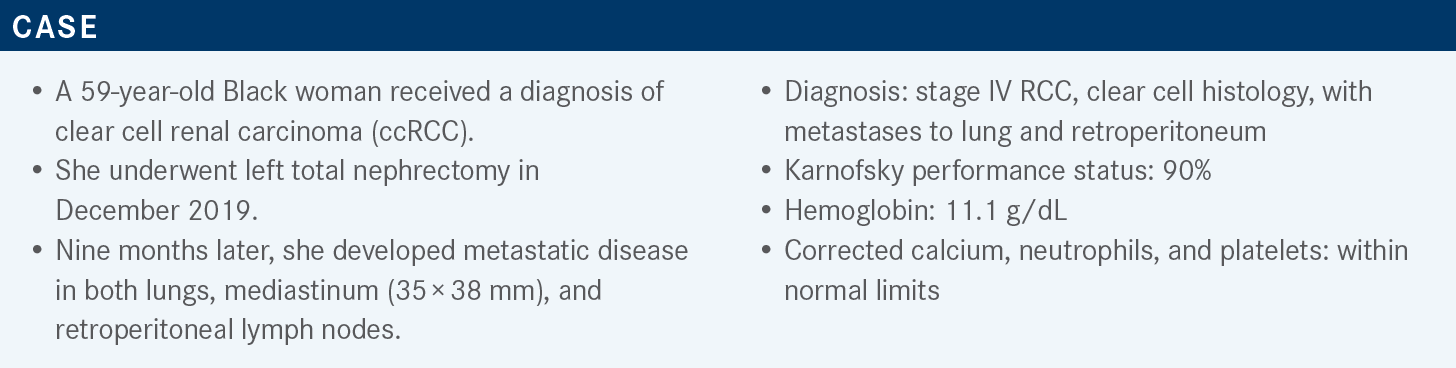
Park Discusses Results of Multiple Phase 3 Trials in ccRCC
During a Targeted Oncology case-based roundtable discussion, Chandler Park, MD, discussed the trials that led to the approval of frontline combination regimens for patients with advanced clear cell renal cell carcinoma.
Chandler Park, MD
Medical Oncologist
Norton Cancer Institute
Assistant Professor
University of Louisville School of Medicine
Louisville, KY

Targeted OncologyTM: What first-line systemic therapies do the National Comprehensive Cancer Network guidelines recommend for patients with relapsed or stage IV ccRCC?
PARK: For [patients with] poor- and intermediate-risk ccRCC, we have 4 options: axitinib [Inlyta] plus pembrolizumab [Keytruda; axi-pembro]; cabozantinib [Cabometyx] plus nivolumab [Opdivo; cabo-nivo]; ipilimumab [Yervoy] plus nivolumab [Opdivo; ipi-nivo]; and lenvatinib [Lenvima] plus pembrolizumab [len-pembro].
We’re at a fork in the road. On the one hand, we have [ipi-nivo], a dual checkpoint inhibitor combination, and on the other, we have tyrosine kinase inhibitor [TKI] plus immunotherapy combinations. Within that category, we have 3 different options. We also have single-agent cabozantinib if the patients, for whatever reason, cannot get immunotherapy, such as in cases of tough immunocompromised disease or colitis.1
What can we learn from recent phase 3 trials that have explored first-line immune checkpoint inhibitor combinations in metastatic RCC?
It is difficult to compare studies, especially since the favorable-, intermediate-, and poor-risk categories were different for every patient population. Also, in some studies, such as KEYNOTE-426 [NCT02853331], cytoreductive nephrectomy was included. But in the CheckMate 9ER trial [NCT03141177], some of those patients had de novo disease, so they didn’t have cytoreductive nephrectomy. Comparing the results of these studies is comparing apples with oranges. The original premise was that patients with more immunogenic, metastatic ccRCC tend to have more poor-risk disease, as opposed to patients with vascular disease, for whom a TKI tends to be more effective and among whom a higher percentage has favorable-risk disease.
The CheckMate 214 study of ipi-nivo [NCT02231749] is the most mature study, extending beyond 5 years. It was first released at the ESMO [European Society for Medical Oncology] Congress in 2017. The percentages of patients in this study with favorable, intermediate, and poor risk were 23%, 61%, and 17%, respectively.
Median follow-up was 67.7 months, and median overall survival [OS] was 55.7 months vs 38.4 months for ipi-nivo vs sunitinib [Sutent], respectively [HR, 0.72; 95% CI, 0.62- 0.85]. The landmark OS [at 12 months] was 83% vs 78%, respectively, with a progression-free survival [PFS] HR of 0.86 [95% CI, 0.73-1.01]. The overall response rate [ORR] was 39% vs 32%, and the rate of complete response [CR] was 12% vs 3%, respectively.2,3
The other 3 studies [KEYNOTE-426, CheckMate 9ER, and CLEAR (NCT02811861)] were similar in terms of the treatments’ mechanisms of action. In each of these studies, 1 treatment was a TKI—axitinib, cabozantinib, or lenvatinib, respectively. [These were combined with] PD-1 inhibitors: pembrolizumab, nivolumab, and pembrolizumab, respectively. What stands out is that the CheckMate 9ER study had a higher percentage of poor-risk patients at 19% [vs 13% for the KEYNOTE-426 study and 9% for the CLEAR study].
The CLEAR and KEYNOTE-426 studies had more favorable-risk patients, 31% [and 32%], respectively, with the percentages of intermediate-risk patients approximately the same among the 3 studies. Median follow-up for the KEYNOTE-426 study was approximately a year ahead of that for the CheckMate 9ER and the CLEAR studies, so it’s still not comparable. You have to wait until we can compare apples with apples.
The other thing that stands out is the OS at 1 year. If you start a patient today on a treatment, what are the chances that the patient will be alive in 1 year? In the KEYNOTE-426 study of axi-pembro and in the CLEAR study of len-pembro, OS was 90% as opposed to 83% in the CheckMate 214 trial. For PFS, the CLEAR study stands out [HR, 0.39; 95% CI, 0.32-0.49], but there were more favorable-risk patients in that study. The ORR was 71% for the CLEAR study, 56% for the CheckMate 9ER study, and 60% for the KEYNOTE-426 study. The rate of CR in the CLEAR study was 16%, vs 12% for the CheckMate 9ER study and 10% for the KEYNOTE-426 study.4-8
How do the results of these trials affect your clinical practice?
On the first CT scan after 3 months in the CLEAR study, only 5% of the patients had progressive disease [PD].7 That means that 95% had better than PD. That’s why, if a patient has symptomatic disease, I lean more toward [using drugs with] 2 different mechanisms of action, a TKI and immunotherapy. For the patients who are asymptomatic with diffuse disease, where I have some time [in case] I get no response—like 15% to 20% of the patients in the CheckMate 214 study2,3—I can try to bail them out [later] with a TKI. That’s how I think about these things.
What additional data shed light on the combination of lenvatinib plus pembrolizumab as treatment for patients with ccRCC?
The phase 3 CLEAR study of frontline therapy compared single-agent sunitinib with lenvatinib plus either pembrolizumab or everolimus [Afinitor]. Patients were randomly assigned 1:1:1 among the 3 arms. The primary end point was PFS and the secondary end point was OS.7
This study had a median follow-up of 26.6 months, which is the earliest of all these studies. In the PFS comparison of len-pembro with sunitinib, the HR was 0.39 [95% CI, 0.32-0.49; P < .001], which equates to a 61% reduction [in progression or death]. There was a clear separation [of the survival curves as early as] the first CT scan at approximately 3 months. The len-pembro combination [had the best performance], followed by lenvatinib plus everolimus and then by sunitinib. There was [an improvement of] 14.7 months with len-pembro vs sunitinib in terms of the PFS.
What were the results of the CLEAR trial subgroup analysis?
The PFS results favored both of the combination regimens over sunitinib across all evaluated subgroups, including those based on Memorial Sloan Kettering Cancer Center or International Metastatic RCC Database Consortium risk groups.7
Whether defined by age, sex, geographic region, risk status, number of organs with metastasis, or even PD-L1 score, all subgroups favored len-pembro. In the prespecified [analysis of adverse prognostic features], every group favored len-pembro. This analysis included groups defined by the presence or absence of prior nephrectomy, sarcomatoid features—which some consider a biomarker for checkpoint inhibitor [responsiveness]— and baseline metastasis.7 In the earlier CABOSUN study [NCT01835158] and other cabozantinib studies, patients with bone metastases [and also those without] tended to favor [the experimental treatment]. Similarly, in the CLEAR study, patients with bone metastases and those without all favored len-pembro.7
Please describe the OS and response rate results of this trial.
The OS results are puzzling. [Although the survival curves showed] great separation in terms of the PFS, and it is still early, the OS tails off a little bit [with initially separate curves coming together over time], and OS for sunitinib does seem to [eventually exceed the OS for the other 2 arms]. [At a median follow-up of 26.6 months], the HR for len-pembro vs sunitinib was 0.66 [95% CI, 0.49-0.88], but with that said, at approximately 33 to 36 months, the [total] number of patients was very low, so this [trend] is something that has to be followed up. The HR for OS, [in a comparison of len-pembro vs sunitinib], favored len-pembro in most subgroups, including groups defined by PD-L1 positive vs negative, with an exception in patients with International Metastatic RCC Database Consortium favorable risk.7
The confirmed rate of CR was 16.1% for len-pembro, 9.8% for lenvatinib plus everolimus, and 4.2% for sunitinib. The rates of PD were 5.4%, 7.3%, and [14.0%], respectively.7 Among patients who achieved a CR with len-pembro in the intention-to-treat population, 79.3% maintained a CR at 2 years, and 74.3% maintained a CR at 3 years.8
What might explain the surprising OS results?
There was a higher percentage of favorable-risk patients in the CLEAR study, [but] 26.6 months is very premature, and the number of events is very low. We’ll have to see what this looks like [after follow-up].
Which treatment-related adverse events (TRAEs) were noted in the CLEAR study, and what are the dosing considerations for physicians using the lenvatinib plus pembrolizumab combination?
Overall, the TRAE profiles of the len-pembro and the sunitinib arms seem very similar. The diarrhea was more pronounced in the len-pembro arm, as was hypertension. Dysgeusia was a little higher in the sunitinib arm, and the levels of alanine aminotransferase and aspartate aminotransferase were less in that arm.7
The recommended dosage is 20 mg of lenvatinib daily plus 200 mg of pembrolizumab every 3 weeks. After 2 years of the combination, interestingly enough, lenvatinib doesn’t need a partner; usually you need everolimus, but here it’s administered as a single agent until PD. The capsules come in 10-mg and 4-mg doses. The dose reduction sequence from 20 mg is to come down to 14 mg, followed by 10 mg and then 8 mg. Lenvatinib can be dose reduced, withheld, or discontinued as recommended. Pembrolizumab can be withheld or discontinued, [but not dose reduced], as recommended.9,10
What data support the use of cabozantinib plus nivolumab for the management of metastatic ccRCC?
These data come from the CheckMate 9ER study, which was similar [to the CLEAR study in that] the comparison arm was sunitinib. Nivolumab was given at 240 mg. [But in contrast, whereas the] lenvatinib dose went from 18 mg to 20 mg, which is a higher dose, for the CheckMate 9ER study, the dose of cabozantinib was reduced from 60 mg to 40 mg. The primary end point was PFS. The secondary end point was OS.5
The PFS, after an [18.1]-month follow-up, was 16.6 months [95% CI, 12.5-24.9] vs 8.3 months [95% CI, 7.0-9.7] for the experimental and comparator arms, respectively [HR, 0.51; 95% CI, 0.41-0.64; P < .0001], with clear separation of the survival curves after the first CT scan at 3 months.5 [After a 33-month follow-up, median PFS values remained the same (HR, 0.56; 95% CI, 0.46-0.68).6] The results of the subgroup PFS analysis were similar to those of the other combinations, [in that] all subgroups favored cabo-nivo.5
The secondary end point of final OS was analyzed after a median of 33 months of follow-up. At 24 months, survival in the experimental and comparator arms was 70.3% vs 60.3%, respectively. The median OS was 37.7 months vs 34.3 months [HR, 0.70; 95% CI, 0.55-0.90], which is not much of a difference.6 Still, the study is premature.
At the 32.9-month follow-up, for the experimental and comparator arms, the ORR was 55.7% vs 28.4%, and the rate of CR was 12.4% vs 5.2%, respectively. The median duration of response was 23.1 months vs 15 months.6 Safety was assessed at a minimum follow-up of 10.6 months. The median duration of therapy for cabo-nivo vs sunitinib was 14.3 months vs 9.2 months, respectively. The percentage of patients with at least 1 dose reduction was 56.3% vs 51.6%, and the treatment discontinuation rate was 44.4% vs 71.3%, respectively.11 At 32.9 months’ median follow-up, TRAEs of any grade affected 97% vs 93% of the respective arms. TRAEs of grade 3 affected 65% vs 54% of the respective arms. There were more diarrhea and elevated alanine aminotransferase and aspartate aminotransferase in the cabo-nivo arm. For the most part, everything else was similar.6
In the CheckMate 214 study, OS was approximately 55 months.2 In the CheckMate 9ER study, which included low-risk patients, OS was only 37 months.6 How do you interpret these results?
That is a good question. At the beginning [of the study], you lose up to 20% of the patients [to a lack of] response, but then [the remaining patients] have a better chance of stabilizing with a CR.6 So it boils down to picking which patients you think will [fail to respond] in the first 3 months.
What are your thoughts about the COSMIC-313 trial (NCT03937219), which combined cabo-nivo with ipilimumab, a CTLA-4 inhibitor?12
It’s going to be interesting to see the toxicity results. With a dual checkpoint inhibitor, you lose something at the beginning, but then you benefit with CR on the right-hand tail of the [survival] curve. It would be the best of both worlds to have the cabozantinib holding the response rate at the beginning, with the PFS, and then to maintain the CR on the right side of the curve with the ipilimumab. The toxicities and the CR are going to be interesting with this triplet therapy.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Kidney cancer, version 3.2023. Accessed October 2, 2022. https://bit.ly/2TAx1m3
2. Motzer RJ, Tannir NM, McDermott DF, et al. Conditional survival and 5-year follow-up in CheckMate 214: first-line nivolumab + ipilimumab (N + I) versus sunitinib (S) in advanced renal cell carcinoma (aRCC). Ann Oncol. 2021;32(suppl 5):S685-S687. doi:10.1016/j.annonc.2021.08.057
3. Albiges L, Tannir NM, Burotto M, et al. Nivolumab plus ipilimumab versus sunitinib for first-line treatment of advanced renal cell carcinoma: extended 4-year follow-up of the phase III CheckMate 214 trial. ESMO Open. 2020;5(6):e001079. doi:10.1136/esmoopen-2020-001079
4. Rini BI, Plimack ER, Stus V, et al. Pembrolizumab (pembro) plus axitinib (axi) versus sunitinib as first-line therapy for advanced clear cell renal cell carcinoma (ccRCC): results from 42-month follow-up of KEYNOTE-426. J Clin Oncol. 2021;39(suppl 15):4500. doi:10.1200/JCO.2021.39.15_suppl.4500
5. Choueiri TK, Powles T, Burotto M, et al; CheckMate 9ER Investigators. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829-841. doi:10.1056/NEJMoa2026982
6. Powles T, Choueiri TK, Burotto M, et al. Final overall survival analysis and organ-specific target lesion assessments with two-year follow-up in ChackMate9 ER: nivolumab plus cabozantinib versus sunitinib for patients with advanced renal cell carcinoma. J Clin Oncol. 2022;40(suppl 6):350. doi:10.1200/JCO.2022.40.6_suppl.350
7. Motzer R, Alekseev B, Rha SY, et al; CLEAR Trial Investigators. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289-1300. doi:10.1056/NEJMoa2035716
8. Grünwald V, Powles T, Kopyltsov E, et al. Analysis of the CLEAR study in patients (pts) with advanced renal cell carcinoma (RCC): depth of response and efficacy for selected subgroups in the lenvatinib (LEN) + pembrolizumab (PEMBRO) and sunitinib (SUN) treatment arms. J Clin Oncol. 2021;39(suppl 15):4560. doi:10.1200/JCO.2021.39.15_suppl.4560
9. Lenvima. Prescribing information. Eisai; 2022. Accessed November 3, 2022. https://bit.ly/3VMFoeF
10. Keytruda. Prescribing information. Merck; 2022. Accessed November 3, 2022. https://bit.ly/3Xb5vgf
11. Choueiri TK, Powles T, Burotto, et al. Nivolumab + cabozantinib vs sunitinib in first-line treatment for advanced renal cell carcinoma: first results from the randomized phase III CheckMate 9ER trial. Ann Oncol. 2020;31(suppl 4):S1159. doi:10.1016/j.annonc.2020.08.2257
12. Exelixis announces cabozantinib in combination with nivolumab and ipilimumab significantly improved progression-free survival in phase 3 COSMIC-313 pivotal trial in patients with previously untreated advanced kidney cancer. Exelixis. July 11, 2022. Accessed November 3, 2022. https://bit.ly/3QBhh1D

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen