Roundtable Discussion: McKay Examines Second- and Third-Line Therapy for Metastatic RCC
During a Targeted Oncology case-based roundtable event, Rana R. McKay, MD, discussed the case of a patient who progressed following treatment with axitinib and pembrolizumab for clear cell renal cell carcinoma.

Rana R. McKay, MD (Moderator)
Associate Professor of Medicine
UC San Diego Health
San Diego, CA


MCKAY: Before we dive into what we would do next, we could speak a little bit to this person’s course of first-line therapy, doing axitinib/pembrolizumab. I do not know if this patient has a similar path to what you all have experienced with toxicity management in the first-line setting and the use of the IO/VEGF-TKI [immuno-oncology/vascular endothelial growth factor–tyrosine kinase inhibitor]. Does anyone have any [experience] to compare there?
SWEET: I tend to have more trouble with the TKIs and frequently have had… to hold the TKI and continue the IO.
DEKKER: I generally have the same issue. The problem with TKI/IO is more cutaneous toxicities, managed with topical steroids.
MCKAY: Yes, not to say that toxicity is inevitable, but there is a very high rate of toxicity with VEGF-TKIs. They work well and patients can be on them for a long time. The longer somebody is on them, it is just a greater opportunity for them to have an adverse event [AE]. And I agree, the chronicity of the TKI can sometimes cause some significant toxicity.
With the pneumonitis, in the context of asymptomatic pneumonitis that is just detected on imaging, a lot of times I do not stop therapy. I would continue treatment if the patient is completely asymptomatic and has grade 1 pneumonitis that would essentially be asymptomatic on imaging. But this patient was clearly symptomatic, and the right thing to do was to start steroids.
MCKAY: What are the factors that you take into account as you are making a decision about second-line therapy?
SWEET: Every bullet point listed is relevant. The challenge would be if I have a sense that, as in this patient, the disease is progressing more rapidly, could I go to a nivolumab/ipilimumab [Opdivo/Yervoy] regimen? I have some concerns with the prior pneumonitis.
MOON: Do you rechallenge? Because for me, personally, it has been kind of shaky. I get scared about [AEs] that land you in the hospital. I have had a couple of pancreatitis or big, serious endocrine [toxicities] that I [felt I would] have a hard time rechallenging. Pneumonitis sometimes is a little bit different. I am curious what [others] all do. Would you give ipilimumab/nivolumab knowing that he had a rough time with pembrolizumab?
SASTE: If he had that much pneumonitis, I would be afraid. Because, as you said, I have had trouble with the ipilimumab/nivolumab combination myself in patients with melanoma. I actually lost one to pancreatitis. It was so bad. I just couldn’t do anything. So it is just that experience itself. If they have any -itis grade 3 or above, which takes a while, and the patient has issues tolerating the medication, then I would have issues using IO/IO again.
MCKAY: Anybody else have anything to share about their toxicity? I think, for me, it is all about what toxicity they had and how severe it was. Sometimes with the endocrine toxicity, for example, they can get symptomatic. When they are hyperthyroid initially as you start them on treatment and they are having a lot of trouble, but then…get out of that and are hypothyroid and…on [hormone] replacement, they are fine. That is when you just rechallenge them. So I think it all depends on what they have. If it is colitis, sometimes we get a little bit leery. But I am certainly interested to hear how you all manage that.
And also how you manage the TKI. With this patient it was pneumonitis, so it was easy. But in the context of diarrhea, where a large number of patients are going to get diarrhea, do you all do something different?
CHO: I agree. With a rash or even colitis or a thyroid problem, I think about rechallenging. But with pneumonitis and hepatitis, I do not usually rechallenge it.
TAI: I like to rechallenge at least once because it is probably one of the few treatments we have that we can give long-term; I hate to give up at the first sign of trouble. I had a lot of experience treating this in the metastatic lung cancer setting. That is even more complicated because many [patients] are already short of breath to begin with. So somehow I went from one to the other.
SUPERFIN: I think it depends on what -itis you have. Pneumonitis is the scariest, or encephalitis. If you have colitis and you did not get to infliximab [Remicade], you can still rechallenge. But if the patient required something like infliximab, I have apprehension. It also depends on how many options you have left. Are you at the end? Do you have a lot of options left? And how important is the immunotherapy option for this particular cancer—can you go without it? I think that is what usually goes into the decision. Obviously for grade 4 AEs, I usually do not, but for grade 3, it depends on which grade 3 AE it is.
CHAUDHARY: I had a patient I rechallenged for hepatitis. It was grade 1. I treated them with steroids and then rechallenged; had no problem. And then I had a patient who developed pemphigoid cutaneous toxicity that occupied more than 50% of her skin surface, and I could not rechallenge. So I think it depends on the severity.
MCKAY: I completely agree.
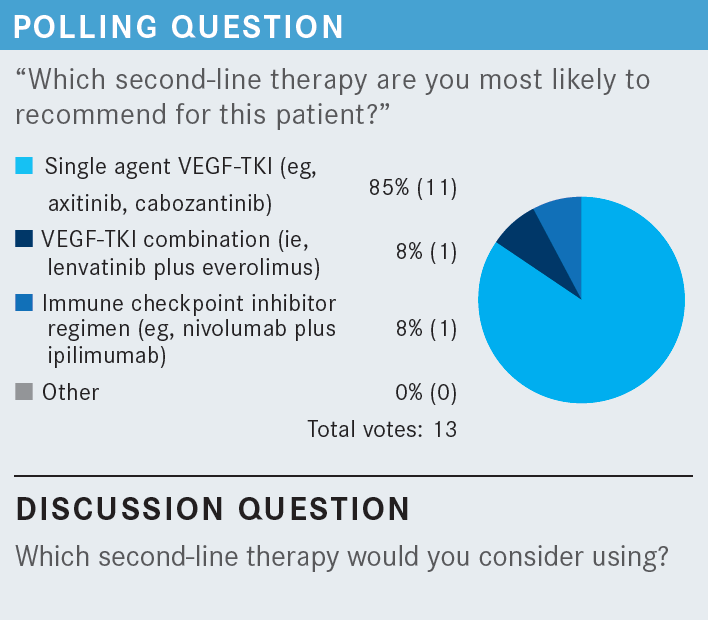
MCKAY: This patient experienced toxicity from IO, seemed to tolerate the axitinib OK, had favorable-risk disease, and ultimately progressed. Sites of metastases at the time of progression are lymph node and bone. As you are thinking about teeing up the next-line therapy, what is running through your mind? What are the options that you are thinking about?
RASILA: Cabozantinib [Cabometyx] would be my choice.
DEKKER: Yes, cabozantinib would be good.
SWEET: I agree.
MCKAY: What makes you all choose cabozantinib?
TAI: It is very well tolerated, and I have had good success with it in the last few patients. So I like to use it.
MCKAY: Would anybody consider lenvatinib/everolimus [Lenvima/Afinitor] in this scenario?
DEKKER: Yes, it could be an option; it would depend how symptomatic the patient is.
CHAUDHARY: Correct me if I am wrong, but the mTOR pathway is not a big pathway in RCC, right?
MCKAY: It is. I think VEGF and mTOR are the 2 key pathways. The data for lenvatinib/everolimus in the second-line space are driven from a phase 1/2 study [NCT01136733] of around 150 patients.1 It is a different regimen and a different toxicity vs the single agent. I think the doublets can sometimes be a little bit more challenging.
Say this patient did not have the pneumonitis—would anybody continue the immunotherapy and add something to it? If this patient did not have pneumonitis and they are progressing on pembrolizumab/axitinib, would you keep the pembrolizumab going and add lenvatinib?
SWEET: The other consideration, a bit out of the box, would be to stop the pembrolizumab and convert to ipilimumab/ nivolumab, as a second-line dual IO therapy.
SUPERFIN: Do you think adding ipilimumab, if you have already come through the failure, would have any additional benefit? In most of the cancer cases, if you fail pembrolizumab, adding ipilimumab does not make a big difference.
DEKKER: Adding ipilimumab may make a difference if it fights T-cell exhaustion.
MCKAY: There are certainly not level 1 data [supporting this]....There are some patients that I think we can salvage with ipilimumab, but it is certainly not the majority.
MCKAY: What are your goals of therapy as you go into the third line, and what are the different factors that influence clinical decision-making in the third-line setting for you all?
TAI: I think at this point it is all palliation, so symptom relief is probably the No. 1 goal. If there are some physiological issues that are affecting the patient that you can maybe reverse, that would be definitely worth it. Certainly progression-free survival is a third one, but that is less clear.
CHAND: I agree with this. By the time patients get to third-line treatment, the question is how much they can tolerate. A lot of times they get very symptomatic from the disease burden, especially the ones that are very fast progressors. So it is good to use a treatment that has a rather good toxicity profile because it may be hard to use a TKI, with too many AEs. It does get very difficult to treat beyond the second-line setting because of so many factors that tend to build over lines of treatment.
MCKAY: We have talked a lot about quality of life and… palliation of symptoms. What are your thoughts about response and the need for immediate response? Does that factor in?
DEKKER: For me it is, at this point, do I believe the patient is going to respond or not? Or am I trying to treat the patient, who is not yet ready to transition, to comfort her? In this situation, medication that is likely to cause the least toxicity would be the most preferred. And even though it fell out of favor, with single-agent bevacizumab [Avastin], I have seen some interesting responses even after multiple TKIs. So that could be an option in this situation, but it comes down to how much the oncologist believes that this patient actually could be helped.
MCKAY: It is interesting. How many of you all in your practice are actually giving third-line therapy? Do you have a lot of patients that will see third, fourth, or fifth line with RCC?
DEKKER: Two-thirds.
CHAUDHARY: I have had patients who still had decent performance status, especially younger patients, and you are wondering [whether they] should be referred to a tertiary center for a trial. A few patients are actually still clinically OK.
MCKAY: I hear you. This is an interesting patient because this one started out as favorable risk. Sometimes these patients with favorable risk can actually go on to see so many different lines of therapy.
MCKAY: How do you all determine progression in these patients? What is the threshold for you to actually switch therapy? Do you use stereotactic body radiation or other things like that if there is some oligoprogression or some mixed progression and just continue to push along? This patient only got 4 months on cabozantinib. How do you determine progression and the right time to switch? And do you use these other modalities?
CHAUDHARY: I have continued beyond progression and addressed the progressive side. I have had a patient with the sarcomatoid variant of RCC. Initially I thought he was not going to do well, but he did well with the ipilimumab/nivolumab combination and follow-up. I did cherry-picking for almost 6 to 7 months and then switched treatment when he started having constitutional symptoms or weight loss, and I thought at that time he was progressing.
ZHOU: I have a similar patient. It depends on the imaging and also patient symptoms. But if I isolate a lung mass, you could just watch it grow even a little bit; you can do the stereotactic radiation.
SWEET: I find I have to look beyond the radiologist’s reading, which suggests that everything is significant. When you look at the images with the patient, you see these little ditzel 1- to 2-mm changes that lack some correlation and then you stick with the program.
MCKAY: Yes. So how do you all handle the brain? Do you treat beyond progression in the brain? How frequently do you do brain imaging?
TAI: Usually I only do it if symptoms are present.
DEKKER: I do it at diagnosis and symptoms.
SUPERFIN: I think I agree with at diagnosis and symptoms.
MCKAY: Do you do it at times of therapy change? If you are going to switch somebody, do you just scan them just to make sure beforehand?
SWEET: I do not.
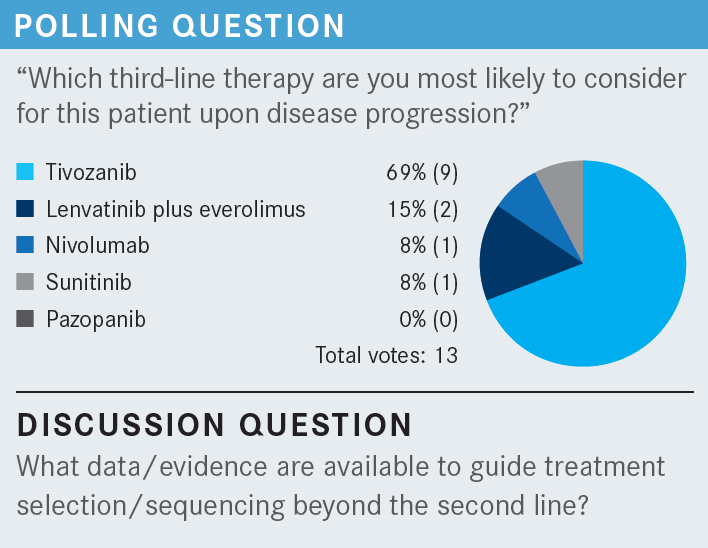
TAI: I would like to see some trials where patients have had multiple lines of treatment and still had a response. That is probably the only reason to choose one over the other.
MCKAY: Yes, I definitely think we are in a data-free zone. Our frontline therapy advancements have outpaced our second-line therapy options. We are lacking level 1 evidence for what to do in the second or third line, as our front line is changing. And it is going to change even more with adjuvant therapy.
MCKAY: What are your thoughts [on] the tivozanib data on efficacy, response, and toxicity [in the TIVO-3 trial (NCT02627963)]. Does something resonate with you about these data?
CHO: I have to say tivozanib is a very tolerable TKI [From the Data2].
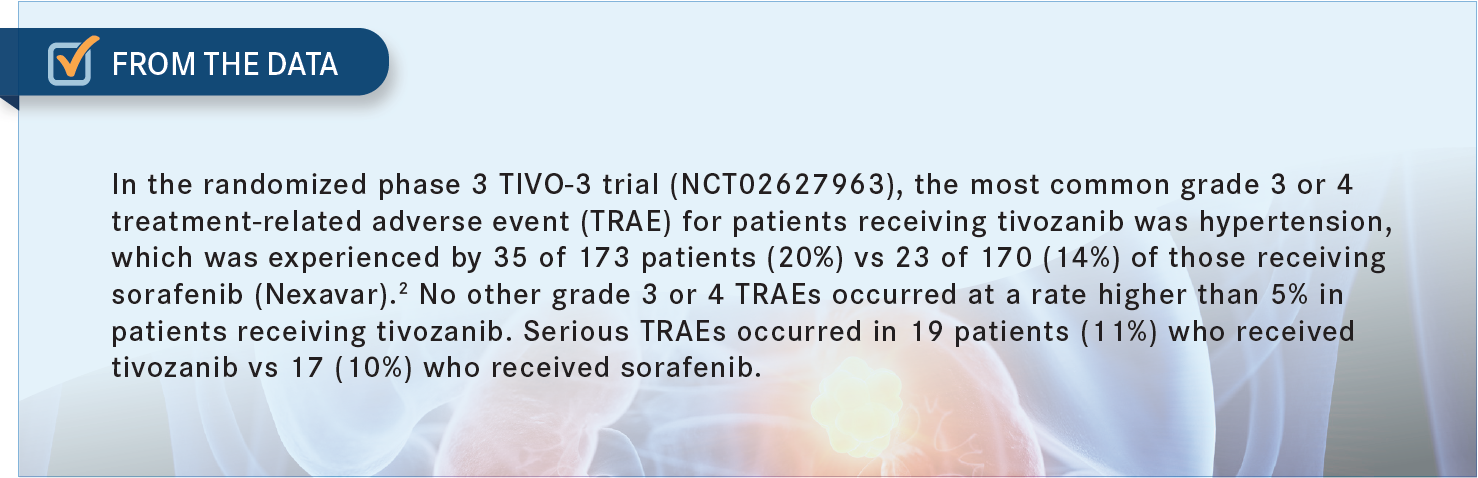
SASTE: My impression is that it is definitely better tolerated. The toxicities [such as] hypertension you can easily manage. Rash and hand-foot syndrome are the 2 challenging ones with the TKIs, although a dose [reduction] or giving the patient breaks in between the treatments is something that can also be managed. But the tivozanib data are definitely much better than [those of] the lenvatinib/everolimus combination.
FARJAMI: I echo the same experience. [Tivozanib] is definitely better tolerated and has better positive patient experience in the third-line setting.
MCKAY: Have you all modified the schedule, where you keep the dose the same but, instead of doing a 7-day hold every month, do 2 weeks on, 1 week off? Or instead of reducing the dose, do you modify that at all or stick to what is on the label?
SASTE: Personally, I have not used it, but if I were to adjust, the first thing I would do is the dose adjustment. If that is not helping, then I will go with the scheduling of 7 days on, 7 days off or 2 weeks on, 1 week off.
TAI: I am curious, were there any patients who had cabozantinib plus nivolumab before they switched to this drug? Because most of us probably would be using combination IO plus TKI of some kind as a first- [and] second-line treatment. This is a new [treatment]. And [if they] continued the IO, [and] there was no toxicity and substituted for the cabozantinib, that is probably the most likely scenario where it is actually being used.
MCKAY: I think the patients that went on this trial, probably a fair [number] did receive prior cabozantinib; as I said, prior sunitinib [Sutent] and pazopanib [Votrient] were used.2 There are safety data of tivozanib with nivolumab. There is…a phase 3 study that is going to be launched, which is currently in the process of accruing, of tivozanib plus nivolumab vs tivozanib alone [NCT04987203]. But there are safety data for the combination of tivozanib with nivolumab.
MOON: Yes, I think there is a trial that is going to just answer exactly Dr Tai’s question, which is: In the event of an IO combination or IO monotherapy regression, does the idea of keeping the IO going [make sense or would it] make a difference? Because we do not know. No data [currently are available], and data [need] to be acquired.
MCKAY: Well, let’s keep moving. What do you see as the value of a positive phase 3 clinical trial, such as TIVO-3 in the third line? Do these data sway you? I think when we look at the lenvatinib/everolimus data, they are based on a 150-patient phase 2 trial.1 Here we have level 1 evidence with a several-hundred-patient phase 3 trial supporting the use of tivozanib.2 Does the level of evidence sway you, and is that a factor you think about when selecting a therapy? Or at this stage in the game, does that not matter for you?
DEKKER: I will say it this way: Data are data…so you are probably doing something for a few patients. It is probably better than nothing, but it is no game changer and probably would not sway me one way or another vs something more tolerable.
TAI: I think these are only level 1 data because the sorafenib [Nexavar] is the control group. None of us, probably, would use some sorafenib in the third line. I was involved in the very first clinical trial with sorafenib, and my impression was that patients progress fairly quickly.
So it is probably not a very effective agent to begin with. Yes, compared with sorafenib, this is much better. But is it much better compared with more modern treatment? That remains to be seen, right? I think that is where the problem is. So I am not that impressed with the data because the control group is too weak.
MCKAY: I would ask you: In the third-line setting, post IO, post 1 or 2 VEGF agents, what would you compare [tivozanib] with? What would you pick as the comparator in a patient who has seen cabozantinib or has seen sunitinib?
TAI: I would like to see the comparison directly [with] cabozantinib plus IO and see how those patients responded to this as a single agent. I am sure we do not have the data to do it, but I would like to see that.
DEKKER: I would probably want to see temsirolimus [Torisel]. I had a lot of success with that agent in the third line.
REFERENCES
1. Motzer RJ, Hutson TE, Glen H, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16(15):1473-1482. doi:10.1016/ S1470-2045(15)00290-9
2. Rini BI, Pal SK, Escudier BJ, et al. Tivozanib versus sorafenib in patients with advanced renal cell carcinoma (TIVO-3): a phase 3, multicentre, randomised, controlled, open-label study. Lancet Oncol. 2020;21(1):95-104. doi:10.1016/ S1470-2045(19)30735-1

Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen











