Clinical Commentary: How Immunotherapy Is Used for Treatment of Patients with ES-SCLC and NSCLC
At a live virtual event, Devika Das, MD, discussed the use of immunotherapy for patients with extensive stage-small cell lung cancer (ES-SCLC) and for patients with non–small cell lung cancer.
Devika Das, MD
Clinical Assistant Professor
University of Alabama at Birmingham Medicine
Birmingham, Alabama

Results of the IMpower133 Trial
The approval for [atezolizumab in patients with ES-SCLC] came from the phase 3 IMpower133 [NCT02763579] clinical trial that looked at patients with ES-SCLC with a good performance status of 0 or 1.1 None of the patients had prior systemic therapy, and it’s important to know that patients were treated and those with asymptomatic brain metastases were eligible for this study.2 They were also stratified by gender, performance status, and the presence or absence of brain metastases.
The 2 arms of the trial were randomized in a 1:1 fashion, and the first arm got induction of 4 cycles and 21-day cycles with atezolizumab/carboplatin and etoposide [EP]. Then, the placebo arm got only carboplatin/etoposide and a placebo. After the 4 cycles, they were on maintenance atezolizumab vs placebo, and they were treated until there was still progression of disease or loss of clinical benefit. The coprimary end points for this study were overall survival [OS] and progression-free survival [PFS], and some of the other secondary objectives they looked at were response rate, duration of response, and safety.
When looking at the PFS at 6 months and at 12 months, in both of those time frames [if you look at patients given] atezolizumab compared with placebo, the PFS rate was better at 30.9% vs 22% and 12.6% vs 5.4%, respectively. Clearly, that response had gone down at 12 months, but it’s still there and there was sustained benefit in the treatment arm. Then, in terms of OS: Remember that in SCLC there have been so many studies, and we’ve not seen a drug since platinum-etoposide that has shown an OS benefit like this.3 So this was the first study [to do that in some time], and because of that, it got the approval even though that number is very small.
The median OS in the atezolizumab arm was 12.3 months vs 10.3 months in the placebo and standard-of-care arm. Again, I think that’s going to be interesting and something that we’re all going to be looking for long term. Is this survival benefit durable? Is this something that’s going to last? Is this going to be a group of patients where this benefit will last for years? And that would be ultimately how we’ll pick a drug, in terms of using immunotherapy in the long run.
Subgroup Analysis of IMpower133
If you look at the [patient subgroups on this trial], if you pay attention to the female patient population, it seemed like the females derived a little bit more benefit in using the immunotherapy.3 Not much difference was seen between patient’s age, and there was not much benefit difference with the performance status groups. However, [the difference is OS for] patients with brain metastases was very disappointing [Table3].
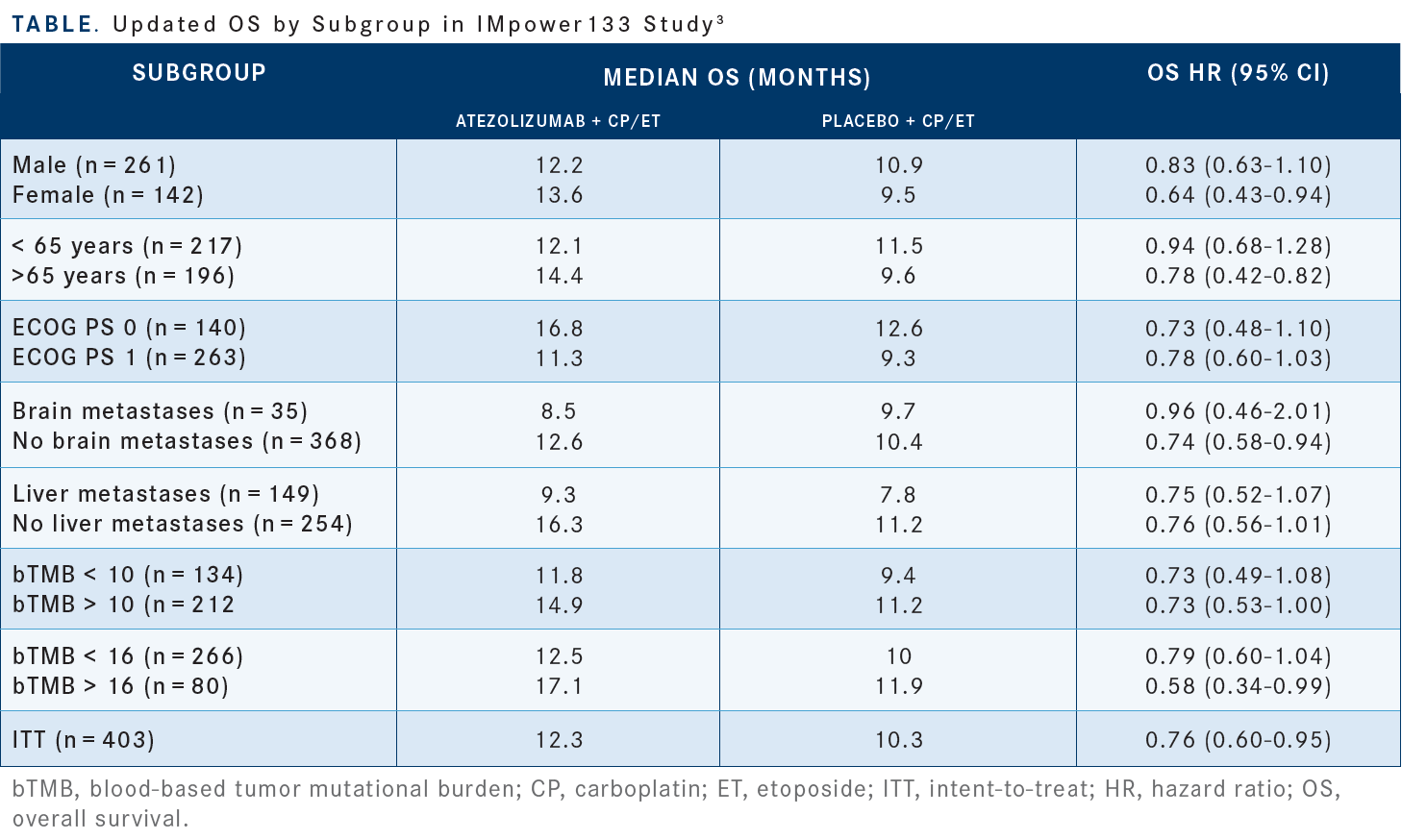
Again, this is sort of a practical challenge of finding that population of patients with treated or asymptomatic brain metastases. It was a small number of patients, as just 35 patients were looked at, but [the data show] it almost looks like there was no benefit or it was detrimental in giving immunotherapy to these patients. Again, if you look at the liver metastases, patients without the liver metastases did better. There are some data that checked the tumor mutation burden [TMB], and the higher TMB that tumors had, those patients did better, but again, this is not a large number and is not validated, so we don’t test that for patients in SCLC.
In summarizing the IMpower133 data, if you look at the atezolizumab vs the placebo group, confirmed objective response rates [ORRs] were seen more in the placebo group compared with the atezolizumab group, in 121 patients [60.2%] vs 130 patients [64.4%], respectively.4 However, 5 patients in the atezolizumab arm had complete responses [CRs] compared with 2 patients in the placebo group. Partial responses [PRs] were seen more in the placebo group [with 128 patients (63.4%) compared with 116 patients (57.7%) in the atezolizumab arm].
What’s impressive with the immunotherapy is the patients who responded and who had ongoing responses at 2 years of follow-up with 11 patients (9.1%) vs 3 patients (2.3%) in the placebo arm having an ongoing response at a 2-year follow-up. So, who is the best sort of patient who responds well [to this treatment]? I don’t think we understand, but if you give this to the right patient and if we have the right biomarker, there is a potential of some patients having durable responses, but I just don’t think we know how to pick them out right now.
Something that is concerning is the adverse events [AEs] seen in this trial, because we’re dealing with a population of patients who come in quite sick, and immunotherapy, as much as patients like the chemotherapy-free option, is not without its own toxicities. Grade 1, grade 3, and grade 5 AEs were comparable in both arms, but more [patients in the atezolizumab arm had grade 1 and 2 AEs compared with the placebo group], at about 36.9% vs 34% in the arm that got placebo alone.
Durvalumab’s Role in ES-SCLC
The CASPIAN study [NCT03043872], which led to the FDA approval for the durvalumab combination, was a phase 3 study that included treatment-naive patients with a performance status of 0 or 1.5 This study also permitted the entry of patients with asymptomatic or treated and stable brain metastases. They had to have a life expectancy of more than 12 weeks as determined by the investigators and had to have measurable disease. This was a slightly more complicated study with 3 arms, but I’m not going to focus on the arm that had dual checkpoint inhibition, but the arm that had durvalumab plus EP vs EP alone.6
A difference here is the EP was permitted up to 6 cycles in this study, whereas in the other study they restricted it to 4 cycles only. Moreover, in this study, researchers permitted the use of both cisplatin and carboplatin and the previous study went with carboplatin alone. The primary end point was OS with secondary end points being PFS, ORR, safety, and then patient-related outcomes.
In terms of median OS, the arm treated with durvalumab was 12.9 months vs 10.5 months in the EP-alone arm, which was not much different than what we saw with the atezolizumab data, with a hazard ratio [HR] of 0.71 [95% CI, 0.60-0.86; P = .0003].7 What’s impressive here [is that there is still survival] at 36 months, so the [long-term response] is what I’m interested most in both studies and to see how many patients are alive [at that time frame]. They're the data that I think we’re going to focus on long term: how many of those patients have OS benefit.
Breaking down these results by subgroups, just like in the previous study, there was not much difference between the patients’ age, but the younger patients tended to do better with an HR of 0.68 (95% CI, 0.54-0.87) vs 0.78 (95% CI, 0.59-1.04), respectively. There was not much difference with the use of the platinum, carboplatin vs cisplatin, as they both seemed to derive benefit. Again, in this study, the female patients seemed to derive more benefit than the males, and performance status was a similar result. [Results for patients with] brain metastases were still disappointing, as only 55 patients had the presence of brain metastases, but there was not a lot of benefit derived in that population compared with those without, at an HR of 0.76 (95% CI, 0.43- 1.33) vs 0.71 (95% CI, 0.59-0.86).
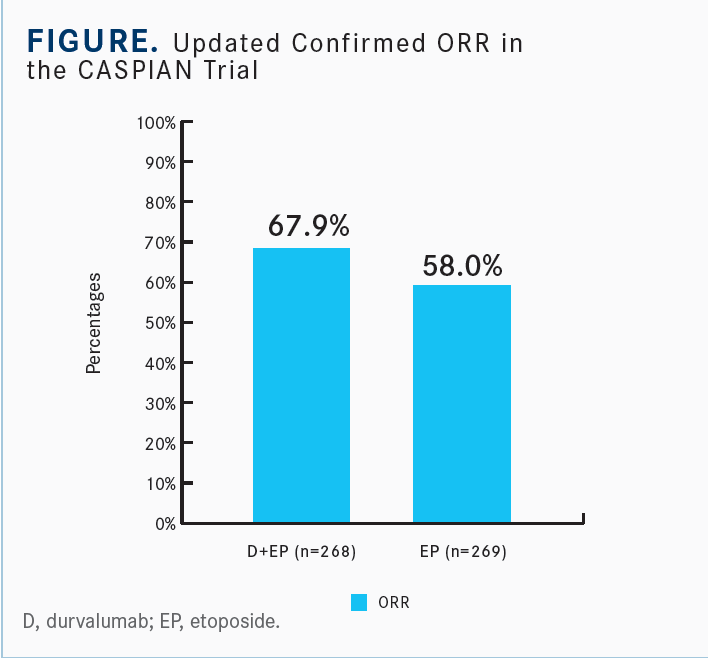
The landmark PFS rates at 6 months, 12 months, 18 months, and 24 months favored adding immunotherapy to treatment vs without over time [at 45.4% vs 45.8%, 17.9% vs 5.3%, 13.9% vs 3.4%, and 11% vs 2.9%, respectively].8 [Moreover, the median PFS was 5.1 months in the durvalumab plus EP arm and 5.4 months in the EP alone arm (HR, 0.80; 95% CI, 0.66-0.96)]. In terms of the ORR, this is a little bit better with the durvalumab compared with data seen with atezolizumab.9 This was slightly better in the durvalumab population than in the previous study with atezolizumab.
Maintaining Benefit of Treatment Over Toxicities
In terms of AEs, lots of AEs were seen in both arms. There were about 6 deaths in the durvalumab arm vs 2 in the EP arm, so honing in on the point that this is not significantly higher toxicity than chemotherapy alone, but there is still a significant amount of toxicity every time you add a new drug. Therefore, you need to make the decision if that hinders the quality of life, is it worth going through that, and what is the right patient who should be exposed to an additional drug just to improve the quality of life and PFS?
Then what’s important, while there were AEs on both the studies, when looking at immune-related AEs, those were only 20% in the CASPIAN study vs 41% in the IMpower133 trial.
Again, in terms of practical use, the atezolizumab study had carboplatin, and in the durvalumab you could use cisplatin or carboplatin if you’re sticking purely to the study design and then how these drugs are available. I think it’s important to note with durvalumab that if the patient is significantly underweight, which I don’t think most of us treat anybody that’s less than 30 kgs, there is a dose difference.
Testing for Frontline Treatment in NSCLC
The National Comprehensive Cancer network [NCCN] recommendation for frontline molecular testing for NSCLC includes EGFR, ALK, KRAS, ROS1, BRAF, NTRK, METex14 skipping mutations, and RET.10 Then the testing should be considered as a part of broad molecular testing, so this is not something that’s a special test anymore; this is standard of care, along with then getting PD-L1 testing. I think getting that up front rather than doing sequential single-gene testing and then sending in NGS when they progress [is better], because by then you run out of tissue, so you have to rebiopsy patients. It’s helpful, and it seems that most practices have put that into their workflow to send that and get that information up front.
Again, reiterating that NCCN does recommend that all clinicians obtain molecular testing for actionable biomarkers before administering checkpoint inhibition. So that is actually an NCCN recommendation, to not give immunotherapy before you have the molecular testing back. So even if the PD-L1 is very high, they may or may not have responses to the checkpoint inhibition, which is why having that information before you start a patient on immunotherapy is critical.
For patients with PD-L1 expression of more than 1% with a targetable driver oncogene, the frontline therapy is the targeted therapy for that oncogene and not checkpoint inhibition. The first-line preferred NCCN recommendation is to use osimertinib [Tagrisso] up front, even though there are other approved tyrosine kinase inhibitors [TKIs]. I think that’s in practice based on what I’m hearing, everybody is using that up front.
In some of the treatment guidelines for patients who have PD-L1–positive disease but have also an EGFR mutation, the NCCN says there’s contraindication for treatment with PD-1/PD-L1 inhibitors that may include documented autoimmune disease, current use of immunosuppressive agents, and the presence of an oncogene like an EGFR exon 19 deletion, or L858R, or ALK rearrangement that would predict lack of benefit.
Similarly, for second line, at that point, you could use a PD-L1 inhibitor, but they prefer using chemotherapy before the use of single-agent pembrolizumab [Keytruda]. So [guidelines suggest], as much as possible, doing directed TKI, chemotherapy, and then immunotherapy as the last option for these patients who have oncogene-driven tumors.
Relevant Data in NSCLC
A phase 2 study of pembrolizumab before a TKI for EGFR-positive, PD-L1–positive non–small cell lung cancer wanted to enroll about 25 patients who were TKI naive with EGFR-positive disease, had positive PD-L1, and got up-front pembrolizumab at 200 mg every 3 weeks, with overall response rate as the end point.11
After 11 patients were approved, they saw they had to discontinue the trial because of lack of efficacy. About 73% of those patients had PD-L1 of more than 50%, and 1 of those 11 patients had an objective response but then was found to not have had an EGFR mutation. There were 2 deaths within 6 months of enrollment, including 1 attributed to pneumonitis. So toxicities occurred down the line when they were given TKI, so there is a big concern. There’s a signal about concern about sequencing PD-L1 inhibitors and TKIs in patients that have EGFR-positive disease.
The current evidence says we really should not be using those drugs before a TKI, even for patients with high PD-L1 expression, at least based on some of the small studies that were seen. They then looked at the development of severe irAE [immune-related adverse events] for patients on a PD-L1 blockade followed by osimertinib, and found that about 15% of those patients had severe immune-related AEs.12
The median time of onset was about 20 days after they started the osimertinib, they all required steroids, and most of them were hospitalized. In looking at the PD-L1 blockade followed by erlotinib [Tarceva], they did not see the same thing, with EGFR TKI followed by PD-L1 blockade, they also did not see the same thing in this particular study. Then they broke it down by how many days were patients on immunotherapy, what was the time interval between the immunotherapy and osimertinib, and then time to toxicity.
I think most of the toxicity happens within the first 30 days or so, but 1 patient was on pembrolizumab for a while, with the interval between the immunotherapy and osimertinib close to a year, but the patient still had toxicities within 15 days of starting osimertinib. This is, again, not a very large number of patients, but I think the signal is concerning enough in terms of how to best sequence these drugs. So, as much as possible, what NCCN recommends is we don’t use immune checkpoint inhibition in this population. Another meta-analysis that looked at 5 trials with about 3000 patients who received nivolumab [Opdivo], pembrolizumab, atezolizumab, docetaxel, with the EGFR status, data were available for about 2200 of those patients.13
Overall, OS for patients on an immune checkpoint inhibitor vs docetaxel had a hazard ratio of 0.69 [95% CI, 0.63-0.75; P < .001]. Then, the patients with EGFR wild-type disease had an OS hazard ratio of 0.67 [95% CI, 0.60-.075; P < .001], but those who had EGFR-mutated disease did not do well [HR, 1.11; 95% CI, 0.80-1.53; P = .54]; they did worse if they were getting immune checkpoint inhibition.
The conclusion from this meta-analysis was that compared with docetaxel, checkpoint inhibitions were associated with higher significantly prolonged OS in the second-line setting. However, the lack of OS benefit in the EGFR-mutated patients suggested that checkpoint inhibition should be considered only after all other effective therapies have been exhausted.
REFERENCES
1. FDA approves atezolizumab for extensive-stage small cell lung cancer. News release. FDA. March 3, 2019. Accessed June 30, 2022. https://bit.ly/2Jkowds
2. Horn L, Mansfield AS, Szczęsna A, IMpower133 study Group, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220-2229. doi:10.1056/NEJMoa1809064
3. Liu SV, Reck M, Mansfield AS, et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J Clin Oncol. 2021;39(6):619-630. doi:10.1200/JCO.20.01055
4. Reck M, Liu S, Mansfield AS, et al. IMpower133: updated overall survival (OS) analysis of first-line (1L) atezolizumab (atezo) + carboplatin + etoposide in extensive-stage SCLC (ES-SCLC). Ann Oncol. 2019;30(suppl 5):v710-v717. doi:10.1093/annonc/mdz264
5. FDA approves durvalumab for extensive-stage small cell lung cancer. News release. FDA. March 30, 2020. Accessed June 30, 2022. https://bit.ly/3I5AjZp
6. Paz-Ares L, Dvorkin M, Chen Y, et al; CASPIAN Investigators. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929- 1939. doi:10.1016/S0140-6736(19)32222-6
7. Paz-Ares L, Chen Y, Reinmuth N, et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer: 3-year overall survival update from CASPIAN. ESMO Open. 2022;7(2):100408. doi:10.1016/j.esmoop.2022.100408
8. Goldman JW, Dvorkin M, Chen Y, et al; CASPIAN Investigators. Durvalumab, with or without tremelimumab, plus platinum-etoposide versus platinum-etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2021;22(1):51-65. doi:10.1016/S1470-2045(20)30539-8
9. Paz-Ares L, Dvorkin M, Chen Y, et al. Durvalumab ± tremelimumab + platinum-etoposide in first-line extensive-stage SCLC (ES-SCLC): Updated results from the phase III CASPIAN study. J Clin Oncol. 2020;38(suppl 15):9002. doi:10.1200/JCO.2020.38.15_suppl.9002
10. Ettinger DS, Wood DE, Aisner DL, et al. NCCN guidelines insights: non-small cell lung cancer, version 2.2021. J Natl Compr Canc Netw. 2021;19(3):254-266. doi:10.6004/jnccn.2021.0013
11. Lisberg A, Cummings A, Goldman JW, et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1+, tyrosine kinase inhibitor naive patients with advanced NSCLC. J Thorac Oncol. 2018;13(8):1138-1145. doi:10.1016/j.jtho.2018.03.035
12. Schoenfeld AJ, Arbour KC, Rizvi H, et al. Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann Oncol. 2019;30(5):839-844. doi:10.1093/ annonc/mdz077
13. Lee CK, Man J, Lord S, et al. Clinical and molecular characteristics associated with survival among patients treated with checkpoint inhibitors for advanced non-small cell lung carcinoma: a systematic review and meta-analysis. JAMA Oncol. 2018 Feb 1;4(2):210-216. doi:10.1001/ jamaoncol.2017.4427
14. FDA approves atezolizumab for extensive-stage small cell lung cancer. News release. March 3, 2019. Accessed June 30, 2022. https://bit.ly/2Jkowds

















