Awan Discusses the Growing Use of BTK Inhibitors in CLL
Farrukh Awan, MD
Professor Department of Internal Medicine
Harold C. Simmons Comprehensive Cancer Center
UT Southwestern Medical Center Dallas, TX

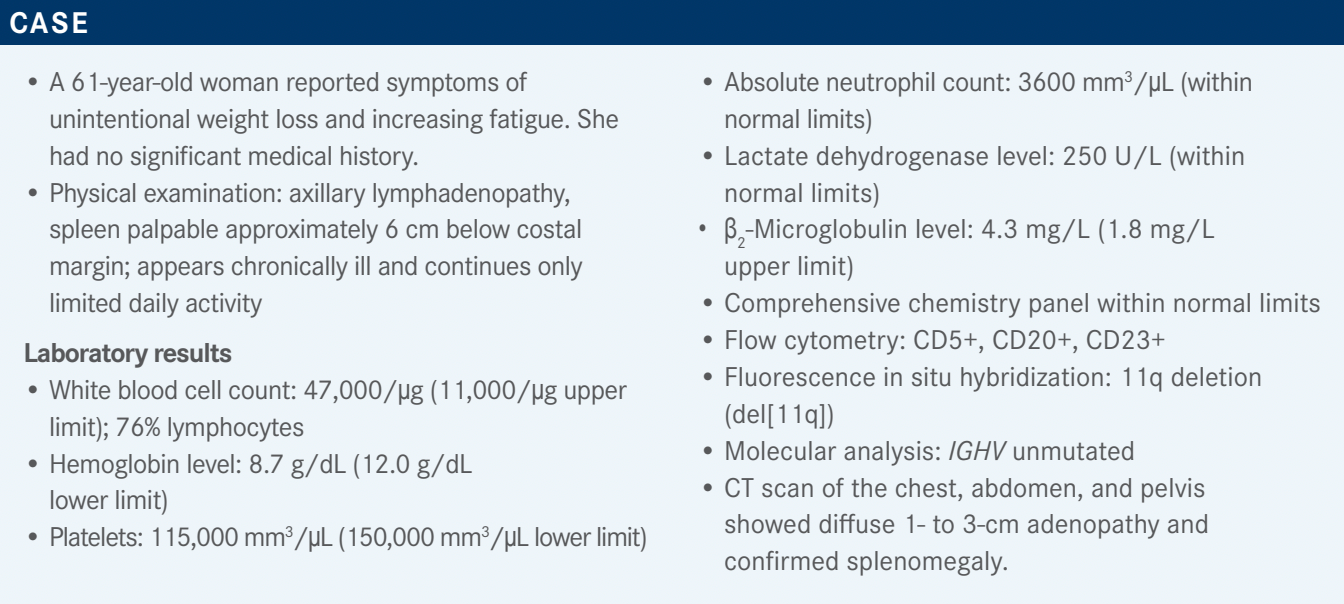
Targeted OncologyTM: What are the Bruton tyrosine kinase (BTK) inhibitors used in frontline treatment of patients with chronic lymphocytic leukemia (CLL)?
AWAN: The first major study with ibrutinib [Imbruvica] was the RESONATE-2 study [NCT01722487].1,2 Ibrutinib was the major breakthrough in the CLL arena as the first effective targeted therapy. Ibrutinib was compared with chlorambucil [Leukeran] in patients with treatment-naïve CLL who were [older] and would not have been considered candidates for chemotherapy.
We have 7- to 8-year follow-up data now, which show consistently that patients who are on ibrutinib do fine with a progression-free survival [PFS] of 59% vs 9% of those without [HR, 0.154; 95% CI, 0.108-0.220].3 There’s initial drop-off, but then it plateaus. So essentially, if you’re going to stop ibrutinib, you will stop ibrutinib within the first 2 years of therapy. Once you get beyond the first couple of years, you tend to do well. Most of those patients can tolerate ibrutinib fine and do well and have good longterm outcomes.
In terms of safety, when compared with chlorambucil, it’s not a fair comparison.1,4 Initially, we saw that it’s a drug that’s well tolerated, has no major issues, but maybe there is a signal of AFib [atrial fibrillation]. This is a classic example of how our thinking has evolved; how we start paying attention to different adverse events [AEs] from the first trial to now in the real world. If you look at the RESONATE study outcomes, the incidence of AFib, even in an older patient population, was not that high. It was less than 10%.
Hypertension was less than 15%. Bleeding [was] nothing, really, which looked pretty impressive back then. But we know that this is not how the real world performs, especially if you have somebody [older than] 70 years. Discontinuation rates from ibrutinib back then were around 10%, so this was a major advance.
What is the evidence supporting acalabrutinib in CLL?
Fortunately, right on the heels of ibrutinib, came acalabrutinib [Calquence]. Acalabrutinib was an option for patients who, for whatever reason, could not take ibrutinib. And some of those patients got on acalabrutinib before they got on ibrutinib.
This was an important development in the field. Eventually, acalabrutinib had the definitive ELEVATE-TN study [NCT02475681] in a treatment-naïve patient population, which compared acalabrutinib plus obinutuzumab [Gazyva] with acalabrutinib by itself and with obinutuzumab plus chlorambucil [in a 1:1:1 randomization].5 It was a similar population to the RESONATE-2 population: elderly patients who would not automatically be considered candidates for conventional chemotherapy. Basically, these patients were not considered candidates for BR [bendamustine, rituximab (Rituxan)] or FCR [fludarabine, cyclophosphamide, rituximab]. So those 70-plus years old, classic, stratified; and those 65 and older with comorbid conditions also were included in this analysis.
Why combine acalabrutinib with obinutuzumab?
When these studies were being done, there was some thought that adding CD20 antibodies to BTK inhibitors would improve outcomes. That’s why some of the earlier studies with ibrutinib included rituximab. There were other studies done that showed that the addition of rituximab didn’t improve the outcomes with ibrutinib. That’s why we stopped adding rituximab.
But then the other question was, “Is it because of rituximab?” Maybe if we use a more effective CD20 antibody, maybe if the dose density is higher than rituximab, maybe you can get a better outcome. So this study was important because it was answering all of those questions, but the main comparison was acalabrutinib vs the standard of care at that point—which I don’t think anybody would consider the standard of care now.
What were the efficacy results of ELEVATE-TN?
The median follow-up is pretty long now, more than 4 or 5 years out.6 Basically, acalabrutinib plus obinutuzumab was the best, followed by acalabrutinib alone. No surprise that it’s better than obinutuzumab plus chlorambucil. This difference [in PFS] is more than 10% with acalabrutinib plus obinutuzumab vs acalabrutinib alone [HR, 0.51; 95% CI, 0.31- 0.81; P = .0259].
The study was not designed to detect that difference, so that’s why you can’t say that it was significant or not, but a 10% to 12% difference is an impressive difference, especially after 5 years of follow-up. The problem with this was this was also happening around the COVID-19 era, so a lot of [clinicians] were not using CD20 antibodies because of the theoretically higher risk of having issues with COVID-19 infection. So that’s why I don’t think that it’s used a lot. But this is, again, provocative, and we can always argue that maybe the addition of a CD20 antibody to acalabrutinib can result in better outcomes.
How does a patient’s IGHV mutation status impact their results?
There’s always this argument that patients with the IGHV mutation will do well with FCR chemotherapy….Those data are out there, and ibrutinib is better than FCR even in patients who are IGHV mutated.7 In the overall cohort, there’s improvement in survival with ibrutinib as compared with FCR. There’s little argument to be made, unless somebody is adamant that they want to use FCR. If you look at the outcomes at 5, 6, 7 years out for IGHV-mutated patients with these novel agents, it is impressive.8 Mutation status doesn’t matter. With or without a mutation in IGHV, outcomes are excellent with these agents, and that’s the take-home message here.
What were the other notable efficacy outcomes in this trial?
For overall survival [OS] outcomes, it’s pretty close, but there’s a trend.5,6 It’s hard to demonstrate improvement in OS in patients with CLL; all of these patients will do well because they will go from one to the other therapies. But the acalabrutinib [plus obinutuzumab] vs the chlorambucil arm, that was statistically significant [HR, 0.55; 95% CI, 0.30-0.99; P = .0474]. There is improvement in survival, but it was also interesting that the acalabrutinib plus obinutuzumab arm was the best. The study wasn’t designed to compare the 2 acalabrutinib arms, but acalabrutinib was categorically better than obinutuzumab plus chlorambucil, so that resulted in it finally demonstrating a survival advantage. It’s getting hard to demonstrate a survival advantage because patients with CLL are doing so well. That’s why this was impressive and also reassuring—5 or 6 years out, your patients are doing well. The vast majority of these patients are alive and have excellent disease control.
For all of these agents: ibrutinib, acalabrutinib, and zanubrutinib [Brukinsa]—2 are approved and 1 is in the approval process—there’s no doubt that these drugs are effective. The issue right now is all about AEs. If you have a drug that’s 10% vs 8% vs 5%, which one will you start off with if the efficacy is the same? If you’re going to get the same outcome in terms of effectiveness, you would want to go with the easiest one, even if it’s a 5% difference.
What AEs were notable in ELEVATE-TN?
If you look at the important ones: atrial fibrillation at 6%…and bleeding issues have consistently been 30% to 50% with BTK inhibitors.5,6,9 By the way, I feel that bleeding is a class effect rather than a drug effect. I think [a patient receiving] the BTK class will have bleeding issues. We also have [approximately] 9% to 10% with hypertension, so we do see the classic AEs. It appears that it might be better than what we have seen with ibrutinib.
There are 2 ways to compare these outcomes. One is you can compare them head-to-head. That would be the ideal way, but you can also look at cross-trial comparisons. The acalabrutinib trials are looking pretty clean, and the ibrutinib trials didn’t look that bad. But in the real-world population…you have a huge number of patients who have these outcomes, because they have multiple comorbid conditions.
They’re much sicker than an ordinary patient on a clinical trial. You would have a lot of these problems in those patients. Regardless, [there are] impressive results with BTK inhibitors—specifically acalabrutinib in the ELEVATE-TN study, a modest incidence of the bad AEs.5 Bleeding [risk] was mostly minor and major bleeding risk was less than 10%.
Can you discuss zanubrutinib for CLL?
The SEQUOIA [NCT03336333] data results are out already.10 Zanubrutinib was compared with BR—even more reason to get rid of chemotherapy now. This was an important study of untreated patients without deletion of 17p [del(17p)], frontline treatment with BR and zanubrutinib vs BR. It was an important trial that was recently presented and we’ll continue to have updates from this, with longer follow-up.
There’s clearly a better [outcome] with zanubrutinib compared with BR.10 If there’s a unique situation in which patients absolutely cannot get these targeted therapies, you might be able to make an argument for using some sort of chemotherapy. But as a standard of care, I don’t feel that there’s any reason to use chemotherapy for CLL. I cannot think of a situation where you would use chemotherapy now. SEQUOIA [data are] still early, so we only have a couple of years of follow-up data. With longer follow-up, we will see a similar curve like we’ve seen with BR and other chemotherapy studies.
The subset analysis is not what I would pay attention to because the follow-up is not significant, even for the ECOG in the Alliance study [NCT01886872].11 We have to wait 3 years [or longer] to start seeing differences in different subsets because the numbers are small. Hopefully, this PFS will manifest itself in subgroup analyses with longer follow-up, but, at this point, it’s looking promising overall.10
Response rate is also better with these targeted therapies. If you’re asking if ibrutinib, acalabrutinib, or zanubrutinib are not as effective in terms of response rate compared with chemotherapy, and you want to get the response faster, the answer is “absolutely not.” Their median time to response for all of these is less than 2 months, which is what you would see with chemotherapy: 1 to 2 months, at least a few weeks before the chemotherapy decreases the counts. You’ll get the same thing [with these therapies]; you will get better lymph node responses. You may not have white blood cell count decreases, but a lot of times, a high white count is not that big a deal. It’s mostly lymphadenopathy and splenomegaly. In terms of response rate, in terms of disease control rates, in terms of OS—multiple studies have shown the same thing, against FCR, BR, chlorambucil.
We don’t have a lot of follow-up yet, but if you’re looking at those important items, such as AFib, ventricular arrythmias, bleeding or bruising, you don’t see a ton of that with zanubrutinib.10 At first glance, these are encouraging data, much cleaner than what we have seen with BTK inhibitors in the past. But we have to be a little bit more cautious because we’ve been through this before. Early results from clinical trials are always better, but then in the real world, we start using the drug and we see a lot more adverse outcomes.
If you break it down and look at the specifics, even if it’s in a few patients, one of the things that you do see with zanubrutinib is neutropenia, which is more prominent [with the] BTK inhibitors.10 We see a little bit of neutropenia, which is more pronounced with the use of zanubrutinib as compared with other things we have used in the past. If you look at AFib rates, [they are] around less than 5%, and then you scratch your head and wonder, “This is an older patient population typically, CLL is generally an older patient disease—what’s the population background of atrial fibrillation?” And you’re looking at approximately 1% to 3% [having atrial fibrillation] as they get older, above age 70.10
So are we almost at the population baseline? I don’t think so. It’s still higher than the population baseline, but it’s pretty impressive that you’re looking at low single digits with zanubrutinib. Bleeding, again I feel, is a class effect. I think all BTK inhibitors will have bleeding issues, and you will continue to have that problem. Fortunately, major bleeding is not that common. The vast majority are bruises and petechiae, but not major life-threatening bleeds, fortunately…. Hypertension and bleeding, in my mind, are class effects. AFib varies by drug a bit because of specificity. Anemia, thrombocytopenia, headaches, arthralgias, diarrhea; there’s always some variation between one and the other drugs.10
REFERENCES 1. Burger JA, Tedeschi A, Barr PM, et al; RESONATE-2 Investigators. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373(25):2425-2437. doi:10.1056/NEJMoa1509388
2. Burger JA, Barr PM, Robak T, et al. Long-term efficacy and safety of first-line ibrutinib treatment for patients with CLL/SLL: 5 years of follow-up from the phase 3 RESONATE-2 study. Leukemia. 2020;34(3):787-798. doi:10.1038/s41375-019-0602-x
3. Barr PM, Owen C, Robak T, et al. Up to 8-year follow-up from RESONATE-2: firstline ibrutinib treatment for patients with chronic lymphocytic leukemia. Blood Adv. 2022;6(11):3440-3450. doi:10.1182/bloodadvances.2021006434
4. Imbruvica. Prescribing information. Pharmacyclics; 2022. Accessed October 13, 2022. https://bit.ly/3Rmm7Qo
5. Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib with or without obinutuzumab vs chlorambucil and obinutuzumab for treatment-naive chronic lymphocytic leukaemia (ELEVATE TN): a randomised, controlled, phase 3 trial. Lancet. 2020;395(10232):1278- 1291. doi:10.1016/S0140-6736(20)30262-2
6. Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib ± obinutuzumab vs obinutuzumab+chlorambucil in treatment-naïve chronic lymphocytic leukemia: five-year follow-up of ELEVATE-TN. J Clin Oncol. 2022;40(suppl 16):7539. doi:10.1200/ JCO.2022.40.16_suppl.7539
7. Fakhri B, Andreadis C. The role of acalabrutinib in adults with chronic lymphocytic leukemia. Ther Adv Hematol. 2021;12:2040620721990553. doi:10.1177/2040620721990553
8. Sharman JP, Egyed M, Jurczak W, et al. Efficacy and safety in a 4-year follow-up of the ELEVATE-TN study comparing acalabrutinib with or without obinutuzumab vs obinutuzumab plus chlorambucil in treatment-naïve chronic lymphocytic leukemia. Leukemia. 2022;36(4):1171-1175. doi:10.1038/s41375-021-01485-x
9. Calquence. Prescribing information. AstraZeneca; 2019. Accessed October 13, 2022. https://bit.ly/3DwEuN8
10. Tam CS, Brown JR, Kahl BS, et al. Zanubrutinib vs bendamustine and rituximab in untreated chronic lymphocytic leukaemia and small lymphocytic lymphoma (SEQUOIA): a randomised, controlled, phase 3 trial. Lancet Oncol. 2022;23(8):1031-1043. doi:10.1016/S1470-2045(22)00293-5
11. Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens vs chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379(26):2517-2528. doi:10.1056/NEJMoa1812836
