Second-line Options for Patients With Metastatic TNBC
Aditya Bardia, MD, MPH, discussed potential second-line therapies for patients with metastatic triple-negative breast cancer.

Aditya Bardia, MD, MPH
Associate Professor of Medicine
Harvard Medical School
Director of Breast Cancer Research
Massachusetts General Hospital Boston, MA

Targeted OncologyTM: Based on the National Comprehensive Cancer Network (NCCN) guidelines, what is the ideal second-line therapy for metastatic TNBC?
BARDIA: If we look at the NCCN guidelines, sacituzumab govitecan [Trodelvy] has a category 1 recommendation for TNBC and is recommended for hormone receptor [HR]-positive or HER2-negative breast cancer.1
Trastuzumab deruxtecan [Enhertu] is for HER2 IHC 1+ [and] 2+. The label for sacituzumab govitecan is for patients who’ve received at least 1 line of therapy in the metastatic setting, so technically it is for the second-line and later settings. Similarly, for trastuzumab deruxtecan, the label is for patients who’ve received at least 1 prior line of chemotherapy for metastatic disease.
What was the design of the trial that led to the approval of sacituzumab govitecan in the second line and beyond?
The approval of sacituzumab govitecan was based on the phase 3 ASCENT trial [NCT02574455]. This was a trial looking at sacituzumab govitecan vs treatment of physician’s choice [TPC] for patients with metastatic TNBC. The primary end point was progression-free survival [PFS]. The overall survival [OS] was a key secondary end point.2
For background, sacituzumab govitecan is an antibody-drug conjugate [ADC] targeting Trop-2. Trop-2 is overexpressed in TNBC. The idea is that the drug would bind to Trop-2–expressing cells, get internalized, and give the payload to the cancer cells, which would then cause cell death. It also has a bystander effect, so it can impact cells that do not express Trop-2, and if there’s Trop-2 heterogeneity in the tumor, it can impact Trop-2– negative cells because of this bystander effect.
Please describe the efficacy in the ASCENT study.
There was an impressive improvement in both PFS and OS, a doubling of PFS and OS from 6 months to 12 months, which is clinically meaningful and…significant as well. This resulted in the FDA approval of sacituzumab govitecan for pretreated metastatic TNBC, and the approval was in the second-line and plus setting.3
Generally, when we see results that are this significant, we would expect all the subgroups to derive benefit, and this is exactly what was seen in all the subgroups, including patients who did not have an initial diagnosis of TNBC. This is something we see in clinical practice—patients who have HR-positive breast cancer to begin with in the metastatic setting can become HR-negative.
That’s why it’s important to repeat the receptors at the time of metastatic diagnosis. Other subgroups, including [those with] prior use of PD-1 or PD-L1 inhibitors, benefited. One would not expect any cross-resistance between pembrolizumab [Keytruda] and sacituzumab govitecan. So whether one [had] prior immunotherapy or not, there was benefit.2 In terms of response rates, the majority of the tumors had some reduction compared with TPC. Eribulin [Halaven] and capecitabine had some reduction but not that much. The response rate was higher with sacituzumab govitecan at 35% vs just 5% with standard chemotherapy.2
What did investigators observe in terms of adverse events (AEs) in this trial?
The 3 common AEs seen with this agent include grade 3 and 4 neutropenia; the incidence of febrile neutropenia was not high—[it was] in single digits—but it can be seen. The second is gastrointestinal AEs like diarrhea, as well as nausea. Sacituzumab is considered a moderately emetogenic regimen, so you could use 2 or 3 drugs to prevent nausea. In patients I’m worried about, I generally use 3, so that would include palonosetron, fosaprepitant, and dexamethasone. The third AE is alopecia. In metastatic TNBC, patients often have alopecia to begin with, so that just gets maintained. These are the 3 AEs that I discuss with patients.
The AE profile is largely because of SN-38, the payload that’s attached to this ADC. If one has some experience with irinotecan, it [sacituzumab] has a similar AE profile to it, but the percentage of AEs is lower. For example, with irinotecan, the grade 3 diarrhea is about 30%, and with sacituzumab it’s about 10%.2 So while the AE profile is similar, the incidence of individual AEs is lower than what we would expect with irinotecan. The advantage of the ADC is a better toxicity profile compared with chemotherapy.
Did the type of chemotherapy or other factors make a difference to the outcome?
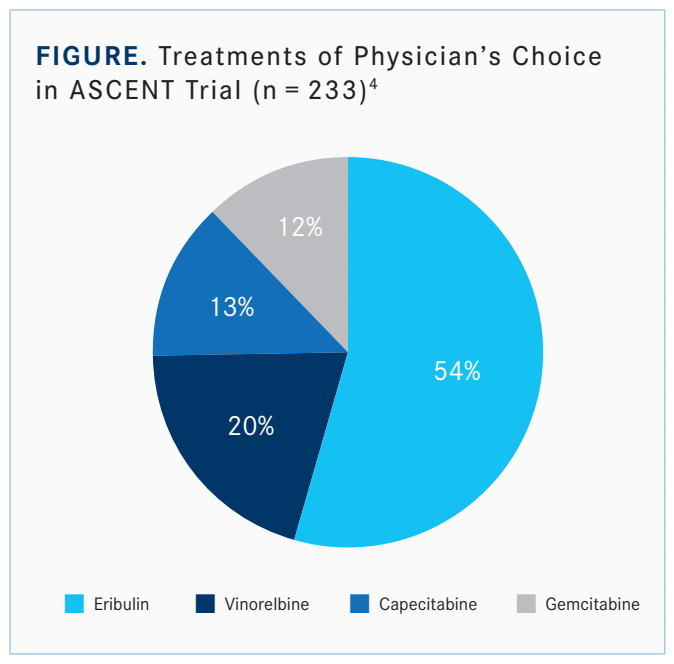
For the chemotherapy, it didn’t matter whether it was eribulin, capecitabine, or vinorelbine [Figure]. Against all the chemotherapy agents, sacituzumab did better, so essentially that’s why it’s used currently in the secondline metastatic TNBC setting.4
The responses based on BRCA in patients who had germline BRCA mutation vs wild type had similar improvements in PFS and OS. It’s not something that necessarily influences response to sacituzumab govitecan. Similarly, with Trop-2, you saw benefit even in the lower Trop-2 group compared with standard chemotherapy, so there’s no clinical utility to monitor Trop-2.5
Age is not a factor related to sacituzumab govitecan. Patients [who were younger] than 65 years and older than 65 had similar benefit. The only thing to consider in a patient who is [somewhat] elderly, say someone in their 70s, is that they generally have a higher incidence of AEs, so you should have a low threshold for dose reduction, bringing the dose down to 8 mg/kg or 7.5 mg/kg. Generally, with dose reduction, you can manage the AEs.6
Which data led to the approval of trastuzumab deruxtecan in the second line and later?
Trastuzumab deruxtecan is another agent in this setting. This was evaluated in the DESTINY-Breast04 [NCT03734029] trial, which looked at metastatic breast cancer that was HER2 low, defined as IHC 1+ [and] 2+ and fluorescence in situ hybridization negative. The trial required patients to have at least 1 prior line of chemotherapy. The primary end point of the trial was PFS in patients who had HR-positive disease. The majority of the patients, about 90%, who enrolled in DESTINY-Breast04 had HR-positive disease, and a small cohort, about 10% of patients, had HR-negative disease. They were also enrolled, but with an exploratory objective, not primary.7
The HR-negative or the so-called TNBC subgroup saw an improvement in both PFS and OS, a doubling of PFS and OS. Again, I would emphasize this was an exploratory subgroup, not the primary. The number of patients who were enrolled in this cohort was 58, which was a small subgroup but the results were quite remarkable.
Due the unmet need in this patient population, the FDA approved trastuzumab in the HR-negative subgroup, which is very different from the ASCENT trial where the primary end point was for patients with TNBC on sacituzumab govitecan vs standard chemotherapy. There was a clear improvement in response rate with trastuzumab compared with standard chemotherapy [for both subgroups].
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Breast cancer, version 4.2022. Accessed January 13, 2023. https://bit.ly/3iFEraf
2. Bardia A, Hurvitz SA, Tolaney SM, et al; ASCENT Trial Investigators. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384(16):1529-1541. doi:10.1056/NEJMoa2028485
3. Bardia A, Tolaney SM, Loirat D, et al. Sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) in patients (pts) with previously treated, metastatic triple-negative breast cancer (mTNBC): final results from the phase 3 ASCENT study. J Clin Oncol. 2022;40(suppl 16):1071.
4. O’Shaughnessy J, Punie K, Oliveira M, et al. Assessment of sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) cohort by agent in the phase 3 ASCENT study of patients (pts) with metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1077. doi:10.1200/JCO.2021.39.15_suppl.1077
5. Bardia A, Tolaney SM, Punie K, et al. Biomarker analyses in the phase III ASCENT study of sacituzumab govitecan versus chemotherapy in patients with metastatic triple-negative breast cancer. Ann Oncol. 2021;32(9):1148-1156. doi:10.1016/j.annonc.2021.06.002
6. Kalinsky K, Oliveira M, Traina TA, et al. Outcomes in patients (pts) aged ≥ 65 years in the phase 3 ASCENT study of sacituzumab govitecan (SG) in metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1011. doi:10.1200/JCO.2021.39.15_suppl.1011
7. Modi S, Jacot W, Yamashita T, et al; DESTINY-Breast04 Trial Investigators. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387(1):9-20. doi:10.1056/ NEJMoa2203690