Akerley Discusses Different Regimens in Advanced Stage NSCLC
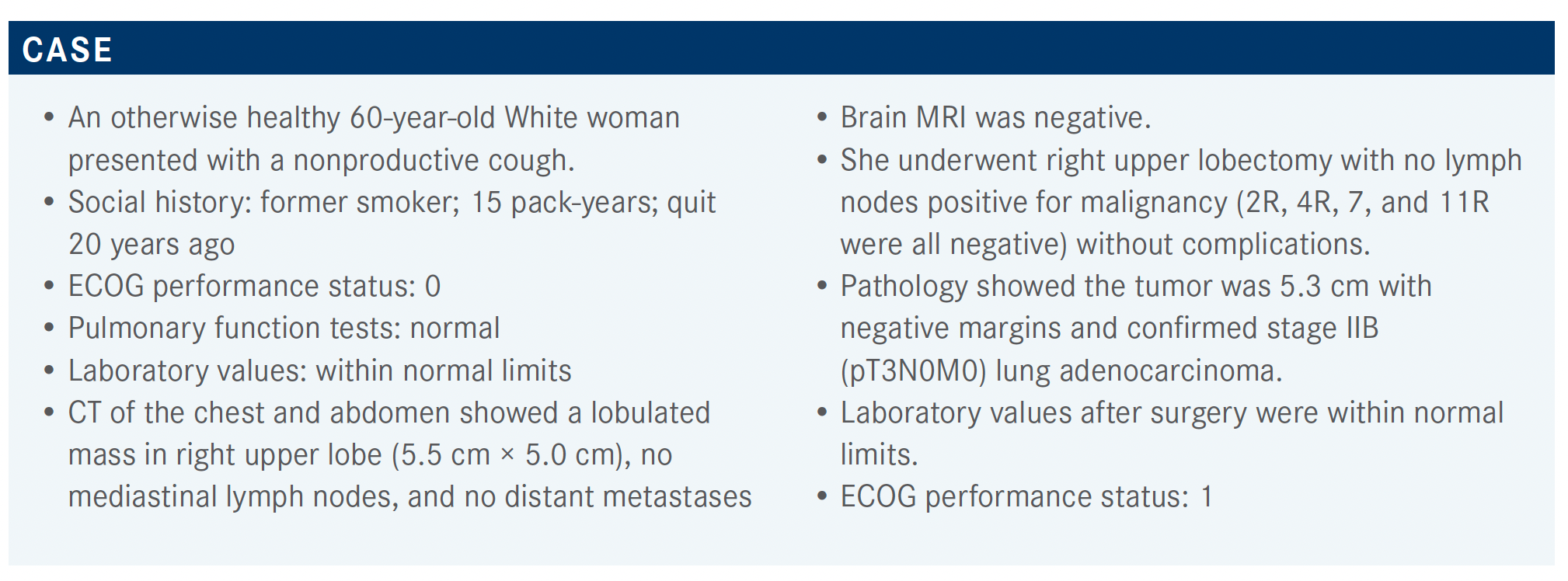
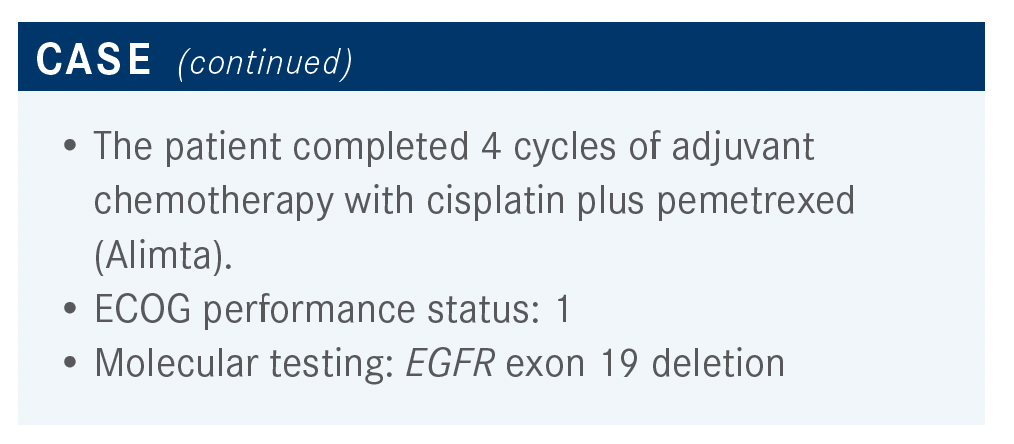
An otherwise healthy 60-year-old White woman presented with a nonproductive cough. She was later diagnosed with advanced stage non–small cell lung cancer.
Wallace Akerley, MD

Wallace Akerley, MD, medical oncologist, chairman, Protocol Review and Monitoring Committee, and director, Lung Cancer Disease Center of Excellence, Huntsman Cancer Institute, Salt Lake City, UT, discussed the case of a patients with advanced stage non–small cell lung cancer during a Targeted Oncology Case-Based Roundtable event.
Targeted OncologyTM: What is the role of adjuvant chemotherapy in your practice? What are the treatment goals?
AKERLEY: Whether a patient’s disease is metastatic or whether they have regional disease, [there] is a high chance of relapse—not everybody benefits with adjuvant chemotherapy. The benefits come in terms of increasing the cure rate.…By the time you get to stage II and certainly stage III, you’re benefiting the patient. Are there benefits in terms of cure rate? Yes, but there’s typically a delay. If you get adjuvant chemotherapy, your cancer tends to come back a year or a year and a half later. Toxicity is a real issue. Performance status plays [a role] a lot in terms of age, as well as just performance status. Preexisting diabetes and hearing issues I think play a role, too.
How do the National Comprehensive Cancer Network (NCCN) guidelines recommend treating a patient like this?
AKERLEY: The NCCN gives guidelines [on the adjuvant treatment of stage I to III non–small cell lung cancer (NSCLC)]. For stage I, which is low risk, it is observation. For those with stage IB, it’s worth considering treatment with chemotherapy. For stages II and III, you should be going forward with chemotherapy as a category 1 recommendation. Of the high-risk features in stage IB that might push you one way or another, visceral pleural invasion is perhaps the dominant one.1 You should look for reasons to not give chemotherapy rather than to give chemotherapy. I think our default position with risky cancers should be to go forward with chemotherapy. In summary, risk features include tumors greater than 4 cm, vascular invasion, poorly differentiated tumors, visceral pleural invasion, wedge resection where cancer might not have been adequately sampled, and patients with unknown lymph node status.1
Which parameters are important when deciding whether to add adjuvant radiation therapy?
AKERLEY: The important parameters when deciding whether to add adjuvant radiation therapy are controversial. Tumor size, what you do for tumors less than 4 cm; resection, R0 vs R1; N2 disease; and which patients should be referred [to radiation oncology for evaluation should be discussed.]
CHOWDHARY: Tumor size is not something I routinely [base my decisions] on. I think the PORT [postoperative radiotherapy] analysis was clear on resection status, but if it’s an R1 I send it to the radiation oncologists for evaluation. Even with N2 disease, we discuss the matter at our thoracic tumor board, then refer the patient. I have to say, [based on] the extremely compelling data from the LUNG ART study [NCT00410683]—which I know is a single study and not all radiation oncologists in Cleveland, Ohio, are convinced whether the lack of benefit in N2 disease is real or not—chemotherapy is much more important than radiotherapy. I think chemotherapy needs to be at least your primary mode of treatment.
I still feel that adjuvant chemotherapy for lung cancer, given the high-risk nature of the disease, is very important. The relative risk reduction is 20% to 30%; the absolute benefit, certainly, is at least in most cases 5% to 6% but can be as high as 9% to 10%. I feel like when we accept a 5% to 6% absolute benefit for breast cancer, we should be really doing that for lung cancer as well because a lung cancer recurrence is much worse, in general, than a breast cancer recurrence. That’s why, to me, the chemotherapy is still very important. I don’t know if at your institutions you have moved away completely from radiation therapy in the adjuvant setting for N2 disease? I know we’re seriously looking at that in our institution and having discussions with every patient.
SRIVASTAVA: I’m at University of Colorado in Colorado Springs, and I think our radiation oncologists have been very impressed with the [LUNG ART study] and the trend has been to not offer radiation therapy for N2 disease after the data came out. So there definitely has been a decrease in adjuvant radiation in that setting. I agree, for positive margins, we have the discussion.
There are some N2 disease [cases] with a bit of bulky disease or just some high-risk feature that we may still have to meet with radiation oncology. A lot of patients are on forums and they hear and read about things, so it’s good for them to meet with radiation oncologists and go into a discussion with them, but I do feel that there has been a downward trend [in adjuvant radiation therapy] at our institution.
AKERLEY: Yes, I would say the same thing has happened with our group. The data for radiation goes back to the PORT analysis a long time ago. What it showed was that for stage I disease, you hurt patients and made outcomes worse. For stage II, it didn’t make a whole lot of difference, and for the high-risk patients, those with node-positive disease, you didn’t do any harm. Now, that got extrapolated into, “Well, it didn’t do any harm, and half the relapses are going to happen within the radiation port. Therefore, if I irradiate that mediastinum, then maybe I’ll do some good.” But it was not a definitive randomized study that said do it. It was a definitive randomized study that sort of said you’re not doing any harm. I think current data say we’re doing less good than we thought.
We mentioned risk reduction as high as 5% or 6% but if a patient has stage III cancer, you can find studies with risk of relapse approaching 90%. At a 90% risk of recurrence, and a 20% risk reduction, you’re approaching 18% absolute benefit. So again, the greater the risk of cancer, the more likely you are to benefit patients with adjuvant therapy. I think it’s reasonable to refer. The nice part about radiation is they get to hear both sides of the story, but the role is decreasing as time goes by.
The LUNG ART trial was a randomized study between control and a standard PORT of 54 Gy. This was a great study in the sense that the original data supporting use of it were a lack of harm rather than an addition of benefit.
The disease-free survival [DFS] by Kaplan-Meier curves had a P value that was less than .05.2 There was improvement with PORT and we said, “Well, half the relapses are going to show up there.” So you’re going to mask some of the relapses. But the deal is, if a patient relapses in their chest, they are likely to relapse somewhere else at the same time whether you can see it or not. The overall survival [OS] rate at 3 years was 68%, so no real difference.2 I think this is a game-changing study and I think it’s worth repeating it to our radiation oncologists whenever we can.
What do we know about adjuvant EGFR-targeted therapy?
AKERLEY: We have older data from the RADIANT study [NCT00373425], which was performed in an unselected population of patients. Investigators retrospectively went through the data and looked for those who had mutations and those who didn’t. So when adjuvant erlotinib [Tarceva] was given vs placebo in stages IB to IIIA, the DFS curves looked identical. However, when those with EGFR mutations were pulled out, the erlotinib was seen to at least affect the DFS curve. The second study is the SELECT study [NCT00567359], which was phase 2, not phase 3, [and] had the same argument for adjuvant erlotinib. These groups were given 3 years of adjuvant therapy in a single-arm study. The data looked reasonably good and largely showed feasibility that one can go ahead and do it.3 Another was gefitinib [Iressa] vs vinorelbine [Navelbine], which showed that there is an improvement in DFS with gefitinib, but does that tell us anything? It’s not entirely clear.
So we’ve been left with no clear guidance. When you were giving erlotinib as an adjuvant therapy, there was no clear evidence that you were improving cure rate. There was also a reasonable amount of toxicity. Those were the 2 features for arguing against. If you had cured the patient, you were treating a lot of patients and giving them toxicity without any proven benefit at the time. Now is the opportunity to go ahead and answer the question and be clear about an answer. We have randomized data that I believe will turn into real data.
The ADAURA study [NCT02511106] is a legitimate double-blinded, placebo-controlled, phase 3 study. [Patients recruited were] 18 years of age with good performance status.
They took only the 2 common EGFR mutations: exon 19 deletion and L858R. Brain imaging was required, you had to have a complete resection with negative margins, and the interval between surgery and randomization was 10 to 26 weeks, depending on whether you’d had adjuvant chemotherapy. These patients were stratified by stage, EGFR status, and age. They were treated with osimertinib [Tagrisso], 80 mg daily.4 The planned treatment duration was 3 years; treatment continued until disease recurrence, treatment completion, or discontinuation criteria were met. Patients were followed up [until recurrence] at weeks 12 and 24, then every 24 weeks for 5 years, then yearly. After recurrence, follow-up was every 24 weeks for 5 years, and then yearly.
The study was powered not for OS but for DFS by 2 groups. The primary end point was to look in those with higher risk (ie, stages II and IIIA). It was designed for superiority under the assumption that DFS would be improved by 30%. A secondary analysis was to just look at the overall patient population.4
Randomization, especially when you have 700 patients, promises that you will be evenly balanced. [For baseline characteristics in the ADAURA study], the median age is low 60s and they had an EGFR mutation, as we said, so there’s something a little different here. For typical NSCLC, you see [patients who are] 65, 67, and 68 years old. These patients were a couple of years younger.
Majority of the patients were never smokers. Race, performance status, and stages were evenly distributed between the [osimertinib and placebo arms and adenocarcinoma was the predominant histologic type in both arms].
I usually find EGFR exon 19 deletion much more common than L858R, but it was 56% and 44% in both groups, [respectively]. Physicians decided who would receive chemotherapy; 60% [of patients] had adjuvant chemotherapy and 40% of patients did not receive adjuvant therapy.5
At the interim analysis, the primary end point of DFS in both the stage II and III group and overall population were remarkably different. We have very few therapies that have a hazard ratio of 0.17 [99.06% CI, 0.11-0.26; P < .001], and 83% reduction of risk over the time that we’ve looked at. This is starting to get into the penicillin world if one measures this by DFS. For the overall population that included patients with stage IB cancer, risk reduction is nearly 80% [HR, 0.20; 99.12% CI, 0.14-0.30; P < .001]. Again, tremendous improvements in DFS.5
Based on the forest plot, there was overall improvement through all categories and it benefited males, both younger or older, and smoking or nonsmoking. Race didn’t make a difference; stage maybe showed a trend but all of them benefited. Both EGFR types benefited and those who received adjuvant chemotherapy or not. All groups appeared to benefit. So there wasn’t a particular group you needed to target.5
Based on the forest plot you had some sense that the greater the risk, the greater the benefit. In the group with stage IB that had all patients, hazard ratio was 0.39 [95% CI, 0.18-0.76]. The group with patients with stage II cancer had a hazard ratio of 0.17 [95% CI, 0.08-0.31] and for stage III hazard ratio was 0.12 [95% CI, 0.70-0.20] and approaching [a risk reduction of] 88% to 90% if you limited it to stage IIIA only.5
Osimertinib is a unique drug in the sense that it’s an irreversible binder. There isn’t a huge concentration of drug in the CNS [central nervous system], but the little bit that does get there has an effect, and certainly in metastatic cancer. In terms of CNS DFS, there is a benefit. So this drug does get to CNS disease and there is a statistically significant improvement in terms of CNS risk. [The median CNS DFS was not reached for osimertinib and was 48.2 months for placebo (HR, 0.18; 95% CI, 0.10-0.33)].5
The OS is perhaps the only weakness of the study. But when you look at the stage II and III groups, there is a difference by hazard ratio, and I guess the hazard ratio has matured enough. There’s updated data that suggest there is an improvement in OS.4
The challenge to these data is the censored data that have not reached 2 years, so these data are still felt to be immature. We’ll have an answer on whether OS has been impacted in the future. It’s quite possible that a patient may control their disease, as they would with metastatic disease, and ultimately they may relapse in the future. But clearly at this point there will be an improvement in DFS in the first 3 years.
For the safety summary, nothing was out of the ordinary. The placebo group vs the osimertinib group had grade 3 toxicity at 14% vs 20%. There weren’t any deaths. Serious adverse events [AEs] were 16% for osimertinib vs 13% for placebo. Discontinuation of the drug occurred in 4% of those on placebo [and 11% of those on osimertinib].
In the placebo group and osimertinib group there were quite a few casually related AEs, so toxicities weren’t necessarily out of the ordinary.4
Diarrhea occurred in 19% of people in the placebo group and the number was double in the treatment group. Paronychia, which is a very specific AE with osimertinib, occurred in 25% of patients in the treatment group. Skin-related issues [were more in the treatment group]. Cough was almost equal in both groups. Otherwise, AEs weren’t really all that different from what one would have expected.4
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. Non-small cell lung cancer, version 6.2021. Accessed October 11, 2021. https://bit.ly/30l9kaG
2. Le Pechoux C, Pourel N, Barlesi F, et al. LBA3_PR An international randomized trial, comparing post-operative conformal radiotherapy (PORT) to no PORT, in patients with completely resected non-small cell lung cancer (NSCLC) and mediastinal N2 involvement: primary end-point analysis of LungART (IFCT- 0503, UK NCRI, SAKK) NCT00410683. Ann Oncol. 2020;31(suppl 4):S1178. doi:10.1016/j.annonc.2020.08.2280
4. Spigel DR. Discussion of LBA5. Presented at: 2020 ASCO Virtual Scientific Program; June 1-4, 2020; virtual. Accessed October 11, 2021. https://www. bit.ly/38gIEd8
5. Herbst RS, Tsuboi M, John T, et al. Osimertinib as adjuvant therapy in patients (pts) with stage IB-IIIA EGFR mutation positive (EGFRm) NSCLC after complete tumor resection: ADAURA. J Clin Oncol. 2020;38(suppl 18):LBA5. doi:10.1200/JCO.2020.38.18_suppl.LBA5
6. Wu YL, Tsuboi M, He J, et al; ADAURA Investigators. Osimertinib in resected EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2020;383(18):1711- 1723. doi:10.1056/NEJMoa2027071
