Roundtable Discussion: Coleman Examines Dose Management in Endometrial Cancer
During a Targeted Oncology case-based roundtable event, Robert Coleman, MD, discussed dosing of lenvatinib plus pembrolizumab in patients with endometrial carcinoma.
Robert Coleman, MD (Moderator)
Chief Scientific Officer
US Oncology Research
Texas Oncology
The Woodlands, TX

CASE SUMMARY:
A 64-year-old postmenopausal woman presented with abnormal uterine bleeding for approximately 3 months. She has 2 grown children and no known family history of cancer. She has a body mass index of 32, with hypertension controlled with medication. A physical exam showed a large uterus and right lower quadrant abdominal tenderness on palpation.
An endometrial biopsy showed the patient had an International Federation of Gynecology and Obstetrics (FIGO) grade 1 endometrioid adenocarcinoma. Surgery included exploratory laparotomy, total abdominal hysterectomy, and bilateral salpingo-oophorectomy with bilateral pelvic node dissection.
Her pathology revealed she had grade 2 endometrioid adenocarcinoma with 18 negative pelvic nodes and an invasive myometrium of 2.1 cm to 2.3 cm. The immunohistochemistry showed she was HER2 negative, estrogen receptor negative, and had FIGO stage IB (T1b, N0, M0), grade 2 endometrial adenocarcinoma.
DISCUSSION QUESTIONS
- What diagnostic testing do you typically order for a patient who presents with abnormal uterine bleeding?
- Should every patient have molecular testing? What biomarkers are you testing for and why?
- When should testing be ordered?
- What kind of testing do you use in practice? How are you using the results?
- How do you assess prognostic risk?
COLEMAN: This patient has already had some diagnostic intervention, and I’m curious as to what you normally get on your endometrial pathology specimens as part of routine care, without asking the pathologist for additional information.
ARJUNAN: I’m a medical oncologist [at] Texas Oncology in South Dallas, and I usually don’t get anything extra. If we want something, we usually have to ask for it. I don’t see many gynecologic oncology cases, but for these kinds of cases, I might ask for microsatellite instability [MSI] status up front.
COLEMAN: [Dr Koon], let me ask you, because you’re operating on these patients: What do you normally get from your pathologist when you get a primary specimen back?
KOON: I’m in gynecologic oncology at Baylor [Scott & White Charles A.] Sammons Cancer Center [in] Dallas. I get the histology and the grade of the tumor. Sometimes, if they have enough tissue, they’ll do MSI testing, and sometimes [I’ll get estrogen receptor (ER) and progesterone receptor (PR) testing]. Usually, we don’t get [testing for] HER2 or anything else [until the final] pathology.
COLEMAN: Right, so that’s routine. You don’t have to call your pathologist to do MSI testing for endometrial [cancer]?
KOON: No.
COLEMAN: Dr Oh, is it the same [in your practice]?
OH: I’m in general oncology at Texas Oncology-Presbyterian [Cancer Center Dallas]. I get referrals from multiple practitioners, so we get a hodgepodge of pathology reports, but we generally just get the grade and histology, and we may or may not have ER/PR testing when we first see these patients. For example, if I’m doing a dilation and curettage for a patient when I’m suspicious of cancer, I ask for ER/PR testing, and I ask [the pathologist whether] they have enough to check for MSI and mismatch repair [MMR] gene products.
COLEMAN: Yes. I probably asked this out of order, but I think for most of us who are getting endometrial biopsy, [we] just want to know what the diagnosis is, right? When I talk about this to pathologists [who] are outside the United States, [they say] they get very limited information as part of the routine pathology report. But I’ve seen in the United States, over time—now that we’ve got availability of immune checkpoint inhibitors—more and more of the endometrioid adenocarcinomas are coming in with MSI status already done, and I didn’t have to ask for it. It’s variable [for] hormone receptors.
I was surprised to see [hormone receptor testing] wasn’t part of a standard panel in this case; the patient only got ER testing. I think many of us would be looking at PR, as well, because of the opportunities for endocrine therapy.
The next [thing to consider] is whether you recommend any genetic counseling. I think for those of us [who] were getting MSI testing, we’d want to rule out Lynch syndrome. I don’t know [whether] you have genetic counselors easily available to you, or this is something you do yourself.
MALIREDDY: We have a couple of nurse practitioners who do the genetic counseling and testing; so yes, for most of the patients with endometrial cancer, we do [testing]. The patients don’t have to be advanced stage or anything. I do genetic counseling even with the early stages.
CASE UPDATE
Notable molecular features in this patient included MSI stability, MMR proficiency, and HER2 and ER negativity. Postoperative radiotherapy included vaginal cuff brachytherapy to a dose of 21 Gy in 3 fractions. Fourteen months after completing radiotherapy, the patient presented with new right lower extremity edema and right hydroureter. There was no evidence of distant metastases on radiologic imaging.
Carboplatin/paclitaxel chemotherapy was initiated, and treatment was well tolerated. Four months after initiation, there was no evidence of disease on PET scan, with complete resolution of symptoms.
Twelve months later, disease relapse was documented on routine follow-up, with metastases to paraaortic lymph nodes and lung. The patient reported a chronic cough that she attributed to allergies. Bronchoscopy with biopsy revealed endometrial carcinoma cells, and the patient received lenvatinib (Lenvima) plus pembrolizumab (Keytruda).
DISCUSSION QUESTIONS
- Do you have experience using lenvatinib in endometrial cancer or any other tumor type?
- What are your reactions to the KEYNOTE-775 (NCT03517449) data?
- How will you counsel patients regarding this regimen?
- What is your impression of the safety/tolerability of this regimen?
COLEMAN: I assume most of you have used this regimen. For those of you who have, tell me your horror stories. What has been your experience with it?
AGARWAL: It has been well tolerated. I had to reduce the dose of lenvatinib a couple times. [For one] patient, after 1 year, I stopped lenvatinib, and he is [now] just on pembrolizumab.
WANG: In my experience, lenvatinib is harder [to tolerate] than pembrolizumab.
AGARWAL: I agree.
WANG: For all my patients on lenvatinib, I have to dose reduce [because of] fatigue, high blood pressure, [and] weight loss. So now, I’m not starting at 20 mg; I’m scared [of] 20 mg. I usually start with the low dose, approximately 14 mg, and see [whether] they can tolerate that, and maybe go up a little later. Cytopenia is also a problem.
AGARWAL: Yes, I do 14-mg or 10-mg [doses].
MALIK: I had a patient whom I put on lenvatinib. Similarly, she was having a lot of fatigue and decreased appetite, so I had to dose reduce her [treatment]. Overall, she tolerated it well and her disease responded well, but I did have to make some dose modifications for her.
Thrombocytopenia was another issue with her because she was heavily pretreated with carboplatin. She also had blood clots, and I remember she was on anticoagulation [medication], so monitoring her platelets was tricky.
SOLANKI: I was surprised the 20-mg dose was chosen [in the KEYNOTE-775 study].1 There was already experience with renal cell carcinoma that even an 18-mg starting dose was too much, and there was already a discussion about starting at 14 mg and escalating it as tolerated, so I was quite surprised 20 mg was chosen. Do you know why that was chosen?
COLEMAN: In the manuscript, there is a section where they say they used data—not from endometrial cancer but from other tumor types—that [showed that] the lower starting dose was associated with a lower response rate.1
They recognized that dose modification is necessary, but they still recommended—in discussion with the FDA—that because of the potential decrease in efficacy for the regimen [when] starting at a dose lower than 20 mg in [patients with] endometrial cancer, they should start at 20 mg and then [dose reduce]. However, I think many [providers]— myself included—have experienced exactly what you just described and have tried to make this a more tolerable regimen by doing some dose modifications either ahead of time or after the first cycle.
SOLANKI: We went through this with regorafenib [Stivarga] in colon [cancer]. The recommended dose was never tolerated until Mayo Clinic did a study of what they call step-up dosing, then it worked out very well. I’m always surprised. How do they decide what is the right dose for targeted therapy, like we do for chemotherapy?
COLEMAN: It’s an excellent question, and it’s getting a lot of press these days, because the FDA has requested that new drug applications come in with data that support the dose that they moved from the phase 1/2 space into the phase 3 space. [In this case], this is the regimen that was used in the phase 2 space and was felt to be, quote, “tolerable,” and that’s how it got moved into the phase 3 space.
The target engagement is tough to document in a regimen like this, but that’s what the FDA wanted. If this was done today, the FDA would have required them to do 2 dose levels to determine whether the toxicity that was observed at those 2 dose levels was associated with the same efficacy. If it was, then they would take the lower of the 2 doses. That’s the strategy that’s now required. That wasn’t the case when this [study] first got done. It’s an excellent question, [though]. I think we’re getting more precise about dosing [after] the phase 2 setting, but that’s basically how this got set up.
KOON: I’m curious, what do you do? Do you start patients at a lower dose? Do you start them at 20 mg and dose reduce? Or do you do it on a case-by-case basis, based on [the ECOG status] or what you feel is better?
COLEMAN: To be honest with you, I try hard to be a purist with respect to clinical trials, because I always have felt that if we deviated from the way the eligibility was listed in the trial, it would be hard to expect the outcome we got from the trial. I try hard, but I would be lying if I said I always did it, because when I see a frail patient coming in or somebody who didn’t tolerate chemotherapy well, I don’t want to hurt them so that they never come back for cycle 2. So I do just as you said, I [use] some judgment there.
DISCUSSION QUESTIONS
- If you have a patient who is responding to the combination of lenvatinib plus pembrolizumab, how likely are you to continue using both drugs?
- How do you manage immune-related AEs?
COLEMAN: This drug comes in 4-mg and 10-mg capsules, so we can do some dose modifications. I heard [some of you say you use] 14 mg and 10 mg as starting doses. The general schema [is to start at 20 mg, then to dose reduce to 14 mg, 10 mg, and finally 8 mg]. Remember [it is important to] educate the patient ahead of time, to get them through the regimen with good education, then to pay attention to their [adverse] effects [AEs] so you can make rapid dose modifications. Such modifications will happen in two-thirds of your patients. But I do believe there is some discretion on your part, because you know your patient the best, regarding what you think might be tolerable.2
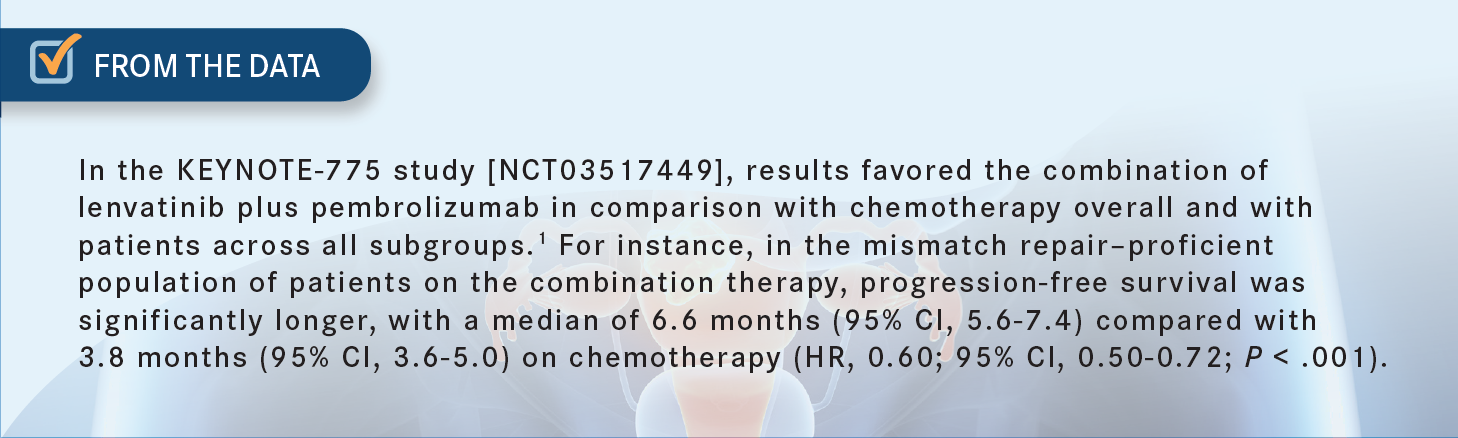
In the KEYNOTE-775 study, only approximately 10% of the patients made it past 2 years without progressing [From the Data1]. For the most part, we’re treating these patients to progression on the regimen, and most of those patients are progressing during their therapy. The question that comes up—and I’d be curious to hear what you think about it—is whether you have to keep both drugs going. We’ve already heard about a patient treated for 12 months, then stopped the lenvatinib and just continued the pembrolizumab.
MALIREDDY: It all depends on the toxicity the patient is tolerating. If they’re really tolerating the drug combination at a low dose, especially lenvatinib, I would tend to keep both drugs going.
But one [AE] I had with lenvatinib was hypertension. I had to stop the drug and get the blood pressure under control, then go to the next level. So, before I start any of these combinations, if the patient has a tough agent and an easy agent to take and they’re still getting the benefit from the infusional agent, I push them to try a little bit of the tougher agent as well. If they can’t tolerate it through the treatments, then at least they’re getting benefit from 1 agent. That’s my approach here.
COLEMAN: Right. I would say most physicians struggle to keep patients on lenvatinib for 2 years. It’s just a tough drug. And I agree, I think the hypertension we see here is different from what we see with bevacizumab [Avastin]. It’s much more difficult to control, but I think with dose modification and all the [other] things you do, we can get to a happy place to try to get the patients the most benefit.
The thing I always keep in the back of my mind, if I know the patient is MMR proficient, is that the likelihood they’re going to respond to single-agent pembrolizumab is pretty low. It’s [approximately] 15%, the same as with chemotherapy. But you do what you can do, and under the protocol, you can give it [for] up to 2 years per indication.3 If the patient is benefiting, they’re benefiting.
I have 1 question, especially for the medical oncologists who give a lot of immune checkpoint inhibitors outside gynecological [cancers]: How comfortable are you with restarting an immune checkpoint inhibitor—in this case, with pembrolizumab—if the patient has had an immune-related AE? What has been your experience with that? For example, [let’s say] it’s colitis.
WANG: If it’s colitis, I usually just emphasize that the patient [should] call us as soon as they start having diarrhea. Usually, if I start the prednisone early to get that under control ahead of time, I don’t really have problems restarting them after tapering down the prednisone to 20 mg, 10 mg, or lower. I just hold the pembrolizumab usually for 1 dose and restart it maybe 6 weeks later, trying to avoid having the patient end up in the hospital. That can be hard.
COLEMAN: Right. How do you know that the toxicity—[in this instance, the gastrointestinal toxicity]—is coming from pembrolizumab vs lenvatinib? Because lenvatinib can cause the same toxicity.
WANG: I know; that was the question initially. I asked other experts, [and] I don’t know. [My approach is] just to blast it with the steroids and maybe hold the pembrolizumab. If the patient responds, then I know [the toxicity is] from [the pembrolizumab]. If they continue to have diarrhea, I know it’s probably from the lenvatinib.
COLEMAN: Yes, but at least with lenvatinib, [because] it’s being given every day orally, it’s easy to stop that and see whether we see resolution. With a short half-life, it should clear the system [quickly]. The immune therapy is an antibody, so it’s there [for a longer time]. And you’re right, the character of the diarrhea is different and more problematic for management.
REFERENCES
1. Makker V, Colombo N, Casado Herráez A, et al; Study 309–KEYNOTE-775 Investigators. Lenvatinib plus pembrolizumab for advanced endometrial cancer. N Engl J Med. 2022;386(5):437-448. doi:10.1056/NEJMoa2108330
2. Lenvima. Prescribing information. Eisai Inc; 2022. Accessed October 31, 2022. https://bit.ly/3ib2Ap3
3. Keytruda. Prescribing information. Merck Sharpe & Dohme Corp; 2022. Accessed November 1, 2022. https://bit.ly/3CmP4FH