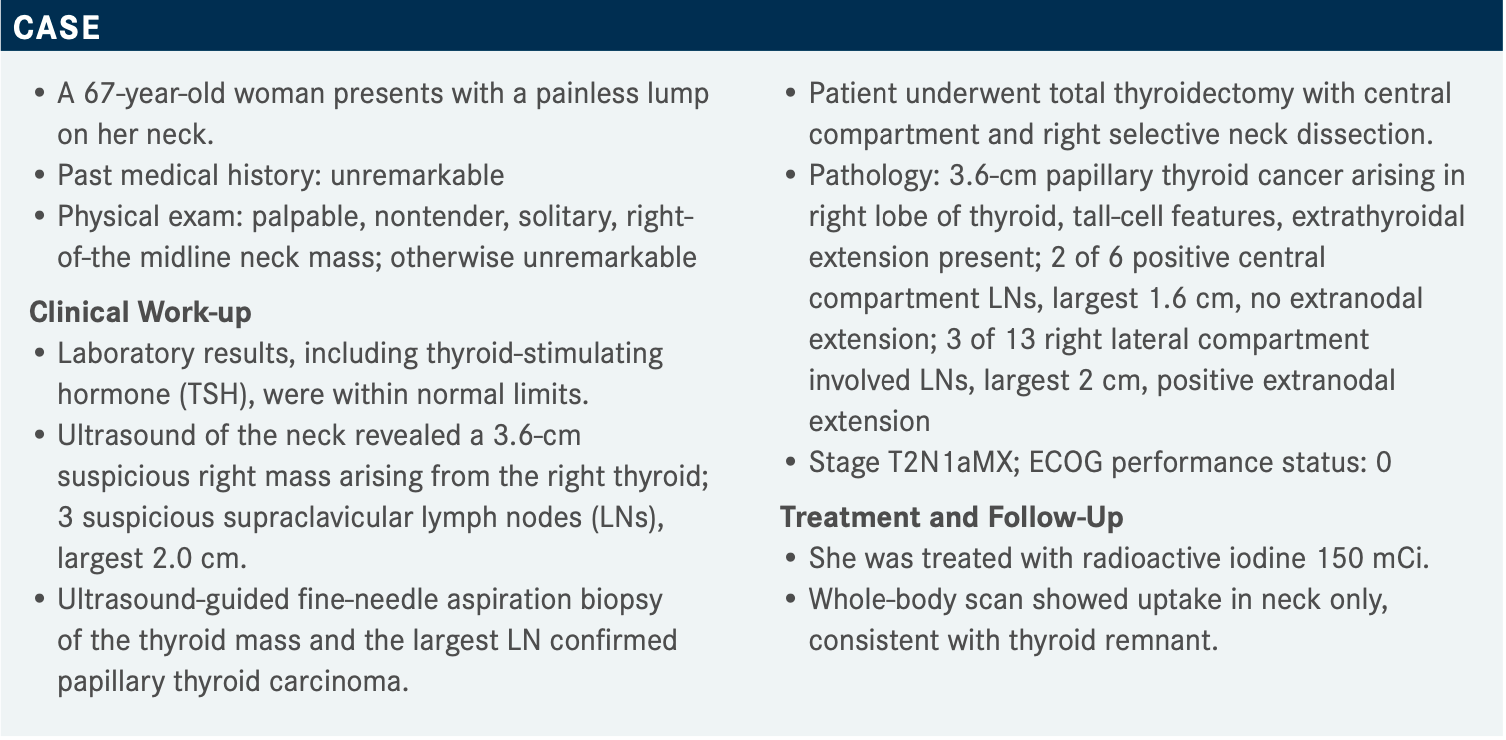
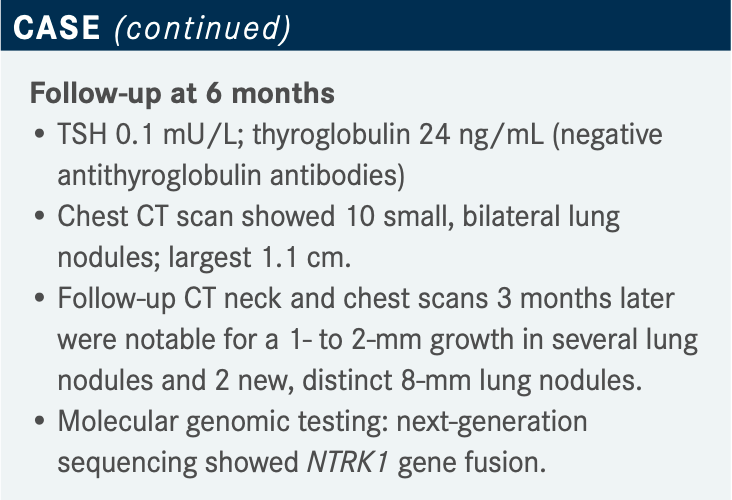
Misiukiewicz Describes Decision-Making for NTRK Inhibitors in Thyroid Cancer
During a Targeted Oncology case-based roundtable event, Krzysztof J. Misiukiewicz, MD, discussed deciding to use NTRK inhibitor for the treatment of a 67-year-old woman with thyroid cancer.
Targeted OncologyTM: What do the NCCN (National Comprehensive Cancer Network) guidelines recommend for treatment of metastatic papillary carcinoma that is not amenable to radioactive iodine?
MISIUKIEWICZ: The NCCN guidelines recommend lenvatinib [Lenvima] and sorafenib [Nexavar]. Lenvatinib is preferred based on the high response rate, which is 65% vs 12% for sorafenib, or [for] any iodine-refractory progressive radiographically differentiated thyroid cancer, or if the patient has symptoms.1
Larotrectinib [Vitrakvi] and entrectinib [Rozlytrek] are the 2 NTRK inhibitors for gene fusion–positive disease, so [the patient] must have those mutations. Selpercatinib [Retevmo] and pralsetinib [Gavreto] are reserved for RET fusion–positive disease. Pembrolizumab [Keytruda] can be used if the TMB [tumor mutational burden] is high, but I do use pembrolizumab as a systemic therapy.
I have a tendency not to use chemotherapy in thyroid cancer because it’s not very effective and [it is] toxic. A clinical trial is always the correct answer. Obviously, there are unique situations. If I have a patient with 10 lesions and 1 of them is not responding, I would consider local treatment; it could be resection, stereotactic radiation, or any other kind of localized therapy.1 Disease monitoring is absolutely a good option too [for asymptomatic, indolent disease with no brain metastases], and best supportive care [is always appropriate].
What should influence the recommendation of an NTRK inhibitor over lenvatinib in a case like this, and what do you consider when recommending an NTRK inhibitor?
I would say there are no data comparing lenvatinib to NTRK inhibitors, and obviously we don’t have any evidence. There’s no evidence [lenvatinib] should be reserved for the first and second line, but my preference is [to use it because] (1) it’s effective, (2) there aren’t too many adverse effects, and (3) it provides the patient with a good quality of life.
A good quality of life can be [provided by] an oral drug; [those are] always preferred over any intravenously given ence]. Obviously there are unique situations, and NTRK inhibitors have the capacity to [treat] brain lesions. This is [a class of drug] that I would strongly consider in a situation [where brain lesions are involved], but yes, you must have the mutation and you cannot use [NTRK inhibitors solely] because [a patient] has brain lesions.
Mutational profile, convenience, quality of life, patient satisfaction, and financial toxicity [are all things I consider]. Larotrectinib is an FDA-approved drug, and I’ve never had a problem having this drug approved [for treatment], but I’m not shy; whenever I had any problems I would reach out to the company. My personal experience is most of those companies have very good patient assistance programs, many times with zero copayments, so I would encourage [others to pursue that option as well]. Patient factors and preference [are considered,] but usually it’s a medically driven decision.
Which end points are the most important in considering an NTRK inhibitor?
In the first-line setting, I would say progression-free survival [PFS] and objective response. Time to response [is also important], especially for symptomatic patients, and duration of response; obviously, you want to maintain the response.
What are the most important considerations in terms of toxicity and the overall safety profile of NTRK inhibitors?
I pay attention to treatment discontinuation and dose reductions and omissions. [These events] tell me that this drug is toxic, and any toxicity is going to be in the grade 3/4/5 category, which can be alarming.
What are the data that support the use of larotrectinib in a case like this?
Larotrectinib was FDA approved based on 3 studies. There was a phase 1 adult [study] with 8 patients, there was a pediatric study, and then there was a phase 2 basket trial with 35 patients.2 All of those patients had to have NTRK gene fusions. The primary end point of those studies was best objective response assessed by RECIST criteria, and secondary end points were the duration of the response, PFS, and safety. The approved dose for larotrectinib is a 100-mg capsule given twice a day.3 There is also a liquid pediatric form that can be considered in patients who have difficulty swallowing. Treatment was allowed even after the patient progressed if the investigator found that there was a benefit of continuing the treatment.2
So, most of the patients did respond to the treatment, and this was a population of patients with different illnesses.4 Even though the [focus of the trials was] thyroid cancer, [there were also patients with] pancreatic cancer, melanoma, soft tissue sarcoma. Some of these cancer types, like cholangiocarcinoma and bone sarcoma, are very aggressive; [nonetheless], they responded to the treatment.
Larotrectinib has a tissue-agnostic indication.3 If the patient has any of [the previously mentioned cancers] and has [an NTRK gene fusion] mutation [without a known acquired resistance mutation], this drug can be used. The objective response rate seen in [121 of 153] patients was about 79% [95% CI, 72%-85%].4 The [mean] duration of response was 35 months [95% CI, 22.8-NE], and the safety profile was very tolerable. Within the [overall cohort], there were 24 patients with thyroid cancer, and their response rate was 79% [95% CI, 58%-93%]. The median duration of the response was not reported. So, [there was an] excellent response in thyroid cancer patients.
In terms of patient characteristics, most of them had received at least 1 prior treatment.4 The most common NTRK fusion genes were NTRK1 and NTRK3. NTRK2 is not commonly seen. Most of the patients had received systemic therapy, such as radiotherapy, and most had good performance status. But some patients had poor performance status, and they were also included. Thyroid [cancer] was seen in about 19% of the patients, so [that patient population was] represented in this study.
Are there updated results with this therapy to discuss?
Yes, the updated [analysis in an expanded cohort of 130 adult patients with TRK fusion cancers] showed an overall response rate of 67% [95% CI, 58%-75%].5 There were 19 patients with brain metastases, and the response rate [in that subset] was 73%, [which] was high. The patients with thyroid cancer all responded, [except those who had] anaplastic thyroid cancer. Seven of the patients had anaplastic thyroid cancer, and their response rate was only 29%; all of them progressed.
So, this treatment does work in anaplastic thyroid cancer, but the response is not as robust as we see in differentiated thyroid cancers. The response rate [when considering only patients with differentiated thyroid cancer, including papillary and follicular thyroid carcinoma,] was 86%. All the patients who had differentiated thyroid cancer or brain metastases responded. This was a remarkable response, and in [patients with cancers of] other histologies, the response was similar. So, overall, larotrectinib is a very effective treatment.
Most of the patients [with thyroid cancer] continued the treatment.5 There was a difference in the duration of the response and PFS between patients with and without brain metastases. However, patients with brain metastases still responded, so I think this is a very active treatment in that population.
What is the safety profile for larotrectinib?
[In terms of] adverse events [AEs], larotrectinib is very well tolerated; [the most common treatment-related grade 3 or 4 AE was elevated alanine transaminase (ALT)].3,5 There was some dizziness [reported] as well. I have some patients who have fatigue, and there is some weight gain, but other than that, it’s extremely well tolerated. There was 1 patient who discontinued [treatment] because of liver enzyme elevation, but the rest of the patients were able to continue with the drug, so overall, I think it’s a very well-tolerated medication.
The updated data on larotrectinib [evaluated the long-term efficacy and safety of larotrectinib in an integrated dataset of patients, including those with TRK fusion cancer] in both the primary and supplementary data from the studies that we have seen.6 The data set included about 218 patients with TRK gene fusions, and as we discussed, this drug was given at a dose of a 100-mg capsule twice a day. There was also a pediatric dose, which was important because it’s a liquid. So, the [patient breakdown by type of cancer revealed] predominantly soft tissue sarcoma and fibrous sarcoma, 20% and 26% [respectively], and thyroid cancer was represented with 13% of the cases. The distributions of the patients and characteristics were very similar to the previous data we just discussed, but there were no [substantial] differences.
In the [integrated data set, the] tumor response in thyroid cancer was the same.6 So, patients with anaplastic thyroid cancer did not respond, but all of those with differentiated thyroid cancer responded. [And there was a] tremendous response even in soft tissue sarcoma, fibrous sarcoma, and salivary gland, lung, and other cancers. The overall response rate [was] 75% [95% CI, 68%-81%]. [In patients who had] CNS [central nervous system] metastases, [the overall response rate was] 73% [95% CI, 45%-92%].
The duration of the treatment [went to] almost 6 months, which is a long time.6 The median time to response was no longer than 2 months. I had a patient whom I started [on an] NTRK inhibitor who had lesions on the skin, and it was very encouraging to see that she was responding; so yes, I can confirm that this drug can work quickly. At the data cutoff, 50% of the patients were still on the treatment.
The duration of response [was] astonishing; [it was] almost 50 months [95% CI, 27.3-NE]. The PFS was 35 months [95% CI, 23.4-55.7], and median overall survival [OS] was not reached.6 It’s astonishing, especially if you consider that this drug is minimally toxic, [with AEs] mostly consisting of [elevated liver enzymes]. This is something that we don’t see commonly in medical oncology; I think the results are remarkable.
Regarding safety, there were no additional concerning signals different from the previous [data].6 Again, there were few discontinuations [due to treatment-related AEs]; just 2% of the patients. Grade 3 and 4 AEs were reported in about 18% of the patients; they were mostly liver enzyme [elevations] and lab based. Overall, larotrectinib was a very well-tolerated treatment.
What are the data that support the use of entrectinib in a patient case like this one?
Entrectinib [was evaluated in a trial with a] similar design, an aggregate study. The drug was given once a day as a 600-mg dose. [The trial enrolled] 68 [patients who] were receiving this treatment, and the end points were very similar to the previous design.7
In the initial report, thyroid cancer was not heavily represented; they only had 5 cases, [and] the response rate reported in that group was only 20%. But again, it wasn’t a direct, head-to-head comparison of larotrectinib and entrectinib. This is just the first report, so I’m not trying to [convince] you that one is better than the other. You can draw your own conclusions. The duration of the response was about 10 months, and the drug was well tolerated.7 But a response was seen in only 1 out of 5 patients with thyroid cancer.
[However,] there was a subsequent update. They reported results for 13 patients with thyroid cancer, and 7 of them responded, so the response rate was about 53%.8 The patient characteristics [were] very similar to the characteristics seen in the larotrectinib study in terms of performance status, race, and sex. Most had received some previous treatment. There were some patients with brain metastases.
Response rates were calculated for both the entire population and the subset of patients with CNS metastases. The [overall] response rate in the entire population was 61.2% [95% CI, 51.9%-69.9%]; [in patients] with CNS [metastases], it was 57.7% [95% CI, 36.9%-76.7%]. The median time to response was 1 month. Many different types of cancer were seen [in this study,] and most of these patients responded, which I think is remarkable.
[A response] in patients with thyroid cancer was seen in 7 of 13 patients; the rate was 53% [95% CI, 25.1%-80.8%], and the duration of response was 13 months [95% CI, 7.9-NE]. In terms of AEs, results were very similar to what we saw with larotrectinib.8 There were some aspartate aminotransferase/ALT abnormalities, diarrhea, weight increase, and fatigue, but not significantly different.
How do the data compare between entrectinib and larotrectinib?
[Entrectinib and larotrectinib] were not compared head-to-head, so I don’t want you to draw any conclusions, but the sample sizes were very similar.7,8 The median follow-up and patient distributions were also very similar. There were slightly more patients with CNS metastases in the entrectinib study than in the larotrectinib trial.
Theoverall response rate for the entire population was 67% for larotrectinib and 61% for entrectinib.7,8 The duration of response was 49 months for larotrectinib [95% CI, 26.3- NE] and only 20 months for entrectinib [95% CI, 13.0-38.2], with similar median follow-up. The median time to response was better for entrectinib; it was just 1 month vs 1.8 months for larotrectinib. The PFS results favored larotrectinib, with 25 months [95% CI, 12.7-51.1] vs 13 months [95% CI, 10.1-19.9]. OS was not reached with larotrectinib, [and] it was 33 months with entrectinib [95% CI, 23.4-46.4].
The response rate in patients with CNS involvement was 73% for larotrectinib [95% CI, 45%-92%] and 57.7% for entrectinib [95% CI, 36.9%-76.7%], but again, this was not a direct, head-to-head comparison. I would call larotrectinib a cleaner drug because it targets only the NTRK mutation. Entrectinib has approval in [patients with ALK mutations,] and it’s just not as clean as larotrectinib; that may explain some of the toxicity.9
In terms of the formulation, larotrectinib comes as a 100-mg [capsule and a] 25-mg capsule [and in a liquid]; it’s given twice a day.3 Entrectinib only comes in a [100-mg and 200-mg] capsule, but it’s given once a day.9 I think having the oral solution helps because you may have some patients who have a PEG [percutaneous endoscopic gastrostomy] tube, and [others have] difficulty swallowing, so I think having the oral solution does help.
Both treatments have skeletal fracture risk; I just wanted to point that out.3,9 Entrectinib is also associated with QT prolongation.9 Patients with thyroid cancer must maintain TSH suppression, so they are often on high-dose levothyroxine [Synthroid], which makes them prone to arrhythmia, palpitations, tachycardia. So, I’d be a little bit concerned having somebody on high-dose levothyroxine and at the same time giving them entrectinib and causing possible QT prolongation.
Some AEs that are unique to entrectinib include some reported cognitive impairment, increased weight, and visual problems.9 This is something that concerns me a little bit, and I don’t know why we see those AEs with entrectinib but not larotrectinib. I wanted to point this out, but [I would let clinicians] draw their own conclusions regarding which drug they favor. Entrectinib is given once a day and larotrectinib is twice a day, so some people may prefer entrectinib for this reason.3,9 However, there is a slight difference in terms of AEs that, in my opinion, favors [the use] of larotrectinib.
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 1.2022. Accessed April 6, 2022. https://bit.ly/3saPqdi
2. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in TRK fusion- positive cancers in adults and children. N Engl J Med. 2018;378(8):731-739. doi:10.1056/NEJMoa1714448
3. Vitrakvi. Prescribing information. Bayer HealthCare Pharmaceuticals Inc; 2021. Accessed April 6, 2022. https://bit.ly/3w84zxv
4. Hong DS, DuBois SG, Kummar S, et al. Larotrectinib in patients with TRK fusion- positive solid tumours: a pooled analysis of three phase 1/2 clinical trials. Lancet Oncol. 2020;21(4):531-540. doi:10.1016/S1470-2045(19)30856-3
5. Brose MS, Shen L, Tan DSW, et al. Larotrectinib efficacy and safety in adult patients with tropomyosin receptor kinase (TRK) fusion cancer. Ann Oncol. 2021;32(suppl 5):S600-S601. doi:10.1016/j.annonc.2021.08.1057
6. Hong DS, Shen L, van Tilburg CM, et al. Long-term efficacy and safety of larotrec- tinib in an integrated dataset of patients with TRK fusion cancer. J Clin Oncol. 2021;39(suppl 15):3108-3108. doi:10.1200/JCO.2021.39.15_suppl.3108
7. Doebele RC, Drilon A, Paz-Ares L, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1-2 trials. Lancet Oncol. 2020;21(2):271-282. doi:10.1016/S1470-2045(19)30691-6
8. Bazhenova L, Liu SV, Lin JJ, et al. Efficacy and safety of entrectinib in patients with locally advanced/metastatic NTRK fusion-positive (NTRK-fp) solid tumours. Ann Oncol. 2021;32(suppl 5):S598-S599. doi:10.1016/j.annonc.2021.08.1055
9. Rozlytrek. Prescribing information. Genentech Inc; 2021. Accessed April 6, 2022. https://bit.ly/3OXPyGR
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen