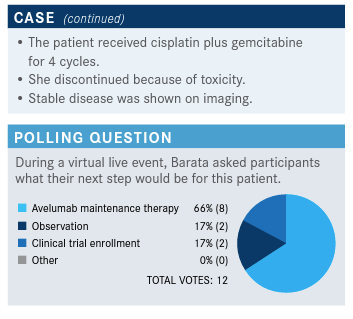
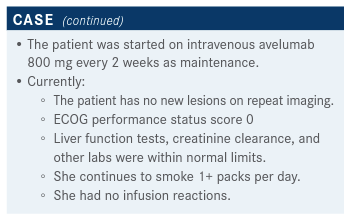
Barata Explains Subgroups of Patients With UC Who May Benefit More From Avelumab Maintenance
Pedro C. Barata, MD, MSc, discussed the case of a 66-year0old woman with urothelial carcinoma during a Targeted Oncology Case-Based Roundtable event.

Pedro C. Barata, MD, MSc, an assistant professor of Medicine Hematology and Medical Oncology at Tulane University School of Medicine, discussed the case of a 66-year0old woman with urothelial carcinoma (UC)during a Targeted Oncology Case-Based Roundtable event.
Targeted OncologyTM: What data support the use of platinum therapy for UC?
BARATA: Platinum has been and still is the standard of care. [Gemcitabine plus cisplatin (GC)], dose-dense MVAC [methotrexate, vinblastine, doxorubicin, and cisplatin plus a colony stimulating factor], or MVAC are the traditional therapies. In the preimmunotherapy era you had several studies [that assessed the efficacy of platinum-based treatment] done in the frontline setting. I will remind that [dose-dense] MVAC has been compared to conventional MVAC.1 [In that study, the 5-year median overall survival (OS) was 15.1 months in the dose-dense cohort and 14.9 months in the conventional MVAC cohort (HR, 0.76; 95% CI, 0.58-0.99).1,2 GC has also been studied in patients who had poorer performance status and renal dysfunction (eGFR 31-59 mL/min) and are usually considered ineligible for a platinum-based regimen.2,3 A randomized phase 2/3 study assessed GC versus methotrexate plus carboplatin plus vinblastine (M-CAVI) in previously untreated patients with advanced urothelial cancer ineligible for cisplatin-based chemotherapy (NCT00014274).3] The CG cohort had some durable responders who remained alive at 72 or more months afterward, which is quite cool.2,3 The median OS was 14 months for those treated with GC and 15.2 months for M-CAVI [HR, 1.09; 95% CI, 0.88-1.34].3 [For cisplatin-ineligible patients, the standard chemotherapy regimen is gemcitabine plus carboplatin, but it achieves relatively lower response rates.] I would argue, based on these data, if we can do a cisplatin-containing regimen, we should consider it based on that.
Where does immunotherapy come into the treatment plan for a patient like this, and what are the data that you consider when making that decision?
We know immune checkpoint inhibitors [ICI] inhibit the signal that the cancer cell transmits to the immune system, telling it “don’t attack me.” By doing that, you have an activation of the immune system to fight cancer better. [ICIs are active against UC and have good safety profiles compared with platinum-based chemotherapy, which is the first-line treatment.4,5 Additionally, resistance to chemotherapy decreases the duration of PFS (progression-free survival) and OS.4,6,7 However, there may be a synergistic effect if the cytotoxic and immunogenic properties of chemotherapy and the antitumor activity ICIs are combined.]
That was the rationale to come up with the JAVELIN Bladder] 100 study [NCT02603432], which was a large trial that’s basically asking [whether an ICI can be used as maintenance therapy in advanced UC.6,7] Patients who were [treated with gemcitabine plus cisplatin or carboplatin] for advanced UC who did not [have disease progression] after 4 to 6 cycles were [eligible]. [There were] 700 trial [participants], randomized 1:1 to observation, which was the standard of care at that point, or observation with avelumab [Bavencio]. [Patients remained in the study until disease progression, an unacceptable level of toxic effects, withdrawal of consent, or any other criterion for withdrawal occurred.] The primary end point was OS, which is the gold standard end point.7 The 2 stratification factors were best response to first-line chemotherapy [complete response or partial response versus stable disease], and metastatic site visceral disease versus no visceral disease.
I would like to highlight 2 points. The randomization happened after completion of the chemotherapy.7 In other words, if a patient received 4 cycles of chemotherapy and [their disease progressed], they would [have been ineligible for] the JAVELIN Bladder 100 study. The other point I would like to make is that no crossover was allowed within the study. So [patients in the control arm] didn’t get avelumab [if their disease progressed]. The reason why the trial didn’t cross over is to minimize the bias. That doesn’t mean patients wouldn’t get a different immunotherapy afterward. [Nearly half of patients in the control arm went on to receive an ICI after disease progression.]
It was a positive study. Patients who completed a platinum-containing regimen and were offered avelumab observation had a median OS of 21.4 months compared with 14.3 months for patients who underwent observation only. That’s a hazard ratio [HR] of 0.69; in other words, [patients had a] 31% risk reduction if they were offered avelumab as maintenance [95% CI, 0.56-0.86; P = .001]. The study met the primary end point and [avelumab] got approved based on that; it made people live longer.8
Do you know why immunotherapy was not studied with chemotherapy?
The combination with chemotherapy has been done in different phase 3 trials. [For example, it has been done] with atezolizumab [Tecentriq], pembrolizumab [Keytruda], and durvalumab [Imfinzi]. The bottom line is, up to now, we have failed to show a survival advantage with concomitant immunotherapy plus chemotherapy. The only trial that’s shown a survival advantage of immunotherapy in the first-line setting is JAVELIN Bladder 100, where you do it as maintenance and not from the get-go.7 There was another study with pembrolizumab in maintenance as well. We did not see a survival advantage in that study.9 Bottom line is that the strategy has been tested. Not all the data have been teased out; for example, we are still waiting for mature survival data for atezolizumab. But as of today, the only data that have shown a survival advantage have been the JAVELIN Bladder 100.
Can you describe the efficacy and safety data that support avelumab as maintenance treatment in a patient like this?
The PFS [in the avelumab arm] almost doubled, 3.7 months versus 2 months [HR, 0.62; 95% CI, 0.52-0.75; P < .001].6,7 I think when I look at these kinds of [data they are] a hypothesis generator. I think it’s important to note that [OS] seems very similar for patients with eGFR below and above 60 mL/min.7 [The HR was 0.68 for both arms (≥ 60 mL/min, 95% CI, 0.50-0.92; < 60 mL/min, 95% CI, 0.5-0.94].7 [OS] also seems to be very similar [in best] response [to chemotherapy] regardless of [whether patients had a] complete response or partial response versus stable disease at the time of [entry into the] trial. [The HR for the complete response/partial response arm was 0.69 (95% CI, 0.53-0.89) and the HR for stable disease was 0.7 (95% CI, 0.46-1.05)]. [OS] by the kind of chemotherapy [patients received], cisplatin or carboplatin, seemed to be similar [HR for CG, 0.69; 95% CI, 0.51-0.94; HR for gemcitabine plus carboplatin, 0.66; 95% CI, 0.47-0.91]. I think that’s reassuring, because it favors the fact that this patient population is likely to benefit regardless of the factors I just mentioned.
The PD-L1 positivity seems to be driving part of this signal. It was present about half of the time and what seems to be different, in my opinion, is the location of metastatic disease.7 Patients with visceral disease did not seem to benefit as much as patients without. This might be because this is a known poor prognostic factor. [An additional prespecified subgroup analysis assessed the median OS based on stratification by site of metastases and by best response.]10 It does seem among all the factors that the presence of visceral disease does determine outcomes. Patients with visceral metastases did worse than those with nonvisceral metastases. The median OS was 18.9 months for those with visceral metastases treated with avelumab and 14.0 months for those with nonvisceral metastases in the observation arm (HR, 0.82; 95% CI, 0.62-1.09). In contrast, the median OS in the treatment arm [in patients] who had nonvisceral metastases was 28.3 months and 15.2 months in the observation arm [HR, 0.54; 95% CI, 0.38-0.76]. The presence of visceral disease determines [poor] outcomes. I would highlight [for best response, the HR for PFS] favors avelumab. Those with a complete response had an HR of 0.65 [95% CI, 0.45-0.96]. Patients with a partial response had an HR of 0.58 [95% CI, 0.44-0.75] and those with stable disease had an HR of 0.61 [95% CI, 0.42-0.87]. Again, this is a hypothesis generator, but it shows that whether you have tumor shrinkage or not, you’re likely to benefit from avelumab. I think that, to me, would be the take-home point.
[Patient flow through the study was mapped and fewer] patients on avelumab [received] subsequent [drug] therapies because they did better on avelumab than observation.6,7 [In the avelumab arm 42.3% of patients received subsequent therapies and 61.7% of patients received subsequent therapies in the observation arm.] [Of those in] observation, 43.7% received a PD-1 or PD-L1 inhibitor and 70.8% of patients [received] a checkpoint [inhibitor overall]. What this tells us is, you don’t want to save your best weapons for later because you might lose your window of opportunity to use them. No. 2, even though crossover was not allowed, almost half of patients in the observation arm were able to get immunotherapy. Because we see the difference in survival, this favors the point that we should use immunotherapy sooner rather than later. To me, that’s an important point that tells the story that maybe maintenance avelumab is the new standard of care.
An important point about safety [is that] discontinuation [occurred in] about 1 out of 10 patients.7 Avelumab seems similar to other checkpoint inhibitors and that’s reassuring. Importantly, no hospitalizations, no deaths occurred, and high-dose steroids were used in about 10% [of patients]. The safety profile for immune-related AEs [adverse events] was very reassuring, in my opinion.
Because of [the results from the JAVELIN Bladder 100 trial], the FDA approved avelumab for UC maintenance in June of [2020].8 Based on [these] phase 3 data, [the NCCN guidelines incorporated avelumab as a first-line, category 1 maintenance therapy for UC].5
Data presented [at the 2021 Genitourinary Cancers Symposium] stratified the outcomes by duration of first-line chemotherapy.11 [Subgroups were defined by quartiles (Q) for duration (< Q1, < 15.0 weeks; Q1-Q2, 15.0 to < 18.0 weeks; Q2-Q3, 18.0 to < 20.1 weeks; and > Q3, > 20.1 weeks) or estimated number of cycles (4, 5, or 6) of first-line chemotherapy.]
[The groups that got more lines of chemotherapy appeared to have a higher proportion of patients who had received GC as first-line treatment and had better performance status.] [The data indicate that] the survival advantage seems to be [present] independent of the duration [or number] of cycles. I think this is an important piece of information because some oncologists are treating with chemotherapy for 4 cycles, others are pushing up to 6 cycles and the advantage of maintenance [with avelumab] seems to be there irrespective of that.
References:
1. Sternberg CN, de Mulder P, Schornagel JH, et al; EORTC Genito-Urinary Cancer Group. Seven year update of an EORTC phase III trial of high-dose intensity M-VAC chemotherapy and G-CSF versus classic M-VAC in advanced urothelial tract tumours. Eur J Cancer. 2006;42(1):50-54. doi:10.1016/j.ejca.2005.08.032
2. Plimack E. Checkpoint inhibition in metastatic urothelial carcinoma: timing is everything. Presented at: 2020 American Society of Clinical Oncology Virtual Scientific Program; May 29-31, 2020; virtual. Accessed June 13, 2021.
3. De Santis M, Bellmunt J, Mead G, et al. Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer who are unfit for cisplatin-based chemotherapy: EORTC study 30986. J Clin Oncol. 2012;30(2):191-199. doi:10.1200/JCO.2011.37.3571
4. Grivas P, Agarwal N, Pal S, et al. Avelumab first-line maintenance in locally advanced or metastatic urothelial carcinoma: applying clinical trial findings to clinical practice. Cancer Treat Rev. 2021;97:102187. doi:10.1016/j.ctrv.2021.102187.
5. NCCN. Clinical Practice Guidelines in Oncology. Bladder cancer, version 3.2021. Accessed June 13, 2021. https://bit.ly/3h4clSK
6. Powles T, Park SH, Voog E, et al. Maintenance avelumab + best supportive care (BSC) versus BSC alone after platinum-based first-line (1L) chemotherapy in advanced urothelial carcinoma (UC): JAVELIN Bladder 100 phase III interim analysis. J Clin Oncol. 2020;38(suppl 18):LBA1. doi:10.1200/JCO.2020.38.18_suppl.LBA1
7. Powles T, Park SH, Voog E, at al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218-1230. doi:10.1056/NEJMoa2002788
8. FDA approves avelumab for urothelial carcinoma maintenance treatment. News release. FDA. Updated July 1, 2020. Accessed June 14, 2021. https://bit.ly/3jaforD 9. Galsky MD, Mortazavi A, Milowsky MI, et al. Randomized double-blind phase II study of maintenance pembrolizumab versus placebo after first-line chemotherapy in patients with metastatic urothelial cancer. J Clin Oncol. 2020;38(16):1797-1806. doi:10.1200/JCO.19.03091
10. Grivas P, Park SH, Voog E, et al. Avelumab first-line (1L) maintenance + best supportive care (BSC) vs BSC alone with 1L chemotherapy (CTx) for advanced urothelial carcinoma (UC): subgroup analyses from JAVELIN Bladder 100. Ann Oncol. 2020;31(suppl_4):S555-S556. doi: 10.1016/j.annonc.2020.08.776
11. Loriot Y, Powles T, Durán MÁC, et al. Avelumab (Ave) first-line (1L) maintenance plus best supportive care (BSC) versus BSC alone for advanced urothelial carcinoma (UC): JAVELIN Bladder 100 subgroup analysis based on duration and cycles of 1L chemotherapy. J Clin Oncol. 2021;39(suppl 6):438. doi:10.1200/JCO.2021.39.6_suppl.438