CASE UPDATE
CAR T-cell therapy was discussed as an option, but the patient declined due to distance to nearest transplant center.
During a Targeted Oncology case-based roundtable event, Dipenkumar Modi, MD, and participants discussed the leading later-line therapy options for patients with diffuse large B-cell lymphoma.
Dipenkumar Modi, MD (Moderator)
Hematology/Oncology
Bone Marrow & Stem Cell Transplant Program
Barbara Ann Karmanos Cancer Institute
Detroit, MI


MODI: What factors play a role when selecting subsequent lines of therapy for relapsed DLBCL?
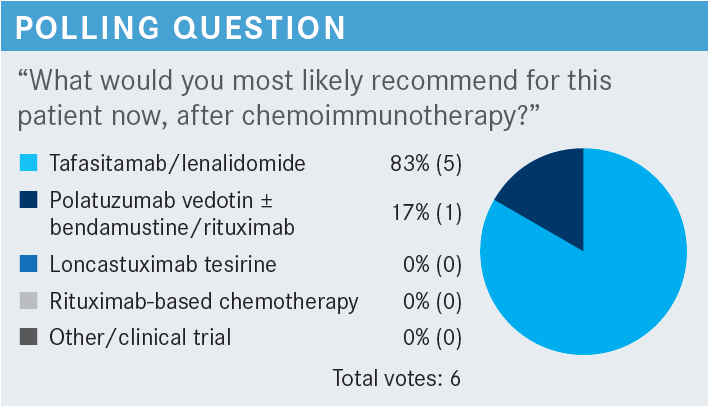
GOLDMAN: I think all these [factors] come into play, and this gentleman being 79 years old and not transplant eligible narrows down the options. And he’s already failed 2 lines of therapy. I can’t imagine that his performance status [PS] is better after failing second-line therapy than it was after he failed first-line therapy. So, I still think that we’re looking at giving him an active regimen that has a good chance of getting him into remission. The recent data with tafasitamab-cixix [Monjuvi] and lenalidomide [Revlimid] are very robust for patients who are transplant ineligible, and there’s a very high complete response [CR] rate and durable remissions.1
I don’t think that the insurance coverage really matters here, and he’s not going to be eligible for chimeric antigen receptor [CAR] T-cell therapy if he’s not eligible for transplant. So, I think using a CD19-based therapy would be most appropriate for him.
MODI: Would you consider cell of origin when you determine second- or third-line therapy for DLBCL?
GOLDMAN: Yes, maybe, but I don’t think the studies clearly show that it makes a difference, unless you’re using a BTK [Bruton tyrosine kinase] inhibitor. I’m not sure that the studies show that it matters or [that] it is necessary to choose therapy based on that, but I’m interested to hear what you say.
MODI: Well, there are some data that show patients who have non–germinal center B-cell–like (GCB) DLBCL tend to respond better with lenalidomide and rituximab–based combinations. The response rates are higher, more than 50% to 55%, compared with GCB DLBCL. But, yes, outside those settings, I think selection of treatment based on cell of origin usually hasn’t panned out in relapsed/refractory DLBCL settings.
Dr Mattour, what factors matter to you or what factors do you consider when you select the next line of therapy?
MATTOUR: A combination of all the factors listed. Sometimes it’s one thing or another that determines what the patient would like or be able to receive. Top of the list oftentimes are comorbidities, and toxicities of the previous treatment also play a role in determining what the patient would be eligible to receive and even to tolerate.
MODI: So for this patient who has received R-CHOP and R-GemOx, what is your preferred regimen? Would you consider tafasitamab/lenalidomide; polatuzumab vedotin-piiq [Polivy], bendamustine, and [rituximab; (pola-BR)]; or loncastuximab tesirine-lpyl [Zynlonta]?
MATTOUR: Tafasitamab/lenalidomide would be an option. Practically, I’ve had some patients who had good results with polatuzumab. Again, it depends on what we can give a patient and what they would be able to tolerate.
MODI: Do you often have issues with the insurance to obtain a lenalidomide prior authorization compared with pola-BR, which is intravenous and easy to get?
MATTOUR: Not so much. I mean, we do, but in our situation, we have a good support system that oftentimes takes some load off us. But yes, we’ll hear some resistance, but oftentimes it resolves in a timely manner.
MODI: OK. How about if you are thinking to send this patient for CAR T-cell therapy down the line?
MATTOUR: Well, [this patient’s] age—I know it shouldn’t be a factor, but it is. I would consider it, but again it would depend on the patient and how he looks in real life.
CAR T-cell therapy was discussed as an option, but the patient declined due to distance to nearest transplant center.
PATEL: I’m new to all these 3 drugs, but I think loncastuximab sounds a little bit more toxic. But given the fact that some of these patients are very young, they could probably benefit from this, [especially those] who have gone at least over 2 lines of therapy. The other fact is that regardless of CAR T-cell therapy before or after, they had a good response.
MODI: Do you think about any patient characteristics that make you worry about using any of these options, like which patients you think might tolerate loncastuximab better than the other patients?
PATEL: If they are heavily treated, it means their bone marrows are heavily treated, so pancytopenia is common in these patients, isn’t it? So I think younger patients might benefit. When I say younger, maybe in their 60s and less than 70 years, and of course, good-performing patients, at least an ECOG PS of [0 to 2].
DABAK: Yes, for me, if I am sending a patient for CAR T-cell therapy, I would rather stay away from CD19-directed treatments and go with maybe a pola-BR regimen vs the other 2. Sure, loncastuximab can be given before or after and it does not change whether the patients responded to CAR T-cell therapy, but what has always been at the back of the mind is the loss of CD19 after you treat them with these medications and [whether it] will reduce the effectiveness of CAR T-cell therapy.
MODI: Yes, you’re right. There are some data showing that CD19 expression—unlike CD20 expression, which can be mutated or diminished with CD20-targeting agents like rituximab or obinutuzumab [Gazyva]—stays on B lymphocytes or even PB [peripheral blood] lymphocytes.2
One of the likely explanations for CAR T-cell therapy failure is CD19 loss, which is present in about 30% of patients. However, there are also CAR T-cell data [in which] the subgroup analysis showed the patient still responded, even if CD19 was not present at the time of therapy.
So yes, to make your point, as a clinician it always worries me as well whether targeting CD19 might diminish the effectiveness of subsequent CAR T-cell therapy. But some data, again the numbers are very small, show reassuringly that targeting CD19 before CAR T-cell therapy might not do major damage in terms of the response to CAR T-cell therapy.
BLOOM: This is often a quandary that we get into when we have multiple therapies—none of which are perfect—that are all developed in parallel and not tested head-to-head. We have more trouble comparing them because so often for isolated trials, when they eventually are tested head-to-head—if they’re ever tested—the outcomes are sometimes different than what you would expect. When this occurs, we tend to try to select patients based upon what toxicities they can best tolerate.
However, what we would prefer in a situation like this is to have a biologic marker that would suggest that this patient is more likely to respond to this treatment or this patient is more likely to respond to that treatment.
Without one and without a clear winner where toxicities are concerned, it seems to me that what everyone in each center is going to have to do is decide which drug they want to use so that they can become very good at it. I’m sure that each of these drugs requires finesse and experience, and I think you’ll end up doing a better job if you choose 1 drug and use it often than if you have a little bit of experience using each of them.
MODI: You are right, Dr Bloom. I think this is the era we are living in. Each trial has its own inclusion criteria and it’s hard to compare across the trials. We are comparing apples to oranges.
Also, you are right, that it [depends] on what physicians are comfortable with. Looking across the patient population, among these 3 treatment options, one thing I can say is that patients who got loncastuximab were somewhat heavily pretreated, but despite that and failing CAR T-cell therapy or having double-hit or double-expressor lymphomas, they have responded to a single-agent drug with an objective response rate of 48%.2
BLOOM: Yes, but the CR rate was 25%, right?
MODI: Yes, the CR rate was 25%.3
BLOOM: The CR rate for the other 2 drugs, where they weren’t as heavily pretreated, was [about] 40%,1,4 and there’s no way to know whether the difference in those numbers is because of how many previous treatments they got or if it is the quality of the drug [From the Data1,3,4]. There is absolutely no way to know.
MODI: Well, one thing I can say is that there were patients who participated in the tafasitamab trial who were less heavily pretreated, and fewer patients had primary refractory disease. Moreover, prior CAR T-cell therapy and transplant were not allowed.
So I can say that biologically, we were dealing with relapsed DLBCL, but the biology among that patient population might be different from the biology in the loncastuximab cohort. Those patients are having high CR rates but also more durable remissions because probably they are more chemotherapy sensitive.
BLOOM: I have no reason to doubt you, but we don’t know.
MODI: Oh, absolutely, yes. The eventual question comes, do we have head-to-head comparisons? Obviously the answer is no. Are there going to be head-to-head comparisons? Probably not. We are still doing apples to oranges. I totally agree with your statement on it, that, yes, we don’t have that comparison yet.
DABAK: I want to also make a couple of points. If the patients have failed, say, R-CHOP, then they go on to another chemotherapy combination like R-GemOx, R-DHAP [rituximab, dexamethasone, cytarabine, cisplatin] or R-ICE [rituximab, ifosfamide (Ifex), carboplatin, etoposide]. Then they go on to transplant and still relapse, or they cannot go to transplant and they relapse, as we have used rituximab-based chemotherapy as a common theme.
So just thinking logically, it makes more sense to go to a different mechanism of action, which is the CD19- targeting agents, whether it’s tafasitamab/lenalidomide or loncastuximab over pola-BR. You may steer more toward that just for a different mechanism of action. Maybe one would use tafasitamab/lenalidomide over loncastuximab only because a lot of times these patients are still going to relapse no matter what you do, whether you give them the CAR T-cell therapy or not, and they’re probably going to need all drugs one after the other. We have more data showing that loncastuximab can be given before or after, whereas we do not have data showing that tafasitamab/lenalidomide works after 2 to 4 lines of therapy or after loncastuximab. So I may reserve it for a later time if the patient relapses.
MODI: Yes, I also echo your comments. I want to add one more thing: The long-term outcomes of tafasitamab/lenalidomide reported that the earlier you offer this combination in second-line therapy, the better the CR, PFS [progression-free survival], and OS [overall survival] compared with when you offer this as third- or fourth-line therapy.
[This is] because we are dealing with an immunomodulatory agent, lenalidomide, which has some synergy with tafasitamab. So the earlier you offer it in the disease course, probably the better mileage you might get out of this regimen. I agree with you on that statement.
Dr Patel, do you have any comments to add? How do you use these agents in your practice?
PATEL: Basically, we are dependent on a referral system once they progress on first-line therapy. But now that these brand-new agents have come into play, I think we are tempted to go ahead and try [them]. Like it was mentioned, all these 3 agents are going to be tried one after the other regardless. I still think depending on the age, PS, and the number of prior lines of therapy, loncastuximab may be the drug of choice because one can use it before or after CAR T-cell therapy.
As Dr Bloom said, all 3 don’t have head-to-head studies, so we can’t say one is better than the other, and there’s only very little experience with each of them. So I think with hematologic malignancies, we need a little bit more experience with these drugs before I can make a definite decision on which I would really use.
MODI: If you must use any of these agents as a bridge for CAR T-cell therapy, do you have any preference?
AL-JANADI: There’s no preference, and honestly, I agree with you completely and with what everyone has been saying. You made a good comment and disclaimer that we’re just assuming we know what the best choice is, but we’re just depending on small studies, and none of these have a very good long-term or large number, right?
There is going to be, hopefully, some registry trial. I’m not sure if any company is doing any registry outcomes to tell us a little more about that. The hypothetical point about CD19 I would still put at the front of my thoughts, because we have very few patients on loncastuximab who have had treatment and then went on to CAR T-cell therapy. But that could be pure chance, right? It’s a very small number, so I would consider that.
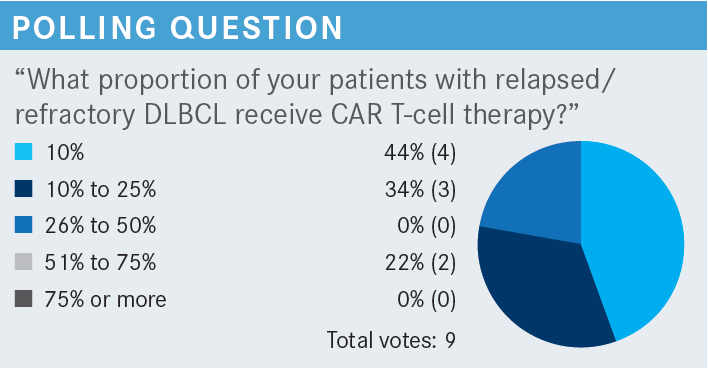
We have a CAR T-cell program [at our center], and we rarely turn down a patient. We have treated in the last 36 months approximately 36 patients—so about an average of 1 patient a month—and the majority of them had DLBCL. Very few patients did not make it [for the CAR T-cell therapy], but of course, it depends on the availability of [whom] we’re seeing. We do use a lot of CAR T cell before any of these antibodies, immediately [after] they fail their second-line therapy.
All patients go to first-line therapy, and when they relapse, they go to second-line therapy with the intention of transplant. If they fail second-line therapy, and probably about 40% of patients still progress, they will move to transplant. Those who respond go to transplant too, and those who relapse after transplant, we still send them for CAR T-cell therapy.
MODI: When they need some bridging or some treatment for the lymphoma when you are waiting for CAR T-cell therapy, do you have any preferred regimen?
AL-JANADI: We don’t direct the doctors on what to do, but I saw a lot of pola-BR being used.
MODI: What is your experience with pola-BR, particularly bendamustine causing lymphopenia?
AL-JANADI: This is only going to be a few cycles anyway, so we don’t necessarily discourage them. We tell them if that’s what you like to use, you could still use it. We have not had failure of the CAR T-cell product.
MODI: I mean in terms of peripheral B-cell collection, have you had any issues when they got bendamustine?
AL-JANADI: That’s what I’m saying, we didn’t have a failure of collecting T cells to send to manufacturing, because they only receive a few cycles of this. Within probably 3, maximum 4, cycles, they’re already ready for their CAR T cells.
REFERENCES
1. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/haematol.2020.275958
2. Thapa B, Caimi PF, Ardeshna KM, et al. CD19 antibody-drug conjugate therapy in DLBCL does not preclude subsequent responses to CD19-directed CAR T-cell therapy. Blood Adv. 2020;4(16):3850-3852. doi:10.1182/bloodadvances.2020002587
3. Caimi PF, Ai W, Alderuccio JP, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):790-800. doi:10.1016/S1470-2045(21)00139-X
4. Sehn LH, Herrera AF, Flowers CR, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020;38(2):155-165. doi:10.1200/ JCO.19.00172
