Roundtable Discussion: Bryce Discusses Outcomes That Clinicians Should Aim for When Treating Patients With mCRPC
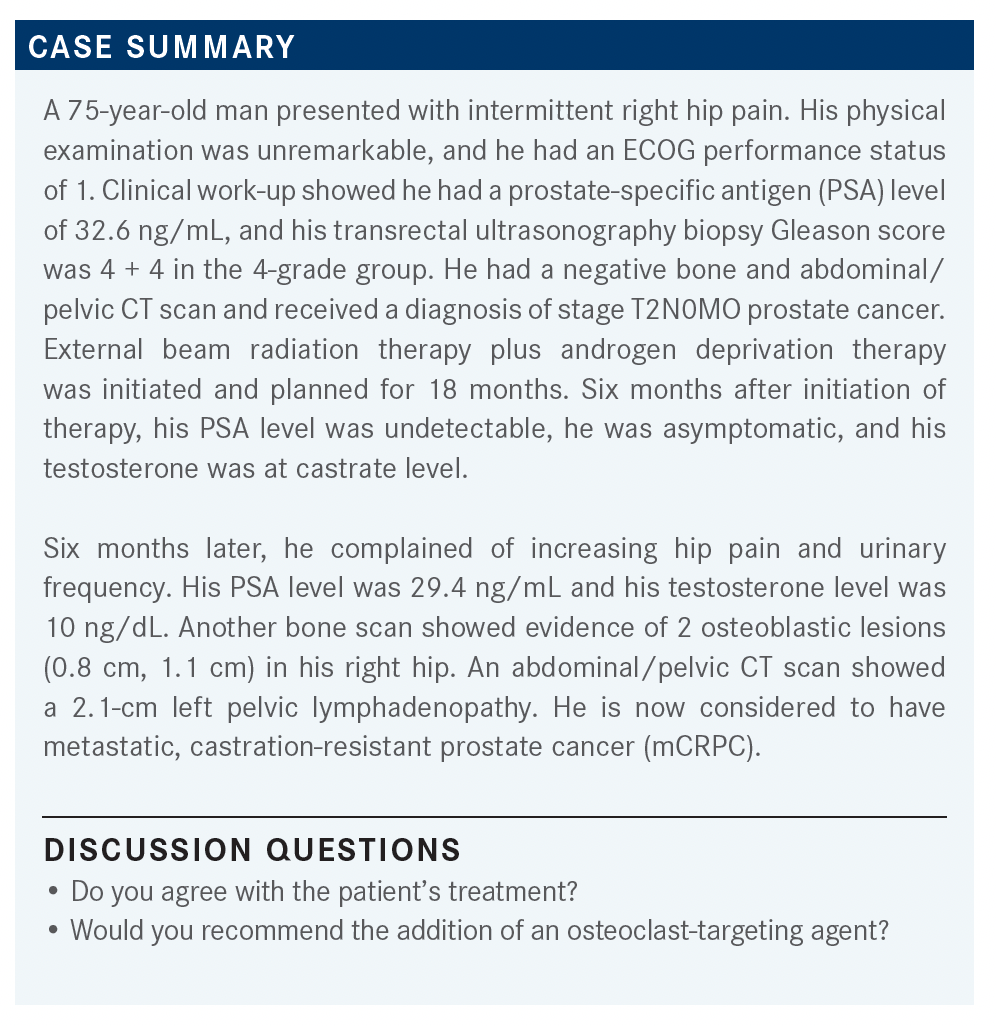
A 75-year-old patient with metastatic castration resistant prostate cancer experienced an increase hip pain and urinary frequency 12 months after external beam radiation therapy plus androgen deprivation therapy.
Alan H. Bryce, MD

Alan H. Bryce, MD, medical director, Genomic Oncology Clinic, Mayo Clinic Arizona moderated a Case-Based Roundtable event during which he and participants discussed the case of a 75-year-old man with metastatic castration resistant prostate cancer.
CHANDAR: I usually discuss the options of abiraterone [Zytiga] and docetaxel with the patients. My patient population tends to be a more elderly population, and I think for the most part [patients] favor trying an oral agent in the first line, and the adverse events [AEs] profile seems to be more tolerable for most [patients]. If it’s a younger patient, I might favor docetaxel up front, but for most of my patients, I usually go for abiraterone in the frontline, and then I might use enzalutamide [Xtandi] a little bit later.
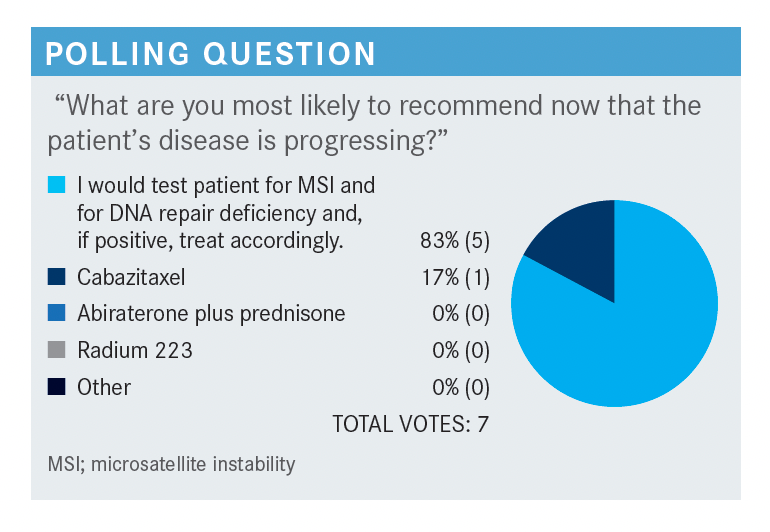
BOMGAARS: I picked mutational testing to see if there are other treatment options [for this patient]. The patient pretty much relapsed quickly after enzalutamide and then after chemotherapy, so I would want to see what other options I would have for treatment. With him relapsing so quickly, and then having toxicity with the docetaxel, too, he could run into similar issues with both of those options.
BRYCE: In terms of getting genetic testing, what kind of testing would you order in this situation?
BOMGAARS: I usually use FoundationOne, Caris [Life Sciences], or [a test] similar to those.
BRYCE: Do you ever go back and use the primary tumor or cell-free DNA [testing if you] can’t get a biopsy? How do you approach that?
BOMGAARS: I usually try to biopsy the metastatic site.
BRYCE: How about the person who voted for the use of cabazitaxel [Jevtana]? Can you walk us through how you approach [a patient such as this]?
GOLDFARB: I would probably check for BRCA [mutations in this patient] before I would check for MSI [microsatellite instability]. I think PARP inhibitors would be more important than a PD-L1 inhibitor, as well.
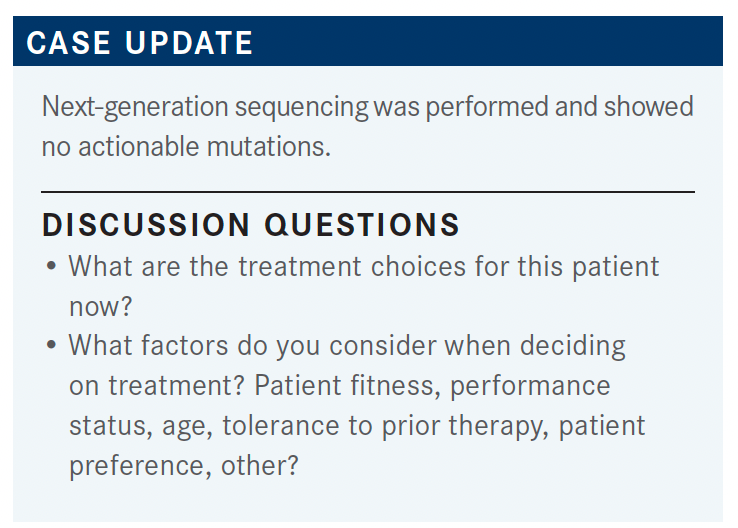
BRYCE: Genetic testing is key, and it’s worthwhile remembering that for [patients with] high-risk or metastatic prostate cancer it is recommended that they get germline testing. So, this gentleman had a Gleason score of 8 [when he received his] initial diagnosis and qualified as high risk. It would have been appropriate to get germline testing at that point. I get germline testing for almost all my patients from the first visit…and I like to repeat testing with each line of therapy, because we do see that the genetic signature evolves, and there are multiple opportunities to go on a different path.
BOMGAARS: Do you do both germline and somatic mutation testing? Or do you just do 1?
BRYCE: No, I usually get germline right in the beginning. For this patient, I wouldn’t have done somatic testing at that point, but I would do germline early, because there’s the familial component and the germline information is still valuable. Somewhere between 10% and15% of all patients with [advanced] prostate cancer will carry some germline predisposition to cancer. So even if I find Lynch syndrome, and I’ve found several in my practice, knowing that their family [members are] getting colonoscopies early and the women are getting checked for endometriosis, I mean that’s a win [for me]. I still think the nightmare scenario is that a patient walks in and says, “My 30-year-old daughter just [received a diagnosis of] metastatic ovarian cancer. She’s BRCA-positive; why didn’t you check me?” I don’t think any of us ever wants to be on that side of that conversation.
Patients who start out with quiet somatic testing, or unimpressive somatic testing [and are found to be] non–BRCA-mutated early then develop BRCA mutations later—that’s why I retest patients. Even if I happen to look at the first line when they have castration-resistant prostate cancer, and here we are 2 lines of therapy later, they may well have developed a BRCA mutation in the meantime, or that clone that maybe was hiding in the background may well be dominant at this time.
BANS: [If this patient] didn’t have nodal disease and it was just bone disease, how do you assess him at that point? Do you do bone biopsies or do you do liquid biopsies?
BRYCE: I do cell-free DNA testing. I generally don’t like bone biopsies because the yield drops off significantly. And the way prostate cancer infiltrates bone, it generally spreads throughout the bone anyway. There’s not a real high tumor cellularity, right? Even if you get a good biopsy, you might not get enough DNA content.
Therefore, I do cell-free DNA testing, and the key to cell-free DNA testing is that a positive signal is real. Positive is positive. The multiple data sets have shown the correlation in the tissue. When you find something in cell-free DNA, it really is what’s in the tissue as well. The problem is that negative is not negative. Cell-free DNA tests depend on the amount of the fraction of DNA that’s circulating. If it happens to fall below the threshold of detection, the test will read out as negative.
BANS: What company or companies do you use for the standard circulating cell-free testing?
BRYCE: I use Guardant [Health] most often, just because they were first, and [I’m] used to using them. FoundationOne has a test now, and other companies have a test, but the biggest difference between the various companies oftentimes is that all they’re doing is manipulating the threshold for their variant calling. This isn’t the better test and it’s just a subjective decision. But I mostly use Guardant out of habit, and I don’t think there’s anything wrong with the other big companies.
The other point I’d make about the cell-free DNA testing is that because it’s dependent on DNA fraction in the serum, it only makes sense to test when the disease is progressing, tumors are growing, or the DNA fraction is maximal. It doesn’t make sense to test it when the patient’s responding. You don’t get it 6 months in advance of when you need it. Turnaround time on these tests is generally less than 2 weeks, so you’re usually able to go ahead and order it when the patient’s progressing, and then bring them back 10 days later to talk about the results.
SUD: I would say cabazitaxel [is the next treatment choice] if the patient’s fitness and performance status are good enough. He has some response to docetaxel, and I understand that he has some neuropathy, but if he can tolerate cabazitaxel then I would try that.
BRYCE: What about going to the other oral drug? I guess you could do abiraterone in the first line, going to enzalutamide, or if you do enzalutamide in the first line, then go to abiraterone. But what are [patients’] experiences with that?
SUD: I’m not aware of any data. You can probably speak to that more, but I have not seen much in the form of a response when you move from one hormone blocking agent to another.
BRYCE: The overlap, despite the fact [that abiraterone and enzalutamide] have different mechanisms of action, they’re only 1 step removed on the androgen receptor [AR] stimulation pathway. Generally, resistance to 1 drug leads to resistance to the other, and it doesn’t matter which order you put them in, the first drug does well, the second drug does poorly. Not that it doesn’t get it done, but we’ve seen the real-world data, and going from 1 oral agent to the other is the dominant pattern. Cabazitaxel, ultimately, is only being used in 10% to 15% of all patients with prostate cancer, and even docetaxel [is being used in] only 40% to 50%.
CHANDAR: I agree that cabazitaxel is the next appropriate step for a medically fit patient. I think the neuropathy certainly is the consideration, and fitness for chemotherapy. I think a lot of patients are not enthusiastic about the idea of further chemotherapy in this situation. I don’t think that there are [many reasons] at some points [to] go to another oral agent, [such as] enzalutamide or abiraterone. If they hadn’t received it previously, the responses do tend to be short-lived.
BRYCE: [These are], without a doubt, the landmark data in this space. When I’m talking with the FDA about other studies, the CARD data are heavily cited. This really is the standard of care, right? [It is] saying chemotherapy rather than another oral agent is the most effective option.
The more effective drug is the drug that leads to better quality of life [QOL]. The toxicity of the therapy notwithstanding, QOL is higher when we control the cancer and QOL is lower when we give less-effective therapy. [This is true] even when we think we’re doing the patient a favor by giving them the less toxic drug, because they just don’t feel well when the cancer’s getting worse. That’s the point of the QOL data, to really validate that we are still taking care of QOL when we’re pursuing that more aggressive drug for OS.
KAHN: In my experience, a lot of patients prefer, if possible, to go with an oral option because they don’t want to leave their home.
BRYCE: Without question. Patient convenience is part of [treatment and those discussions with patients].
KAHN: The problem is, basically, cabazitaxel is not something they can get in an oral regimen. That’s part of the problem.
BRYCE: What’s your approach in managing toxicities associated with cabazitaxel treatment?
KAHN: We give [patients] a handout that describes all about the drug. We tell them what to expect and then tell them that we don’t know how they’ll do. We tell them what to watch out for and to take it depending on how they do. We basically tell them to do a wait-and-see approach, but I warn them about things that we’ll look out for as well.
BOMGAARS: A lot of patients like the oral route. [However, not as much anymore] since the COVID-19 vaccination has taken off, but I would say patients are still hesitant with chemotherapy because they think that they’re going to be more immune compromised, and therefore have a higher risk of contracting an infection, especially COVID-19. I think it’s not the oral [therapy option] vs the intravenous route, but it’s more that they think that they’re going to be more immune compromised [because of the treatment].
REFERENCE:
Fizazi K, Kramer G, Eymard JC, et al. Quality of life in patients with metastatic prostate cancer following treatment with cabazitaxel versus abiraterone or enzalutamide (CARD): an analysis of a randomised, multicentre, open-label, phase 4 study. Lancet Oncol. 2020;21(11):1513-1525. doi:10.1016/S1470-2045(20)30449-6

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More