Singal and Kim Talk Trials and Treatments for HCC
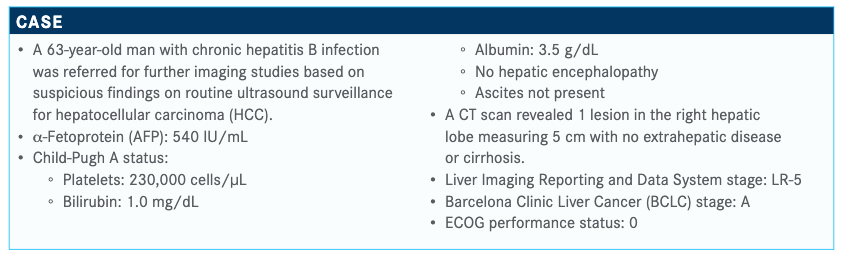
Amit Singal, MD, MS, and Richard Kim, MD, discussed the case of a 63-year-old male patient with hepatocellular carcinoma.

Amit Singal, MD, MS, medical director, Liver Tumor Program Clinical Chief, Hepatology The University of Texas Southwestern Medical Center, and Richard Kim, MD, assistant professor, Oncology University of South Florida College of Medicine Moffitt Cancer Center, discussed the case of a 63-year-old male patient with hepatocellular carcinoma (HCC).
Targeted Oncology™: What would be the best course of treatment for this patient at this time?
SINGAL: [Because] this patient has good liver function, good performance status, and limited tumor burden, he would be a patient with [early-stage disease], would fall into BCLC stage A, and is therefore eligible for curative treatments. [Because] he has a single tumor and no portal hypertension, this patient was treated with resection, and his AFP [level] came down from [greater than] 500 IU/mL all the way to the normal [level].
What options are available to the patient following progression?
SINGAL: Unfortunately, there is a high risk of recurrence. Even though resection is curative, the risk of recurrence is about 70% at 5 years. This patient was followed and had a new lesion in his liver that was 2.3 cm and consistent with HCC. The high AFP [level] was a negative prognostic sign going into initial surgery, so his risk of recurrence was higher.
I think a clinical trial is never the wrong answer. This is a cancer for which we have made progress [in treatment], but I think we need to continue making progress. I think that both lenvatinib [Lenvima] and sorafenib [Nexavar] are good options…and have a direct comparison in the REFLECT trial [NCT01761266].
[Most clinicians] are well aware of the data for sorafenib, which was approved about 13 years ago [for use in patients with HCC] based on the SHARP trial [NCT00105443]. The REFLECT trial was a global, randomized, phase 3 noninferiority study. There were many more patients than we’re used to seeing in other clinical trials, with more than 950 patients.1
In terms of the inclusion/exclusion criteria, they’re similar to [those of] other clinical trials in HCC. These are patients with advanced, unresectable HCC but otherwise good liver function with Child-Pugh A status and good performance status. The other thing that’s worth noting about the REFLECT trial was that it excluded patients with greater than 50% liver involvement. It excluded [patients] with main portal vein invasion or bile duct invasion. These patients who had more extensive disease were not included in the REFLECT trial.
Patients were randomized 1:1 to receive lenvatinib, given at its weight-based dosing of 8 mg for patients weighing less than 60 kg or 12 mg for patients weighing 60 kg or more. Patients were randomized to receive sorafenib at the standard dose of 400 mg twice daily.
The primary end point was overall survival [OS], and secondary end points included progression-free survival [PFS], time to progression, and response rates.
OS did not significantly differ between the 2 therapies, [as the 95% confidence interval for a hazard ratio of 0.92] crossed 1 [0.79- 1.06]. Lenvatinib was not superior to sorafenib, but remember this is a noninferiority study. The noninferiority margin was set at 1.08, so the confidence interval was below that. It was interpreted as a positive trial [such that] lenvatinib is noninferior to sorafenib.
When you look at the secondary end point, you see a significant improvement with lenvatinib compared with sorafenib. You see significantly longer PFS, at 7.4 versus 3.7 months, respectively [HR, 0.66; 95% CI, 0.57-0.77; P < .0001]. There was a significantly longer time to progression, at 8.9 versus 3.7 months, respectively [HR, 0.63; 95% CI, 0.53-0.73; P < .0001]. You also see nearly 3 times higher response rates…whether you use modified RECIST or RECIST.1
Does the adverse effect (AE) profile serve to further differentiate the 2 agents? SINGAL: There were AEs in both arms, but the AE profile did differ between lenvatinib and sorafenib. The key things that you see with lenvatinib include higher hypertension, proteinuria, and constitutional symptoms such as anorexia and fatigue than you see with sorafenib. You see significantly less hand-foot syndrome with lenvatinib than you do with sorafenib. Overall, when you look at grade 3 or higher AEs, it’s 3% with lenvatinib versus 11% with sorafenib. The discontinuation rates in the 2 arms based on AEs are similar, at 13% for lenvatinib versus 9% for sorafenib.1
Do you have any real-life practice insight into the difference between these 2 agents?
KIM: I’m not sure a lot of patients get 12 mg of lenvatinib. You see more biochemical response with lenvatinib and more tumor shrinkage [based on radiographic scans]. But tolerance wise, I have patients who cannot tolerate 8 mg who are going on 4 mg, so I think there is a different toxicity issue. I agree anecdotally, sorafenib is probably harder to tolerate, but there are patients who cannot tolerate even 4 mg of lenvatinib as well. I think by response efficacy, you do see more biochemical response and more radiographic response [with lenvatinib].
SINGAL: That’s our experience. We see nice drops in AFP with lenvatinib. We see some responses on imaging with lenvatinib and definitely higher than what we saw with sorafenib. But I don’t think it’s without any AEs. We’ve had a lot of patients who have had a tough time with their fatigue. We often have to go to an 8-mg dose even though they’re supposed to be on 12 mg. It’s nice to not have to deal with the hand-foot syndrome, but I think it’s also not a drug without any AEs. I had a couple of patients who had hepatic encephalopathy related to lenvatinib. I know this because we used it post transplant in a patient who has no reason to have hepatic encephalopathy, but he developed it after going on lenvatinib.
Can this patient be treated with an immunotherapy combination considering their medical history and performance status?
SINGAL: IMbrave150 [NCT03434379] is a global trial that took patients with advanced HCC, good performance status, and good liver function and used sorafenib as a comparator arm and was able to demonstrate superiority [with atezolizumab (Tecentriq) plus bevacizumab (Avastin)]. This is the first combination that has demonstrated superiority in the first line and now redefines the treatment landscape.
The patients were randomized 2:1 to receive atezolizumab 1200 mg intravenously every 3 weeks plus bevacizumab at 15 mg/kg every 3 weeks or sorafenib at its standard dose. Of note here, all patients once again had liver function. All patients were required to undergo an upper endoscopy within 6 months of the trial to make sure they had either no varices or good control of their varices prior to being randomized, given the risk of bleeding. The trial had coprimary end points of OS and PFS.
In short, IMbrave150 ended early. It hit both end points at its first interim analysis. At the first interim analysis, median OS in the sorafenib arm was 13.2 months versus not reached in the atezolizumab and bevacizumab arm. When you look at 6-month survival rates, you can see 85% versus 72% [for the combination versus the control, respectively,] and once again a significant reduction in mortality. The hazard ratio was 0.58 with an upper limit in terms of confidence interval of 0.79.
Likewise, PFS was significantly different between the 2 arms. Median PFS was 6.8 months with atezolizumab plus bevacizumab versus 4.3 months. You can see the 6-month PFS rates were 55% and 37%, respectively, with a 41% reduction [in the risk of disease progression or death (HR, 0.59; 95% CI, 0.47-0.76; P < .0001)]. This trial hit both coprimary end points on its first interim analysis, [and these findings were further supported by data presented at the 2020 American Society of Clinical Oncology Virtual Scientific Program].3
This has been…FDA approved [based on these data]. This will redefine and reestablish what should be standard first-line therapy outside a clinical trial for all patients with HCC in the advanced-stage setting.4
What would you recommend currently in terms of second-line therapy?
SINGAL: The nice thing is that there’s no wrong answer. The only wrong answer would be not to treat the patient at all. The RESORCE trial [NCT01774344] was a randomized trial of regorafenib [Stivarga] as second-line therapy. Patients were treated after sorafenib. One of the key things about this trial was that patients had to be tolerant of sorafenib, so they had to be on a dose of at least 400 mg a day for 20 of the last 28 days. Regorafenib…can be a tough drug to give in some patients, so that’s why these criteria were selected in terms of patient tolerability. That is important if you’re going to use this in clinical practice, to ensure that it’s restricted to patients who have tolerated sorafenib in the first line.
Regorafenib significantly improved OS, with a median OS of 10.6 months versus 7.8 months [HR, 0.63; 95% CI, 0.50-0.79; P < .0001]. There was also a significant improvement in PFS as well as time to progression. In terms of the AE profile, the thing that I’d point out is that [regorafenib] wasn’t that bad. It was a tolerable medication. In contrast with the experiences in colon cancer, the AE profile in the RESORCE trial was much better than expected.5
The CELESTIAL trial [NCT01908426] was published a couple of years ago in the New England Journal of Medicine.6 This was evaluating cabozantinib [Cabometyx] in the second line [versus placebo]. The interesting thing about this trial is that 70% of patients were evaluated in the second line, but just under onethird of patients had received 2 prior lines of therapy, so there are data for cabozantinib even as a third-line agent. Patients were randomized 2:1 to receive cabozantinib at a dose of 60 mg a day or placebo in the second-line setting, although the median dose was 40 mg because of dose reductions.
Once again, there was a significant improvement in OS. Median OS in the cabozantinib arm was 10.2 months versus 8.0 months with placebo [HR, 0.76; 95% CI, 0.63-0.92; P = .005]. There were significant improvements in PFS response rates [HR, 0.44; 95% CI, 0.36-0.52; P < .001], although the response rates in both arms were low, at less than 5%.
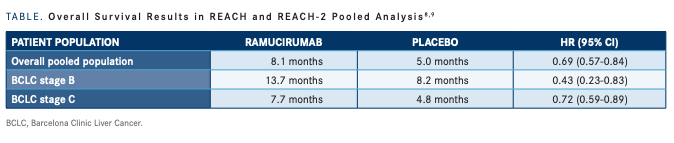
Ramucirumab [Cyramza] was evaluated in the REACH [NCT01140347] and REACH-2 [NCT02435433] trials. The REACH trial was the first evaluation that took all-comers in the secondline setting and randomized them to treatment with ramucirumab versus placebo, with a primary end point of OS. In short, ramucirumab in…all-comers did not improve OS.7 However, in patients who had an elevated AFP [level], greater than 400 IU/mL, there appeared to be a signal.
The [investigators] went back and conducted another phase 3 trial among patients with an elevated baseline AFP [level]. In the second trial, patients were required to have an AFP [level] greater than 400 IU/mL and were randomized to receive ramucirumab or a placebo to once again look at OS with a secondary outcome of PFS.
In the REACH-2 trial, they found an improvement in both OS and PFS.8 They then performed a pooled analysis of both REACH TABLE. Overall Survival Results in REACH and REACH-2 Pooled Analysis 8,9 PATIENT POPULATION RAMUCIRUMAB PLACEBO HR (95% CI) Overall pooled population 8.1 months 5.0 months 0.69 (0.57-0.84) BCLC stage B 13.7 months 8.2 months 0.43 (0.23-0.83) BCLC stage C 7.7 months 4.8 months 0.72 (0.59-0.89) BCLC, Barcelona Clinic Liver Cancer. Case-Based Peer Perspectives Spotlight 19 and REACH-2, taking a look at this subset of patients who had an elevated AFP [level] and reported OS and PFS.9 Both were significantly longer with ramucirumab than placebo [TABLE].8,9
One of the benefits of ramucirumab versus some of the other TKIs [tyrosine kinase inhibitors] in the second-line setting is tolerance. In terms of the AE profile...ramucirumab appears to be better tolerated. The main AE that you see is hypertension.
Can you talk about efficacy of single-agent immunotherapy in this patient population?
SINGAL: Results of the [phase 1/2] CheckMate 040 [NCT01658878] trial showed response rates with nivolumab [Opdivo]. Response rates overall occurred in 15% to 20% of patients and were consistent across etiologies.10 However, this was evaluated in the phase 3 CheckMate 459 trial [NCT02576509], which compared nivolumab versus sorafenib with an overall primary end point of OS. Many of [those in the HCC community] were surprised when the OS failed to show a benefit with nivolumab versus sorafenib. Some of this is related to crossover to second-line agents, but all these excuses aside, the trial is interpreted as a negative study, with no significant difference between the 2 agents.11
Pembrolizumab [Keytruda] was evaluated in the second-line setting in the KEYNOTE-240 study [NCT02702401]. What you saw was that pembrolizumab induced promising response rates, much like nivolumab, with rates that were somewhere between 15% and 20%. Unfortunately, pembrolizumab in the phase 3 study failed to improve survival as a single agent compared with placebo.12
References:
1. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163-1173. doi:10.1016/S0140-6736(18)30207-1
2. Cheng A-L, Qin S, Ikeda M, et al. IMbrave150: Efficacy and safety results from a ph III study evaluating atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (Sor) as first treatment (tx) for patients (pts) with unresectable hepatocellular carcinoma (HCC). Ann Oncol. 2019;30(suppl 9):LBA3. doi:10.1093/annonc/mdz446.002
3. Finn RS, Qin S, Ikeda M, et al. Complete responses (CR) in patients receiving atezolizumab (atezo) + bevacizumab (bev) versus sorafenib (sor) in IMbrave150: a phase III clinical trial for unresectable hepatocellular carcinoma (HCC). J Clin Oncol. 2020;38(suppl 15):4596. doi:10.1200/JCO.2020.38.15_suppl.4596
4. FDA approves Genentech’s Tecentriq in combination with Avastin for people with the most common form of liver cancer. News release. Genentech. May 29, 2020. Accessed June 26, 2020. https://www.gene.com/media/press-releases/14856/2020-05-29/ fda-approves-genentechs-tecentriq-in-com
5. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56-66. doi:10.1016/ S0140-6736(16)32453-9
6. Abou-Alfa GK, Meyer T, Cheng AL, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med. 2018;379(1):54-63. doi:10.1056/ NEJMoa1717002
7. Zhu AX, Park JO, Ryoo BY, et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015;16(7):859-870. doi:10.1016/S1470-2045(15)00050-9
8. Zhu AX, Kang YK, Yen CJ, et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(2):282-296. doi:10.1016/S1470-2045(18)30937-9
9. Kudo M, Finn RS, Morimoto M, et al. Ramucirumab for patients with intermediatestage hepatocellular carcinoma (HCC) and elevated alpha fetoprotein (AFP): pooled results from two phase III studies (REACH and REACH-2). J Clin Oncol. 2020;38(suppl 4):549. doi:10.1200/JCO.2020.38.4_suppl.549
10. El-Khoueiry AB, Sangro B, Yau T, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389(10088):2492-2502. doi:10.1016/ S0140-6736(17)31046-2
11. Bristol-Myers Squibb announces results from CheckMate-459 study evaluating Opdivo (nivolumab) as a first-line treatment for patients with unresectable hepatocellular carcinoma. News release. Bristol-Myers Squibb Co. June 24, 2019. Accessed June 30, 2020. https://news.bms.com/press-release/bmy/ bristol-myers-squibb-announces-results-checkmate-459-study-evaluating-opdivo-nivol
12. Merck provides update on KEYNOTE-240, a phase 3 study of Keytruda (pembrolizumab) in previously treated patients with advanced hepatocellular carcinoma. News release. Merck. February 19, 2019. Accessed June 30, 2020. https://investors. merck.com/news/press-release-details/2019/Merck-Provides-Update-on-KEYNOTE240-a-Phase-3-Study-of-KEYTRUDA-pembrolizumab-in-Previously-Treated-Patientswith-Advanced-Hepatocellular-Carcinoma/default.aspx