Roundtable Discussion: Hutson Explores When and How Clinicians Are Using Cabazitaxel in mCRPC
During a Targeted Oncology Case-Based Roundtable event, Thomas Hutson, DO, PharmD, discussed the case of a patient with metastatic castration-resistant prostate cancer.
Thomas Hutson, DO, PharmD

During a Targeted Oncology Case-Based Roundtable event, Thomas Hutson, DO, PharmD, discussed the case of a patient with metastatic castration-resistant prostate cancer.
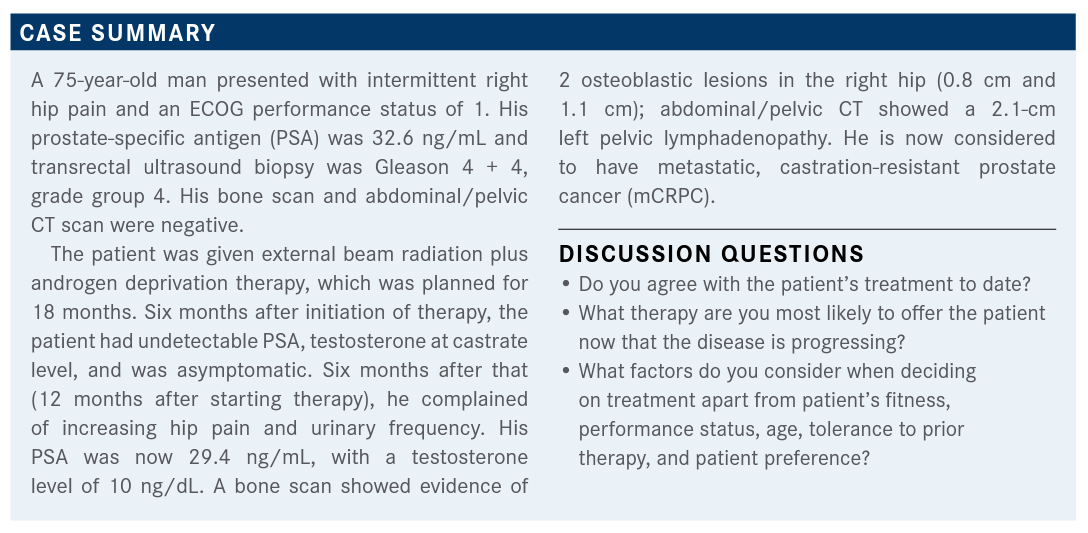
HUTSON: According to the advanced prostate cancer guidelines by the American Urological Association [AUA], the American Society for Radiation Oncology [ASTRO], and the Society of Urologic Oncology [SUO], clinicians should consider prior treatments and sequencing agents and recommend therapy with an alternative mechanism of action.1 Offer radium-223 [Xofigo] to patients with symptoms [of metastases to the bone without known visceral disease or lymphadenopathy]. Recommend cabazitaxel [Jevtana] versus abiraterone [Zytiga]/pred-nisone or enzalutamide [Xtandi] in patients who received prior docetaxel [Taxotere]. This is based upon data from the CARD study [NCT02485691]. Offer PARP inhibitors [to patients with deleterious or suspected deleterious germline or somatic homologous recombination repair gene-mutated mCRPC following prior treatment with enzalutamide or abiraterone, and/or taxane-based chemotherapy]. Offer pembrolizumab [Keytruda] for [mismatch repair-deficient or MSI (microsatellite instability)-high CRPC].
HUTSON: Do you test your patients for PD-1 or MSI?
CHALLAGALLA: We test everybody and for every cancer and then we can give anybody with high TMB [tumor mutational burden] or MSI [the right therapy].
HUTSON: I have tested in prostate [cancer, too]. I have 1 patient who got pembrolizumab as a later-line therapy in prostate cancer and he has done phenomenally well. Clinicians may offer sipuleucel-T [Provenge] [to asymptomatic or minimally symptomatic patients]. Offer platinum-based chemotherapy [in patients who cannot use or obtain a PARP inhibitor].
CHALLAGALLA: I have a patient who after docetaxel therapy had CRPC for almost 10 months. He had a few lymph nodes and is a young man of about 52 years. He did not have a high MSI nor any mutations. Would you think of reusing docetaxel? What is the cutoff? Or would you switch to cabazitaxel?
HUTSON: I am leaning more toward the use of cabazitaxel based on the CARD data prior to which I was never getting to cabazitaxel and my patients were too sick by the time I got to it. So, I’m trying to purposely start using that sooner. Docetaxel [in combination with prednisone] became approved in 2004 [for the treatment of androgen-independent prostate cancer] and [before that] we didn’t have anything.3 Now we have learned that you can, on average, give 16 cycles of docetaxel before someone becomes resistant to it. We used to give 10 cycles at a time, then stop. Now, we give 6 to 8 cycles and then stop. You can then potentially go back to docetaxel and get more mileage from it. Instead, I now go to cabazitaxel. So, you can go back to chemotherapy and decide whether you want it to be docetaxel or cabazitaxel.
HUTSON: Would you give cabazitaxel to a patient who did not tolerate docetaxel?
REDDY: I would use cabazitaxel.
HUTSON: Is it 20 mg/m2 without growth factor support or 25 mg/m2 with growth factor support?
REDDY: [I would use] 20 mg/m2 with growth factor support…because I’ve had problems without growth factor support.
CHALLAGALLA: I use 20 mg/m2. I have not used growth factors unless [there were] extensive bone metastases and my patients were tolerating [treatment well].
WANG: I use 20 mg/m2 without [growth factors]. My experience is that cabazitaxel seems to be better tolerated than docetaxel.
HUTSON: When I do the chemotherapy, my goal is to get the PSA to a lower point and get rid of their symptoms. I don’t continue chemotherapy beyond that goal [to the point where] they’re resistant to it. Do you get a nadir PSA and stop? When you start chemotherapy, do you continue until they are resistant?
CHALLAGALLA: For me, it is until they get toxicity.
REDDY: I watch until the PSA comes to a nadir and maybe do 1 more cycle to confirm.
SAEZ: I go to the nadir and then stop. I do an extra cycle or 2 to make sure it is the nadir and then I’ll stop.
HUTSON: So, no one can tell when someone is refractory. I don’t like doing it because of all the [adverse events (AEs)] of the chemotherapy. I see patients seeking a second opinion who have been on chemotherapy for a long time.
CHALLAGALLA: I have had a patient now for probably 9 to 10 years who had a great response with docetaxel but after 7 cycles he had AEs and I stopped therapy. PSA went to 0.05 ng/mL, stayed there for about 6 months, and then kept rising. I did a PET Axumin [which showed he] had nodal disease and bone metastasis but he had no symptoms at all. So, when enzalutamide was first approved [for mCRPC in patients who have already received docetaxel in 2012] I gave it to him because of all the AEs lingering from docetaxel.4 I could either observe him and do nothing or give him enzalutamide, and he chose enzalutamide.
HUTSON: I’ve had patients who have Parkinson-like symptoms where they end up using oral therapy and sequence and I hope for the best.
The CARD trial was a phase 4 trial of cabazitaxel versus an AR-targeted agent. It was a multicenter trial and median follow-up was 9 months. These were patients with mCRPC who had progressed in less than 12 months on the [alternative AR-targeted therapy] before or after docetaxel. They were randomized to receive cabazitaxel [plus prednisone versus abiraterone plus prednisone or enzalutamide]. [The primary end point was radiographic] progression-free survival [rPFS]. Secondary end points were overall response [OS], PFS, tumor response, and health-related quality of life. [Randomization was stratified] based on [ECOG performance status of (0/1 vs 2), time to progression on their previous AR-targeted therapy (0-6 vs 6-12 months), and timing of AR-targeted therapy (before or after docetaxel)].5
The CARD trial had an older patient population with [about one-third being 75 years and older; those with visceral metastases were just under 20%]. Progression was based on PSA, pain, and radiologic progression. Two-thirds of the people had Gleason 8 to 10 disease.6
Those with metastatic disease at diagnosis were about 40%. So, these patients are not those who had curative intent therapy and then developed recurrence later. Prior alternative AR-targeted therapy with abiraterone/enzalutamide was about 56% versus those who received treatment without previous docetaxel at 38% or those who received treatment after docetaxel at 60%. The median duration of prior alternative AR-targeted therapy was about 8 months.6 My patients are generally on their first oral agent longer than 8 months, but I think this was a patient population with more advanced disease.
For the primary end point, [median rPFS was significantly better for the cabazitaxel group at 8 months compared with the abiraterone or enzalutamide group which was at 3.7 months (HR, 0.54; 95% CI, 0.40-0.73; P < .0001)]. Virtually every preidentified patient subgroup fared better with the cabazitaxel.6
Overall, patients benefited [from cabazitaxel compared with] going for an AR-targeted oral agent. It is hard to do OS trials in prostate cancer, but they were able to show a survival benefit in favor of giving cabazitaxel [HR, 0.64; 95% CI, 0.46-0.89; P = .0078]. The median PFS for cabazitaxel was also better and statistically significant [HR, 0.52; 95% CI, 0.40-0.62; P < .0001].6
PSA, objective tumor response, and pain response had a profound, more than doubling benefit in favor of using the chemotherapy. The time to symptomatic skeletal event was 16.7 months for patients who got the second oral AR-targeted agent but was yet to be reported for the cabazitaxel.7 AEs leading to treatment discontinuation did not have much of a difference between the 2 arms. Serious AEs and those with any grade greater than or equal to 3 were similar for the 2 arms. AEs leading to treatment discontinuation were more on the cabazitaxel arm by about 10%.6
AEs leading to death significantly reduced for cabazitaxel compared with abiraterone and enzalutamide. Overall, cabazitaxel stacks up favorably compared with getting a second oral AR-targeted agent probably more than any of us thought. The health-related quality of life based on the FACT-P [Functional Assessment of Cancer Therapy-Prostate] questionnaire shows the probability of deterioration after 3 months, the prostate-specific concerns, and the well-being of the patient.8
The goal of therapy is to buffer [the anxiety and pain related with prostate cancer] as much as possible and cabazitaxel does better at that compared with abiraterone or enzalutamide. The probability of deterioration at 3 months was slightly in favor of cabazitaxel too.8
HUTSON: Do the data from the CARD trial influence your current practice regarding cabazitaxel?
ALOBA: I already incorporate cabazitaxel into my practice.
CHALLAGALLA: I agree. This was something we were already following.
HUTSON: You’re already using it?
ALOBA: Yes. Except in patients early on in treatment.
HUTSON: Is this new data to anyone or do you already feel like you’re incorporating this?
REDDY: I’m already using it before it is too late because then they may not even be able to tolerate cabazitaxel. So, I try to use this agent when they can still tolerate it.
HUTSON: OK, at least now the data support that. I found that I couldn’t get the cabazitaxel because I had it later in line when people are sicker. One of the ways patients succumb to prostate cancer is bone marrow failure. So, they have pancytopenia from treatment and bone marrow replacement from the cancer.
I am moving to cabazitaxel therapy earlier. The CARD data make me not want to do more docetaxel but go to cabazitaxel sooner than I would have done previously.
REFERENCES:
1. Lowrance WT, Breau RH, Chou R, et al. Advanced prostate cancer: AUA/ASTRO/SUO guideline part I. J Urol. 2021;205(1):14-21. doi:10.1097/JU.0000000000001375
2. NCCN. Clinical Practice Guidelines in Oncology. Prostate cancer, version 2.2021. Accessed June 4, 2021. https://bit.ly/3zczMjG
3. Dagher R, Li N, Abraham S, Rahman A, Sridhara R, Pazdur R. Approval summary: docetaxel in combination with prednisone for the treatment of androgen-indepen-dent hormone-refractory prostate cancer. Clin Cancer Res. 2004;10(24):8147-8151. doi:10.1158/1078-0432.CCR-04-1402
4. Ning YM, Pierce W, Maher VE, et al. Enzalutamide for treatment of patients with metastatic castration-resistant prostate cancer who have previously received docetaxel: U.S. Food and Drug Administration drug approval summary. Clin Cancer Res. 2013;19(22):6067-6073. doi:10.1158/1078-0432.CCR-13-1763
5. de Wit R, Kramer G, Eymard JC, et al. CARD: randomized, open-label study of cabazitaxel (CBZ) vs abiraterone (ABI) or enzalutamide (ENZ) in metastatic castra-tion-resistant prostate cancer (mCRPC). Ann Oncol. 2019;30(suppl 5):v851-v934. doi:10.1093/annonc/mdz394
6. de Wit R, de Bono J, Sternberg CN, et al; CARD Investigators. Cabazitaxel versus abiraterone or enzalutamide in metastatic prostate cancer. N Engl J Med. 2019;381(26):2506-2518. doi:10.1056/NEJMoa1911206
7. Fizazi K, Kramer G, Eymard JC, et al. Pain response and health-related quality of life (HRQL) analysis in patients with metastatic castration-resistant prostate cancer (mCRPC) receiving cabazitaxel (CBZ) versus abiraterone or enzalutamide in the CARD study. J Clin Oncol. 2020;38(suppl 6):16. doi:10.1200/JCO.2020.38.6_suppl.16
8. Fizazi K, Kramer G, Eymard JC, et al. Quality of life in patients with metastatic prostate cancer following treatment with cabazitaxel versus abiraterone or enzalu-tamide (CARD): an analysis of a randomised, multicentre, open-label, phase 4 study. Lancet Oncol. 2020;21(11):1513-1525. doi:10.1016/S1470-2045(20)30449-6
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More