Evaluating Risk Factors and Treatment for Tumor Lysis Syndrome
During a Targeted Oncology™ Case-Based Roundtable™ event, Javier Pinilla-Ibarz, MD, PhD, discussed risk factors and treatment options for tumor lysis syndrome.
Javier Pinilla-Ibarz, MD, PhD
Head of Lymphoma Section
Department of Malignant Hematology
Moffitt Cancer Center
Tampa, FL
Targeted OncologyTM: Can you discuss the risk assessment of tumor lysis syndrome (TLS) and in which cancer types this can occur?
PINILLA-IBARZ: The risk assessment of TLS in lymphomas, acute and chronic leukemias, myeloma, and solid tumors defines high, intermediate, and low risk.1 One of the things that always surprises me is that technically the risk [of TLS] is not very high.
When we’re talking about lymphomas and acute leukemia, Burkitt or lymphoblastic lymphoma is the classical condition where spontaneous TLS can happen, due to the massive proliferation of B cells, but that also happens as soon as we introduce therapies. [High-risk TLS can be indicated when the] lactate dehydrogenase [(LDH) level] is more than 2 times the limit of normal. Advanced age can also precipitate TLS. Then you have earlier stage, or, in the low risk, you can argue for the classical lymphomas: follicular, Hodgkin, MALT [mucosa-associated lymphoid tissue], and so on.
CLL [chronic lymphocytic leukemia] is technically a small lymphocytic lymphoma. But in ALL [acute lymphoblastic leukemia], every time that you see high blood cell counts— more than 1000 × 103/uL—we’re talking about ALL. The same thing can happen in AML [acute myeloid leukemia]. When you have very high blood cell counts and a very high LDH level as a marker of very rapid proliferative disease, it becomes high risk. Most of these patients will be inpatients, and we will have to follow them very closely.
When we go to intermediate and low risk, you’re going to have less leukocytosis and lower LDH levels, which is used as a tremendous marker for how those patients can evolve when treated. And we have more uncommon lymphomas, like anaplastic large cell lymphoma, and other rare variants. Children with these conditions can also have high or intermediate [risk], depending on the stage, high LDH level, and so on.
For many years we’ve used chemoimmunotherapy for CLL, but incorporation of obinutuzumab [Gazyva] or venetoclax [Venclexta] has clearly brought the possibility of TLS. However, you may have had issues before with rituximab [Rituxan] in very sensitive patients, which may precipitate this problem in the older population.
Myeloma and other solid tumors may not be at such a high risk. They’re different and may not have a large amount of circulating cells. For this reason, the population may not be at high risk. But some of the patients with CLL may be, based on a very high proliferative rate, mainly in the relapsed setting with a very high white blood cell count, as well as bulky lymphadenopathy. We’re discussing risk factors, and they can be related to the disease, the patients, and factors related to the treatment.1,2
What are the disease-related risk factors for TLS?
Rapid cellular proliferation with a high LDH level as a translational [marker] of this rapid proliferation is very important, as well as high tumor burden. Bulky lymph nodes of more than 10 cm, or white blood cell counts of more than 25 ×103/uL, are well exemplified when we discuss the way that we assess TLS risk, for example, with venetoclax. But you can apply this easily to other conditions.
[Regarding] the sensitivity to cytoreductive therapy, some of these new therapeutic strategies produce rapid destruction of the cells through immunologic mechanisms, like monoclonal antibodies, through blockade of BCL2. Lenalidomide [Revlimid] and other drugs may have these problems, although to a lesser extent. Bone marrow involvement and renal infiltration or problems of obstruction can also have a role, as well as splenomegaly as a manifestation of bulky disease.
What are the patient-related risk factors for TLS and treatment-related factors?
There is no doubt that renal disease, [including] nephropathy, renal failure, or urinary tract obstruction, plays a very important role in the risk of these patients, and we have to pay specific and detailed attention to that.
[This includes] pretreatment of hyperuricemia or hyperphosphatemia; hypovolemia or hypotension as triggers for further precipitation of uric acid; acidic urine; congestive heart failure; and in general our older population, who may have higher risk of dehydration.
Finally, treatment-related factors [include] the intensity of these cytoreductive agents. But when we [treat] patients, inadequate hydration, concurrently with the use of nephrotoxic agents, precipitates many of the problems that we encounter in TLS.
Which hematologic disorders carry a high risk for TLS?
Burkitt lymphoma/leukemia, ALL—lymphoblastic lymphomas is what we call ALL with more than 100,000/uL, same thing with AML—[are high risk].3 The high LDH [level shows high risk] in aggressive lymphomas like a lymphoblastic lymphoma—that’s pretty much an ALL—and diffuse large B-cell lymphoma, adult or pediatric, with very high LDH levels and a bulky tumor situation. [With] mantle cell lymphoma, you could argue that some of these can also present very aggressively with high LDH levels and bulky [disease]. CLL with bulky lymphadenopathy and increased lymphocytes, especially using venetoclax, [also carries a high risk].
The first time that we use a monoclonal antibody, [TLS] is something that we need to keep in mind. I mention this because with the use of venetoclax, everyone is concerned about TLS, but I came to the realization that we have seen TLS many times with obinutuzumab or even rituximab, and we never paid too much attention. But I have seen those cases.
What therapies are associated with increased risk for TLS or elevated uric acid?
We can classify [the therapies as follows]: chemotherapies—for example, bendamustine [Belrapzo, Treanda], doxorubicin [Adriamycin], methotrexate, and vincristine [Oncovin]; followed by the monoclonal antibodies in the form of rituximab or obinutuzumab4,5; but also the bispecific T-cell engagers, with blinatumomab [Blincyto] as a classical example. We’re using this strategy to try to eliminate minimal residual disease, but using this more in patients who have relapsed disease, we can encounter this problem.
Then we’re going to targeted therapies, like proteasome inhibitors, although you can argue that [TLS] may not be as common. With TKIs [tyrosine kinase inhibitors], there is not such a high risk; however, patients may have high blood cell counts at the beginning, and dasatinib [Sprycel] or even other drugs can produce a rapid drop on white blood cell counts and precipitate [TLS] in that population.6
Lenalidomide [is no longer used in leukemia treatment], but it was very well reported that the use of this was associated in some patients with TLS. [Additionally, we have] the classical manifestation of a potent BCL2 inhibitor, finally in our clinics after so many years: venetoclax.7 Venetoclax is a unique-class drug in BCL2 inhibition. This is pretty much the long list of drugs that can be associated [with TLS].
What is the Cairo-Bishop definition for TLS?
Much of the literature on TLS comes from pediatric patients and pediatric oncologists.8 They defined these 2 main syndromes: clinical TLS and laboratory TLS. It’s fundamental to recognize laboratory TLS to avoid stepping forward to clinical TLS. These are the classical intrinsic tumor-related factors that we already discussed: high proliferative rate, high-risk cancer, large tumor burden, and chemosensitivity; and the patient-related [risk factors, including] renal issues, inadequate hydration, and hyperuricemia preceding treatment.
What is [laboratory] TLS? Two or more of the following laboratory abnormalities, within 3 days prior to the use of therapy or 7 days after the initiation of therapy. It’s easy to remember: uric acid levels greater than 8 mg/dL, potassium levels above 6 mEq/L, phosphate levels greater than 6.5 mg/dL in children or 4.5 in adults, and calcium less than 7 mg/dL.
What is not easy to remember—and I have encountered cases like this—is that [the definition includes] “or 25% change from the baseline of any of the above analytes.” I have to admit, sometimes I may miss those things if I’m not paying attention and some of these things may predict that these patients—maybe not on the first day, but later on—will encounter the problem.
What you don’t want to happen is to not treat laboratory TLS early. Hydrate them; use very aggressive hydration. With medication, if you’ve not started, for example, allopurinol [Lopurin] or rasburicase [Elitek], I would start that later on. We don’t want to go to clinical TLS because the clinical TLS is what established the consequences of these laboratory abnormalities. We are talking about an increase in creatinine level, at 1.5 times the upper limit of normal. Cardiac arrhythmias can precipitate sudden death. Seizures also can be seen as well, and the problem of sudden death.
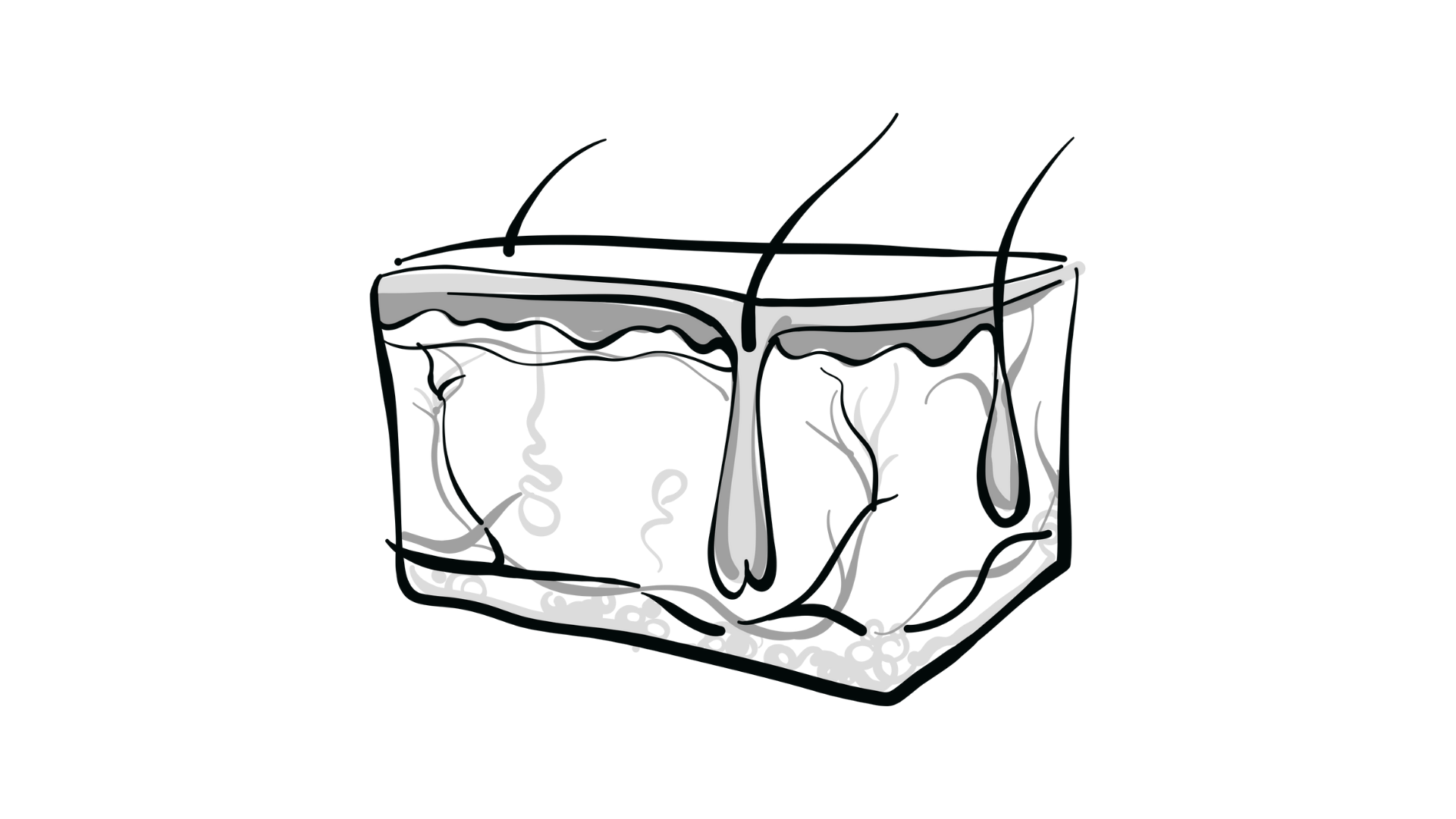
Can you discuss the pathophysiology of TLS?
The pathophysiology of the syndrome [shows]…how to follow the purine catabolism: the hypoxanthine to xanthine oxidase, to xanthine, and then to uric acid.8,9 We are used to seeing allopurinol as a way to block this process. However, once the uric acid is there, it’s there; and it’s important to remember, the only way to get rid of uric acid right away is with rasburicase. It’s the way that [it is metabolized into] allantoin and can be excreted through the kidneys. But there’s no doubt that the accumulation of uric acid in the form of crystals, nephrocalcinosis, obstructive nephropathy, and even xanthine nephropathy due to allopurinol therapy, because you have increase in that metabolism, can be factors that contribute to this syndrome.
Hyperphosphatemia, with secondary hypocalcemia, and also, classically, renal failure and seizures, as well as cardiac abnormalities, [can be seen]. This is manifested by hypocalcemia and [electrocardiogram] changes, and the hyperkalemia that everyone is concerned about because maybe it’s more dangerous, outside of this abnormal renal dysfunction, paresthesia, and weakness. And we don’t want to go to the more advanced stages.
What kind of TLS prevention guidance is available for oncologists?
The [question] is how and when we intervene, depending on if the patient is low, intermediate, or high risk—less than 1%, 1.5%, more than 5%.1,3 In the low risk [cases], we can argue that we watch, we give fluids; definitely…allopurinol, [which] we use in everyone. With intermediate risk, we start to consider some additional kinds of intervention. We can argue that for more aggressive hydration—sometimes [we] have that in...the day after or even before or immediately after the therapy—we’re going to give allopurinol, but rasburicase may definitely be considered.
I really have experience with that, so I try to assess all these risk factors, and the disease, and the condition itself. In our algorithm, we introduced newly diagnosed, high–blood cell count CLL as a potential risk factor to do that. In this case, you could argue for the…prophylactic use of rasburicase; and a low dose of this is easier and less costly than the standard treatment dose, so may be something to consider.
In the high-risk [case], you’re going to throw everything [at it], including the prophylactic rasburicase, and have a much closer look at the laboratory results after you start this therapy. In low- and intermediate-risk patients, after 12 hours or more, if nothing happens, you may feel more comfortable, while in high-risk patients, using rasburicase, you have to [monitor them] better.
We have to remember that G6PD deficiency has to be ruled out. Sometimes it’s tricky, because [although] the risk is low, it’s something that you may encounter, so it has to be taken into consideration. Unfortunately, we had a recent case with G6PD deficiency [in someone who received] rasburicase. It’s something that we should pay attention to.
Can you go over hydration for TLS prevention?
We’re talking about fluids, aggressive oral hydration. Everyone claims to do that, but sometimes it’s hard with an older population to make sure that they are hydrating properly.10 In high-risk patients, we need to go through intravenously and try to do these high rates of 2500 to 3000 mL/m2 per day. It’s important to consider that we may get in trouble, because pulmonary edema is one of the most common manifestations in our older population when we introduce chemotherapy. A balance between hydration and fluid overload has to be considered, but maintain the urine output at more than 100 mL per hour.
What is the evidence for using rasburicase for controlling uric acid?
It’s from an older study; Jorge Cortes, MD, published it in 2010.11 It was a phase 3 study of rasburicase for control of plasma uric acid in adult patients with risk of TLS. The enrollment criteria were active leukemia, lymphoma, or high potential for TLS. One group of patients received 5 consecutive days of rasburicase of 0.2 mg/kg per day, the second group received rasburicase for 3 days followed by allopurinol, and the last group received allopurinol. The anticancer therapy was initiated 4 to 24 hours after the first antihyperuricemic dose. The primary end point was uric acid response rate. Secondary end points were the area under the curve and time to plasma uric acid control.
The “risk for TLS” definition in this specific trial, relatively similar to the one that we have, is [a higher than] baseline plasma uric acid level of 7.5 mg/dL. Some patients may have higher levels, but some patients have lower with high-risk factors—aggressive lymphoma or leukemia, AML, CML blast crisis, even high-grade MDS [myelodysplastic syndrome]— the classical manifestation [of] high risk. [Potential risk for TLS included] more than 2 times the upper limit of normal LDH and advanced stage with a large lymph node of more than 5 cm.
The use of rasburicase or rasburicase with allopurinol provided significantly higher control of plasma uric acid compared with allopurinol alone. But it’s more dramatic when you see the [patients treated] with or without allopurinol; there was this dramatic drop in the uric acid. You can argue [that in] some patients, [uric acid levels] started to go up.
You can go from 0 to 2 or 3 in the group that did not continue [rasburicase], and can argue that it’s OK. But I think what’s dramatic is the mechanism of action of rasburicase, as enzymatic activity and immediate destruction of all the uric acid [takes place] in 4 hours. That is pretty much the time that it takes to produce this effect. Sometimes the pharmacist may tell you that you need to wait 4 hours before you start chemotherapy, but the truth of the matter is that effect is immediate and the maximum effect will happen after 4 hours.
The incidence of TLS and renal events [shows that one could] argue the laboratory TLS happens more [often] with allopurinol compared with rasburicase. Similarly, one can argue that [with] rasburicase/allopurinol, some of the laboratory manifestations [had a higher] incidence with allopurinol alone. Some clinical TLS happened even in the second [use of] rasburicase. Some diseases and conditions, even in the best situation, still may cause trouble, and sometimes I encounter that.
Even after using all my prophylactic measures, I still may find these severe problems…like renal dysfunction. But the use of more aggressive strategies can lower the risk of these conditions. Drug-related adverse events [AEs] were very low in general. But you can argue that some of these AEs could be artifacts [because] the therapies employed in the treatment of these patients can also produce fatigue, pain, anorexia, and so on. What you see in general is not a significant AE profile, but it may be a little more when you compare with the allopurinol alone. Although [the profile] may be mixed, because allopurinol can also produce problems like a classical skin rash, that sometimes can be dramatic.
REFERENCES
1. Williams SM, Killeen AA. Tumor lysis syndrome. Arch Pathol Lab Med. 2019;143(3):386-393. doi:10.5858/arpa.2017-0278-RS
2. Matuszkiewicz-Rowinska J, Malyszko J. Prevention and treatment of tumor lysis syndrome in the era of onco-nephrology progress. Kidney Blood Press Res. 2020;45(5):645-660. doi:10.1159/000509934
3. Cairo MS, Coiffier B, Reiter A, Younes A; TLS Expert Panel. Recommendations for the evaluation of risk and prophylaxis of tumour lysis syndrome (TLS) in adults and children with malignant diseases: an expert TLS panel consensus. Br J Haematol. 2010;149(4):578-586. doi:10.1111/j.1365-2141.2010.08143.x
4. Marqibo. Prescribing information. Acrotech Biopharma LLC; 2020.
5. Sury K. Update on the prevention and treatment of tumor lysis syndrome. J Onco-Nephrol. 2019;3(1):19-30. doi:10.1177/2399369319837212
6. Sprycel. Prescribing information. Bristol-Myers Squibb Company; 2021.
7. Venclexta. Prescribing information. AbbVie Inc; 2022.
8. Puri I, Sharma D, Gunturu KS, Ahmed AA. Diagnosis and management of tumor lysis syndrome. J Community Hosp Intern Med Perspect. 2020;10(3):269-272. doi:10.1080/20009666.2020.1761185
9. Coiffier B, Altman A, Pui CH, Younes A, Cairo MS. Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review. J Clin Oncol. 2008;26(16):2767-2778. doi:10.1200/JCO.2007.15.0177
10. Goodrich A. Advanced practice perspectives on preventing and managing tumor lysis syndrome and neutropenia in chronic lymphocytic leukemia. J Adv Pract Oncol. 2021;12(1):59-70. doi:10.6004/ jadpro.2021.12.1.5
11. Cortes J, Moore JO, Maziarz RT, et al. Control of plasma uric acid in adults at risk for tumor Lysis syndrome: efficacy and safety of rasburicase alone and rasburicase followed by allopurinol compared with allopurinol alone––results of a multicenter phase III study. J Clin Oncol. 2010;28(27):4207-4213. doi:10.1200/JCO.2009.26.8896