Roundtable Discussion: Lunning Compares the Benefits and Disadvantages of Using Tafasitamab-Lenalidomide in R/R DLBCL
Matthew A. Lunning, DO began a Case-Based Roundtable event by asking a group of oncologists how diffuse large b-cell lymphoma in handling in their practices. The responses varied, considering some of the oncologists worked in academic centers and some worked in the community setting.
Matthew A. Lunning, DO

Matthew A. Lunning, DO, an assistant professor of the Internal Medicine Division of Oncology & Hematology at the University of Nebraska Medical Center, began a Case-Based Roundtable event by asking a group of oncologists how diffuse large b-cell lymphoma in handling in their practices. The responses varied, considering some of the oncologists worked in academic centers and some worked in the community setting.
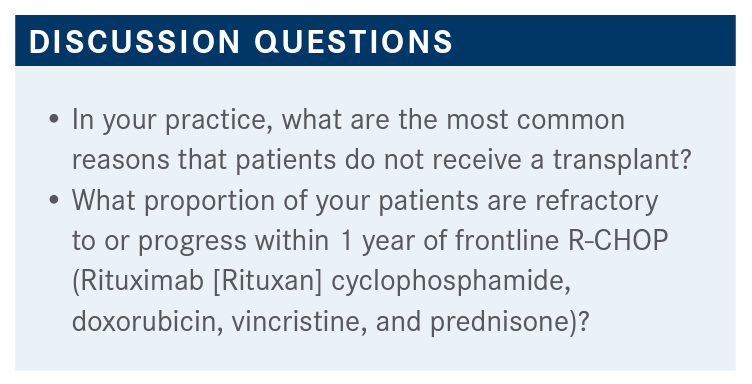
VIJ: I would say it’s physiological age, comorbidities, and performance status that tie into [the decision to with-hold transplant].
NARAJEH: I think the most common reason is that the patient has insensitive disease, and they do not respond to chemotherapy and are deemed to be chemotherapy-resistant.
LUNNING: [Dr Haddadin], what is the most common reason why patients don’t receive transplant at your practice or institution?
HADDADIN: Well, in community oncology, it’s probably going to be because of performance status and comorbidities. If [the patient has] poor performance status and loss of comorbidities, we might not refer them for a trans-plant. These are the major reasons [for withholding trans-plant] in my practice.
LUNNING: You feel comfortable determining the transplant eligibility in a relapse/refractory patient with large cell lymphoma. Is it glaring to you that they’re a clear-cut transplant?
HADDADIN: Yes, recently I had a 76-year-old patient with a bad heart, bad lungs, barely gets out of bed, and he feels like he’s had relapse. He’s not going to be a candidate for anything. But if it’s borderline, I will make a referral to the closest place for us, which is St. Louis, and then ask them to do an evaluation.
LUNNING: So the [patients that are] transplant maybes are being sent to have help with the discussion and the decision. What percentage of patients do you [see in your practice that just go straight to transplant]?
HADDADIN: I will say probably 50/50…depending on the age.
BABLEO: [In my experience, what stops transplant is] mostly age and comorbidities. Our closest facility is about 2.5 hours away and they just didn’t want the transportation to get there, they just didn’t want to go there to even be evaluated for transplant. So access is an issue with me, too.
LUNNING: So logistics and just even getting to the trans-plant center [is a problem], even though they may be [eligible for] a transplant.Any other statements or concerns about sending people to transplant or not getting to transplant that we haven’t heard yet?
NANNEY: One of the concerns is the length of time that [the patient is] away from home with the transplant, and with a lot of older patients they don’t tolerate being in the hospital away from home for a month, which a transplant requires.
LUNNING: Dr Khasawneh, what percentage of your patients are refractory or progress within 1 year of frontline R-CHOP? KHASAWNEH: I would say 10%.
LUNNING: 10%? That’s very good. Anybody else have a different number based upon their area of practice? RAJEH: [About] 40% or 50%, for my practice.
MATTAR: Around a third of the patients progress within 1 year, usually, it’s 50/50 who respond to R-CHOP unless they have high-risk disease, like double-hit or triple-hit [lymphoma]. [For patients with an intermediate risk,] if you’re talking about regular R-CHOP, I would say it’s 50/50 who still progress. About 30% [of those patients] would progress within 1 year and then another 20% in the next year.
LUNNING: [When] you’re looking at the data and looking at some of the prospective trials, we get probably 60% to 70%, depending upon obviously the international prognostic index scores into a metabolic CR, 10 to 15% are your primary refractory or primary progressors. Then you have that population that goes into remission maybe 20% to 30%, I think, that relapses from their disease from that standpoint.
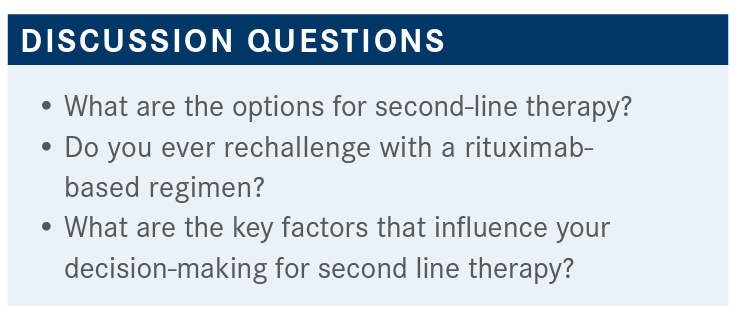
HUESER: It’s based on their performance status, their medical comorbidities, and the patient’s overall protoplasm. A lot of times we have some good tertiary care centers and I get them there since I’m in a small place, if they’re refractory up front and they haven’t done well with first-line chemotherapy. However, hitting patients hard with something in the second line is probably not going to be a very good option. [We look] for something a little bit on the softer side, especially for our older patients and especially for patients that live 100 miles plus away, to try to limit the coming back and forth or access. That would influence how we proceed with what the next line would be.
LUNNING: Whatever you’re giving in the second line, which contains rituximab, are you switching out monoclonal antibodies in the second-line setting for patients with large cell lymphoma?
GHANEM: I think it depends on the patient. I tend to use rituximab with gemcitabine/oxaliplatin [R-GemOx], or the new regimen, polatuzumab vedotin [Polivy] plus bendamustine [Bendeka] with rituximab if the patient is not a candidate for a transplant. I still use rituximab in this line.
VIJ: We usually use RICE [rituximab, ifosfamide, carboplatin, and etoposide] for the most part.
LUNNING: Let’s say a patient received EPOCH [etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin hydrochloride] in the frontline setting. Are you altering the second-line regimen based upon what they received in the first line, if it’s different than R-CHOP?
VIJ: I think most of our patients as a second-line treatment receive RICE. There’s a popular regimen that we’re now using on some of the patients if they’re not going to go for a transplant, they should immediately be on CAR [chimeric antigen receptor] T cells soon, then polatuzumab. Then the bendamustine-rituximab regimen has been a little bit more popular, but not for elderly patients going for that regimen.
LUNNING: [What are some] key factors in your mind that help or persuade you to go one direction when making a second-line therapy decision?
RAJA: The main point at second line is whether they’re fit for transplant or not, so if they are fit for transplant then I start with RICE and they go on for transplant. If they’re not f it for transplant, in the past I’ve used bendamustine/rituximab and now we have polatuzumab which I’ve not had a chance to use yet. The patient’s performance status and age come into play and the treatments, depends on how effective and safe they are, and if they have any underlying comorbidities that can prevent us from using the longest drugs or not.
TU: The factor that decided what to do, depending on whether they can’t have the transplant, is do the RICE treatment and bridge them to the transplant. If not, I was thinking send them to CAR T or using tafasitamab [Monjuvi] and lenalidomide [Revlimid].
LUNNING: What is your reaction to the efficacy data for the combination of tafasitamab and lenalidomide? What are your thoughts about these data?
NANNEY: I think it’s very promising, especially the toxicity profile of [the treatment] besides the neutropenia and thrombocytopenia, patients tolerate it very well.
LUNNING: Is that from experience, or because you’ve seen the data before? NANNEY: Experience.
HADDADIN: [This treatment] would be good for the second line. It looks good, and the safety profile is also adequate. I have not used it yet, but I like what I see.
LUNNING: What’s most striking to you, Dr Tu? What are your thoughts that jump out at you about tafasitamab and lenalidomide?
TU: It’s the tail of the survivor data [when looking at the Kaplan-Meier curves], so it looks like it can even cure some people.
LUNNING: The tail of the curve is the most telling, right, in some of these relapse/refractory lymphoma treatments.
VIJ: I look after these patients when they’re hospitalized. Lymphoma is not my primary area of focus, but the data certainly looks very good. I think that 1 of the reasons is that they’ve excluded, I think, patients with double-hit and triple-hit [lymphoma]. So they were a somewhat selected group of patients. I can’t say that the data are not spectacular, because they are.
MATTAR: The 31% at the 2-year mark is very interesting.
The part that I was a bit confused about—[for patients with] primary refractory disease, they may not be eligible, but there was a bunch of primary-refractory patients. Am I correct on that, or did I misunderstand [these data]?
LUNNING: The definition of refractory disease was changed, I believe, midway through the trial. There were some patients who were deemed refractory based upon a new amendment in the trial. So that’s how I believe those patients got in there. There was more of an amendment in the conduct of the trial that was halfway through it.
MATTAR: Compared with the [new treatment] Zynlonta [loncastuximab tesirine-lpyl], I am usually using rituximab lately.2 What’s the difference between this 1 and loncastuximab, as both of them are anti-CD19 [antibody drug conjugate therapies]?
RAJEH: This is very interesting and a new agent to be used, but this is not a randomized trial; this is only a second-line [trial]. We have so many options for second-line treatment, and we are not able to compare it with what we have available now. I’ve seen a lot of patients receive multiple agents as a second- and a third-line treatment, and yet they have relatively extended survival. So I’m not so sure that that’s ready for prime time to use it on every patient at this time.
RAJA: I think [the safety data are] impressive. I feel most of the toxicity is from lenalidomide and probably likely not from the tafasitamab. Combining these 2 is really leading to [better results]. Overall, I feel it’s a very well-tolerated regimen. The majority were able to stay on the lenalidomide and complete it as planned without needing any dose reductions, so that’s very striking to me.
HADDADIN: Only 12% had discontinuation of treatment based on the AEs. I think that’s good. I agree, I think most of the AEs are related to lenalidomide [less so with tafasitamab].
BABLEO: The neutropenia is high. I was wondering, the treatment-related death is kind of high at 13%. What was that mostly due to? Infection?
RAJA: It doesn’t mention that it is not drug-related.
RAJEH: Have these patients received [intravenous immunoglobulin] to supplement their own immunoglobulin?
LUNNING: I’m sure if they had recurrent signs of pulmonary infections and they were having a low immunoglobulin, I believe [they would have a] discussion with a monitor at the time. But I don’t remember the [investigators] calling out how many individuals were supplemented, or if it was allowed in the study.
MATTAR: I think the mortality concerned me a little bit, because this is [close to] CAR T-cell mortality. If you look at lisocabtagene maraleucel or axicabtagene ciloleucel [axicel], they have around 2 or 3 cases of morality, no more than that.3 That [was a] big study of 70 or 80 patients. If I’m giving feedback, for the study, that’s 1 of the things that concerns me a little bit. I would probably dissect that fact a little bit more to appease the anxiety of oncologists.
RAJEH: Well, those patients mostly did not fit a transplantation, so it’s likely they have poor performance status or comorbidity issues. They’re expected to have a higher mortality. That’s my expectation.
MATTAR: They could have been a CAR T candidate, too, right?
LUNNING: After a second line of therapy, correct, they could have been a CAR T-cell candidate from that standpoint. MATTAR: But for some of the patients in ZUMA-7 [NCT03391466], they’re still looking at CAR T instead of transplant, so we’ll see what the results will be in a few months. But even in the second line, some of those, like axi-cel, could end up being second-line treatment. L
LUNNING: We’re all waiting for the potentially exciting results for ZUMA-7, BELINDA [NCT03570892] and TRANSFORM [NCT03575351], as we had 3 competing randomized trials going after the same second-line space.
LUNNING: After reviewing the data, would you consider this combination for patients?
RAJEH: I think I could consider it in any patient, especially [patients that are] chemotherapy-refractory, if the patient progressed on the first line, rather than if they progressed shortly after achieving some response.
HUESER: I think [the treatment] looks very well tolerated. It’s got durable responses, and the cytopenias don’t seem to be something that’s too difficult to deal with. Although, when they talked about having the 13% mortality, I think that’s a good point, being that some of these patients are already beat up with chemotherapy and probably aren’t doing too well, regardless. Even still, it looks like a very good regimen and I’m very impressed with the data and the durability of it.
LUNNING: Does it bother you that this is a treatment-to-progression type of a regimen?
NANNEY: That’s 1 of the discussions that I had with 1 of the patients that I have on the regimen right now. [The patient] had relapsed and had an excellent response to 2 cycles of RICE, and we couldn’t go further. They were not a transplant candidate at that time and had significant disease, so we had the discussion about what do we do next, R-GemOx or the immunotherapy, and we went with the immunotherapy. [The patient] has done wonderfully with it. They’ve been on it now for 6 months, no progression, tolerating it well, and having a little bit of difficulty with the lenalidomide and a little bit of trouble with low counts. But the counts you can easily manage with growth factors, and the patient is doing well for someone who’s 75 years old.
LUNNING: Have you been able to maintain the lenalidomide dose then?
NANNEY: The patient has renal insufficiency and so we’ve reduced the dose because of their renal insufficiency.
LUNNING: Do you see any barriers to using tafasitamab and lenalidomide?
GHANEM: I think the platelet counts are the main barrier here, and the combination with lenalidomide. The lenalidomide by itself is usually difficult to keep patients on because of the side effects, low counts, the kidney function tests, and adding another drug. However, the efficacy is really impressive, so I didn’t try this regimen before, but it seems to be really a good choice at this point to try.
LUNNING: Would you consider CAR T-cell therapy after tafasitamab if there’s evidence of progression of disease?
HADDADIN: It depends on how the patient is doing afterward. If the patient has the adjuvant performance status, doing well, then yes, I’ll probably go for that.
MATTAR: My concern is about the anti-CD19 and CAR T cell. But I think if we extrapolate from [other studies looking at similar treatments in cancers like myeloma] it does not concern me too much. I don’t feel like this will burn the bridge for me, because you can still have enough lymphocytes with CD19. You’re not going to inhibit them all where you have enough CAR T-cell effect on that.
REFERENCES
1. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
2. Karlovitch S. FDA approves Lonca in relapsed/refractory DLBCL. Targeted Oncology. April 23, 2021. Accessed June 15, 2021. https://bit.ly/3wzXEvK 3. Oluwole O, Bishop M, Gisselbrecht C, et al. ZUMA-7: A phase 3 randomized trial of axicabtagene ciloleucel (axi-cel) versus standard-of-care (SOC) therapy in patients with relapsed/refractory diffuse large B cell lymphoma. J Clin Oncol. 2018;36(15). doi:10.1200/JCO.2018.36.15_suppl.TPS7585
Examining the Non-Hodgkin Lymphoma Treatment Paradigm
July 15th 2022In season 3, episode 6 of Targeted Talks, Yazan Samhouri, MD, discusses the exciting new agents for the treatment of non-Hodgkin lymphoma, the clinical trials that support their use, and hopes for the future of treatment.
Listen