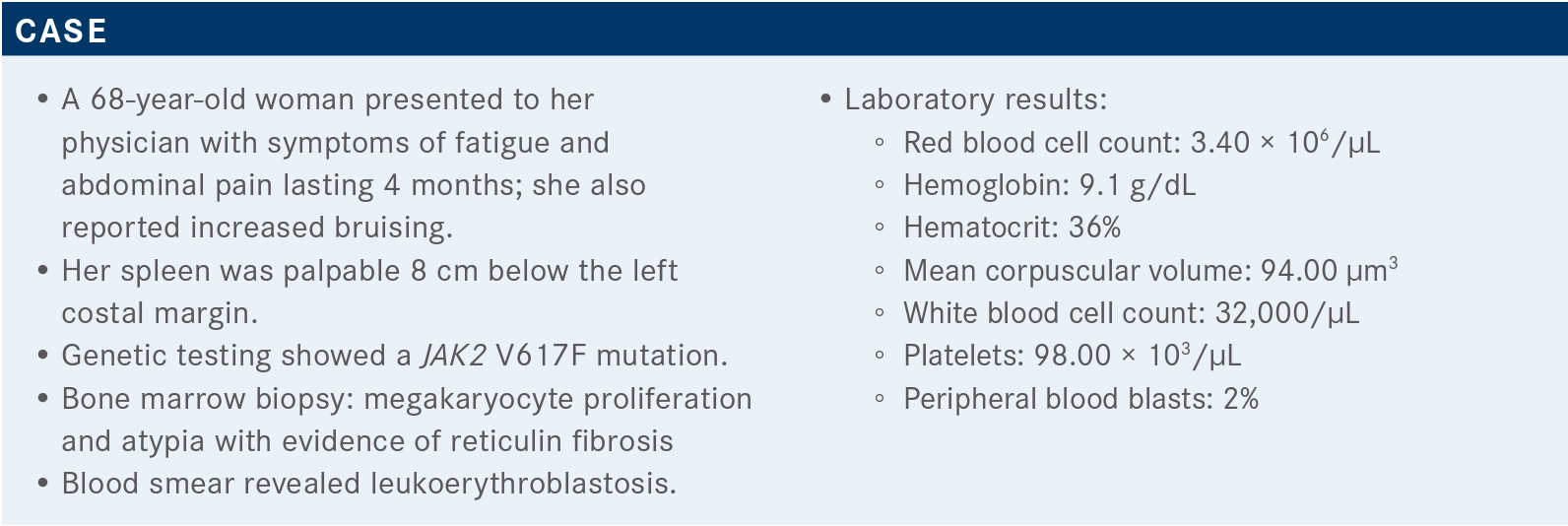
Prognostic Risk System Options Detailed for Myelofibrosis
During a Targeted Oncology Case-Based Roundtable, Ruben Mesa, MD, discussed the prognostic risk systems in myelofibrosis.
Ruben Mesa, MD

In an interview with Targeted Oncology, Ruben Mesa, MD, the executive director of the Mays Cancer Center at UT Health San Antonio MD Anderson Cancer Center discussoses prognostic risk systems in myelofibrosis.
Targeted OncologyTM: How do you choose between the multiple tools for assessing prognostic risk in myelofibrosis (MF)?
MESA: [There are] subtle differences between [the risk assessment tools for MF].1-4 The IPSS [International Prognostic Scoring System] [is used only] at diagnosis. The DIPSS [Dynamic International Prognostic Scoring System] [can be used at diagnosis and] subsequent [time points]. And if [information on] karyotype, red [blood] cell transfusion, and platelet [count is available], you might refine [the assessment] further with the [DIPSS-]Plus.
The DIPSS is probably the most broadly [used] of the [tools] [because of the] limited availability of molecular findings [ie, karyotype]. The challenge with the DIPSS is that patients in the intermediate-1 risk category are heterogeneous.5 [This patient group] might include a younger individual who has anemia and a high-risk molecular feature and might [be considered] for a transplant, [as well as] someone whose only risk factor is being 56 [years old], [ie, just above the threshold for age-related risk].
The MIPSS70 [Mutation-Enhanced International Prognostic Score System for Transplantation-Age Patients With MF] [is another risk assessment tool for MF, and it has an online calculator].6,7 [The important thing for physicians to know is that these risk calculators exist and where to find them, [when to use them], [and what] elements [are needed] to plug into them. [These elements] tell you a bit about the disease. [The MIPSS70] is similar [to the Sokal Index for Chronic Myelogenous Leukemia] and the IPSS-R [revised IPSS for myelodysplastic syndrome]. [This similarity] makes sense [because these calculators] all [assess risk in patients with] chronic myeloid disorders.
The [weight given to specific prognostic factors in calculating the MIPSS70] [may be] either too low or too high. [Nevertheless,] I like [the MIPSS70] because it [includes] both clinical features and molecular features. Some [of the] newer [prognostic risk scores for MF include] only molecular [features], [which] I think is incomplete. The same [genetic] clone [can behave differently] in 2 different people.
I think phenotype matters as well as genetics.
Why are factors that are important for MF prognosis, such as the prevalence of peripheral blood blasts and age, not highly weighted or not included in the calculation of the MIPSS70?
[Age was not included in the MIPSS70 because this tool] focuses [on patients younger than] 70 years, [and age] probably has a subtle [effect on prognosis in this patient group.]
A limitation of these [prognostic risk] scores is [that they are based on] data [that may not be representative] of all patients, [especially those with unusual presentations]. For example, when I was working at Mayo [Clinic in] Rochester, Minnesota, [I had] a patient with [extensive] malignant ascites from their MF, [which I felt was terrible in terms of] prognosis. The [patient died] of AML [acute myeloid leukemia] in 3 months. [But malignant ascites is] not a prognostic marker because [there aren’t] enough [patients with this condition to determine its prognostic value].
Another [issue] is that [prognostic risk scores for MF were developed using] retrospective [data in which spleen size is not precise because] it [was measured] by physical exam. A lot of the older charts are descriptive [and define] the spleen [size very broadly]. There’s little doubt that if the spleen is 30 cm below the costal margin, [the patient is] probably going to do worse, but [the lack of precision in the spleen data may be] why [spleen size] has never [emerged as a prognostic factor for MF]. [When developing the MIPSS70, the investigators] did actually [conduct a] blinded review of [bone marrow samples], and that’s why [bone marrow fibrosis could emerge as a] prognostically significant [factor].
[The MIPSS70-Plus is another] risk score; it includes highrisk karyotype and has some other subtle differences from the MIPSS70.8,9
The MYSEC-PM [Myelofibrosis Secondary to PV and ET-Prognostic Model] [is a prognostic risk score for patients with secondary myelofibrosis].10,11 There is a subtle difference [in prognosis] for patients who evolve from polycythemia vera [PV] or essential thrombocythemia [ET] because [these] patients typically have a better hemoglobin or platelet count than [patients with] primary MF. [The absence of] anemia probably [means something] different [in a patient with primary compared with secondary MF], so there is really quite a difference [what hemoglobin] counts [mean for prognosis in these patient groups].
There is another [prognostic risk] score [for MF], [which] was developed by transplant [physicians and] looks at transplant outcome [rather than survival]. [This score] is very helpful when you’re trying to make a difficult decision [about whether to transplant, and it includes not only disease factors but also other relevant factors, such as] the patient’s performance status and whether the [transplant is from a] mismatched donor.
Do you find these risk assessment tools to be beneficial in your practice? How can they be used for treatment decision-making?
[I think these tools are helpful, but they may not make a big difference in decision-making for treatment or transplantation.] I think that the patient’s disease burden, [for example, symptoms, splenomegaly, and anemia], is as or more important [in making treatment decisions].
The National Comprehensive Cancer Network [NCCN] guidelines have [recently been] adjusted [to simplify the interpretation of prognostic risk scores for MF].12 [Although there are many] scores, most [differentiate patients at] a lower [versus a higher] risk [of disease progression].
So [NCCN guidelines have adopted a] kind of lower-risk [versus] higher-risk [paradigm].12 In higher-risk [patients] with marked thrombocytopenia [platelet count, <50 × 109/L], [physicians should] consider [referral for enrollment in] a clinical trial, [for example, a trial evaluating] fedratinib [Inrebic], [which] may well get FDA approval in the near future for [use in] this group of patients. Clearly, transplant [should also be] considered [in this high-risk patient group].
How important is it to initiate therapy early? What treatment options are available in this setting?
[No patient is] going [to undergo a] transplant right away [because a transplant takes time to set up]. I would argue [that, in the interim,] the patient [should start] on a JAK inhibitor to shrink the spleen, improve symptoms, and improve their performance status. [The patient will] probably benefit from this approach, and if they don’t benefit, or they relapse, fedratinib is approved [for use] in this setting. And there may be other [drugs that could be used], as well, [for such patients].
What data support the use of ruxolitinib [Jakafi] in this setting?
[Data from] the COMFORT studies, [which evaluated] ruxolitinib versus placebo [COMFORT-I; NCT00952289] or versus best alternative therapy [BAT; COMFORT-II; NCT00934544]13,14 [show that in both trials, a reduction in spleen size of at least 35% occurred significantly more often in the ruxolitinib group than in the comparison group [COMFORT-I, 41.9% vs 0.7%; COMFORT-II, 28.0% vs 0%], [and ruxolitinib also reduced symptoms]. [Only a subset of patients reached the threshold of at least 35% reduction in spleen size], but over time, the majority of patients got some benefit [from ruxolitinib, although perhaps not as much] as we would like.
Data from COMFORT-I showed that ruxolitinib improves symptoms better than placebo.13 And I think the benefits of ruxolitinib are multifactorial: It decreases inflammation, decreases cytokines, and helps to improve a variety of inflammatory markers. [Symptom improvement with ruxolitinib] was [also seen in] the COMFORT-II study, which compared ruxolitinib with BAT. Over time, we’ve learned that [hydroxyurea (Hydrea) is not a very effective] therapy for MF. The COMFORT-II study really helped to demonstrate this [because most of the trial patients previously received hydroxyurea treatment for MF]. Hydroxyurea remains a pretty good drug for ET and an OK drug for PV but not a very good drug for MF.
The [COMFORT] trials were not designed [to evaluate] survival. [Nevertheless, a pooled analysis for ruxolitinib demonstrated that ruxolitinib prolonged overall survival compared with placebo] [median overall survival 5.3 months versus 3.8 months with BAT or placebo; HR, 0.70; 95% CI, 0.54-0.91; P = .0065].15 [Generally, survival is difficult to evaluate in these trials because] it’s hard to keep patients on a control arm indefinitely. Some studies have been doing [this] in a setting of second-line therapy, and we will see whether they’re successful. But multiple real-world analyses [evaluating the effect of ruxolitinib on survival], as well as these data [from the COMFORT studies, suggest that ruxolitinib does improve survival].
I think [that improved survival with ruxolitinib may arise from] a range of [effects], not the least of which, I think, is a decrease in the inflammatory milieu in the bone marrow and a slower accumulation of additional somatic mutations. I think [these effects] correlate with the [degree] of [the spleen] response, but I don’t think [the response to ruxolitinib is] solely the improvement in the size of the spleen. [Rather], the spleen [may be] a good biomarker of response. If there’s a response to JAK inhibition, the spleen [shrinks].
[Observational data have also] shown that [in patients treated with ruxolitinib, a better] spleen response [and a higher dose of ruxolitinib are associated with improved survival].16, 17
One of the things we have run into over many years of using ruxolitinib is that the dose matters. [Data from COMFORT-I show that doses of less than 10 mg twice a day are not effective in reducing spleen volume or total symptom score].18 There probably is an overrepresentation of lower-dose ruxolitinib [in clinical practice]. I see patients with thrombocytopenia who are on a ruxolitinib dose of 5 mg twice a day or 5 mg once a day, and these doses are probably suboptimal in terms of improvement in the spleen or symptoms and may also diminish the likelihood of [improved] survival.
[Long-term] use [of ruxolitinib] can cause cytopenia.13,14 These [toxicities are] usually not a major factor [for the patient], but ruxolitinib certainly does not improve anemia. [In the COMFORT trials, anemia occurred more often in the ruxolitinib group than in the comparison group] [COMFORT-I, 45% vs 19%; COMFORT-II, 42% vs 31%].
[Early studies of ruxolitinib suggested that its effect on] platelets was the dose-limiting toxicity. [More recently, data from the EXPAND dose-escalation trial (NCT01317875)] [showed that] starting [ruxolitinib] at a lower dose is a safe approach [ie, at a maximum of 10 mg twice a day] and that to optimize the benefit [of ruxolitinib therapy], you need to increase the dose.19,20
[The EXPAND study evaluated 2 groups of patients, those with very low platelet counts (range, 50-74 × 109/L) and those with slightly higher platelet counts [range, 75-99 × 109/L]. [The study findings showed that these] patients [with low platelet counts] can still respond [to ruxolitinib therapy], [with a reduction] in the spleen [size and an] improvement in symptoms. Many of [these patients tolerated doses of] up to 15 mg twice a day, even when they started with a lower dose.19,20
What other JAK inhibitors can be used to treat patients with MF in the frontline setting?
If pacritinib is approved [as treatment for MF, we may be discussing how to manage a patient with a] platelet count of 45,000, [in terms of whether to treat with pacritinib or with] a lower dose of ruxolitinib.
Fedratinib [was approved by the FDA for treatment of highrisk MF in] September 2019.21 [Data from the JAKARTA trial (NCT01437787)] showed good spleen responses to fedratinib [400 mg compared with] placebo [≥ 35% reduction in spleen volume, 36% vs 1%]22,23; the 400-mg dose is the currently approved dose.21 Fedratinib has a similar [cytopenia] profile as ruxolitinib. It is associated with more gastrointestinal adverse events than ruxolitinib, but I find that [these are] manageable, [for example with use of] Zofran.
What are some considerations for selecting fedratinib versus ruxolitinib as frontline treatment for MF in patients presenting with a low platelet count?
I have [used fedratinib as frontline therapy in a small number of patients with MF]. [An advantage of fedratinib is that] you can [start patients on] a higher, more effective dose [than you can with ruxolitinib]. But I think [fedratinib has been] most helpful in the second-line setting, [particularly during the COVID-19 pandemic]. [During the pandemic] it has been hard for [patients] to travel, [and fedratinib requires fewer trips to the clinic for dose adjustments]. I think that fedratinib is pretty good in the secondline setting, [and data suggest that it’s pretty similar to ruxolitinib] in the [frontline] setting. [However, physicians] are used to using ruxolitinib [and may not be comfortable using fedratinib as frontline therapy].
We do know [that with fedratinib] there’s a low but probably real [risk of Wernicke encephalopathy, resulting from depletion of] thiamin [reserves].22,24,25 I’ve not found [this risk] to be a barrier to using fedratinib, but I certainly don’t ignore it. I check the [patient’s] thiamin level, check for Wernicke [encephalopathy], although it’s unlikely, and if need be, [administer thiamin and] monitor. I give [all my patients] thiamin; [it’s inexpensive and has few adverse events, and ongoing] studies [with fedratinib] [confirm that the drug] can lower thiamin levels.
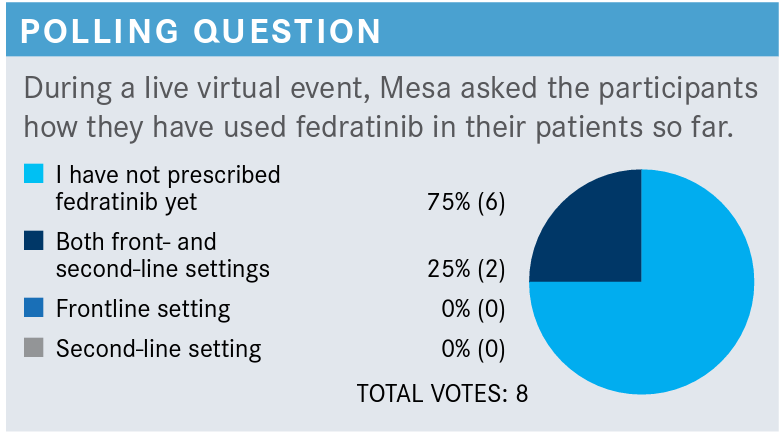
[Most] have not used [fedratinib] yet, and that’s not a big surprise; a couple [of you have used it] in the frontline and second-line [settings]. [Fedratinib] is a good drug, and you should consider [using it in patients] with MF who have [not had] a great response to ruxolitinib and [for whom] participation in a clinical trial [would be] too big of a hassle.
For higher-risk patients [with MF], the NCCN guidelines [recommend fedratinib as] a preferred option for secondline medical therapy.12 But it’s important to [revisit the issue of transplant in patients for whom JAK inhibition had reduced the immediate benefit of transplant].
REFERENCES
1. Bose P, Verstovsek S. The evolution and clinical relevance of prognostic classif ication systems in myelofibrosis. Cancer. 2016;122(5):681-692. doi:10.1002/ cncr.29842
2. Cervantes F, Dupriez B, Pereira A, et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood. 2009;113(13):2895-2901.doi:10.1182/ blood-2008-07-170449
3. Passamonti F, Cervantes F, Vannucchi AM, et al. A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplasms Research and Treatment). Blood. 2010;115(9):1703-1708. doi: 10.1182/blood-2009-09-245837
4. Gangat N, Caramazza D, Vaidya R, et al. DIPSS plus: a refined Dynamic International Prognostic Scoring System for primary myelofibrosis that incorporates prognostic information from karyotype, platelet count, and transfusion status. J Clin Oncol. 2011;29(4):392-397. doi:10.1200/JCO.2010.32.2446
5. Mesa RA. Individualized care plans for myelofibrosis. Hematol Educ. 2011;5:264272. https://bit.ly/3w0SAj1
6. Guglielmelli P, Lasho TL, Rotunno G, et al. MIPSS70: Mutation-Enhanced International Prognostic Score System for transplantation-age patients with primary myelofibrosis. J Clin Oncol. 2018;36(4):310-318. doi:10.1200/JCO.2017.76.4886
7. MIPSS70 score. Accessed June 17, 2021. https://bit.ly/35Xe99x
8. Tefferi A, Guglielmelli P, Lasho TL, et al. MIPSS70+ version 2.0: Mutation and Karyotype-Enhanced International Prognostic Scoring System for Primary Myelofibrosis. J Clin Oncol. 2018;36(17):1769-1770. doi:10.1200/JCO.2018.78.9867
9. Tefferi A, Nicolosi M, Mudireddy M, et al. Revised cytogenetic risk stratification in primary myelofibrosis: analysis based on 1002 informative patients. Leukemia. 2018;32(5):1189-1199. doi:10.1038/s41375-018-0018-z
10. Passamonti F, Giorgino T, Mora B, et al. A clinical-molecular prognostic model to predict survival in patients with post polycythemia vera and post essential thrombocythemia myelofibrosis. Leukemia. 2017;31(12):2726-2731. doi:10.1038/ leu.2017.169
11. MYSEC prognostic model risk calculator (MYSEC-PM). Accessed June 17, 2021. https://bit.ly/2UNFNDN
12. NCCN. Clinical Practice Guidelines in Oncology. Myeloproliferative neoplasms, version 1.2021. Accessed April 22, 2021. https://bit.ly/2Wcczfa
13. Verstovsek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799-807. doi:10.1056/ NEJMoa1110557
14. Harrison C, Kiladjian JJ, Al-Ali HK, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366(9):787-798. doi:10.1056/NEJMoa1110556
15. Verstovsek S, Gotlib J, Mesa RA, et al. Long-term survival in patients treated with ruxolitinib for myelofibrosis: COMFORT-I and -II pooled analyses. J Hematol Oncol. 2017;10(1):156. doi:10.1186/s13045-017-0527-7
16. Palandri F, Palumbo GA, Bonifacio M, et al. Durability of spleen response affects the outcome of ruxolitinib-treated patients with myelofibrosis: results from a multicentre study on 284 patients. Leuk Res. 2018;74:86-88. doi:10.1016/j. leukres.2018.10.001
17. Palandri F, Palumbo GA, Bonifacio M, et al. Baseline factors associated with response to ruxolitinib: an independent study on 408 patients with myelofibrosis. Oncotarget. 2017;8(45):79073-79086. doi:10.18632/oncotarget.18674
18. Menghrajani K, Boonstra PS, Mercer JA, et al. Predictive models for splenic response to JAK-inhibitor therapy in patients with myelofibrosis. Leuk Lymphoma. 2019;60(4):1036-1042. doi:10.1080/10428194.2018.1509315
19. Verstovsek S, Gotlib J, Gupta V, et al. Management of cytopenias in patients with myelofibrosis treated with ruxolitinib and effect of dose modifications on efficacy outcomes. Onco Targets Ther. 2013;7:13-21. doi:10.2147/OTT.S53348
20. Vannucchi AM, Te Boekhorst PAW, Harrison CN, et al. EXPAND, a dosef inding study of ruxolitinib in patients with myelofibrosis and low platelet counts: 48-week follow-up analysis. Haematologica. 2019;104(5):947-954. doi:10.3324/ haematol.2018.204602
21. Guglielmelli P, et al. The final analysis of expand: a phase 1b, open-label, dosef inding study of ruxolitinib (RUX) in patients (pts) with myelofibrosis (MF) and low platelet (PLT) count (50 × 109/L to < 100 × 109/L) at baseline. Poster presented at: 62nd American Society of Hematology Annual Meeting and Exposition; December 5-8, 2020. Poster 1252. Accessed June 18, 2021. https://bit.ly/3qxBgRE
22. FDA approves fedratinib for myelofibrosis. FDA. August 16, 2019. Accessed April 22, 2021. https://bit.ly/3dErcBr
23. Pardanani A, Harrison C, Cortes JE, et al. Safety and efficacy of fedratinib in patients with primary or secondary myelofibrosis: a randomized clinical trial. JAMA Oncol. 2015;1(5):643-651. doi:10.1001/jamaoncol.2015.1590
24. Harrison CN, Schaap N, Vannucchi AM, et al. Fedratinib induces spleen responses and reduces symptom burden in patients with myeloproliferative neoplasm (MPN)associated myelofibrosis (MF) and low platelet counts, who were either ruxolitinibnaïve or were previously treated with ruxolitinib. Blood. 2019;134(suppl 1):668. doi:10.1182/blood-2019-129288
25. Inrebic. Prescribing information. Bristol Myers Squibb; 2020. Accessed June 18, 2021. https://bit.ly/3jmvCQJ