Current Immunotherapy: Progress With Adoptive Cellular Therapies and Combinations
The clinical development and application of cancer immunotherapy over the past decade has translated the long-standing knowledge of the close relationship between cancerous tissues and lymphoid immune cells, dating back to the late 19th century.
Patrick Hwu, MD
Patrick Hwu, MD
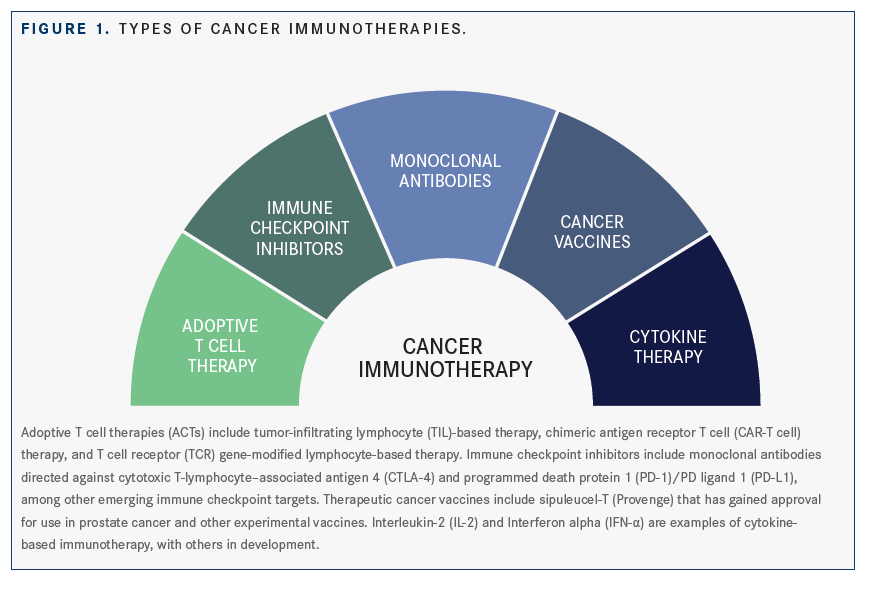
The clinical development and application of cancer immunotherapy over the past decade has translated the long-standing knowledge of the close relationship between cancerous tissues and lymphoid immune cells, dating back to the late 19th century.1,2Today, cancer immunotherapies, all of which recruit the body’s own immune system to target and eliminate cancer cells, represent a rapidly expanding and paradigm-shifting arsenal in cancer treatment. Immunotherapies that have gained regulatory approval and/or are in clinical development include immune checkpoint blockade agents, chimeric antigen receptor (CAR) T-cell therapy, cancer vaccines, and adoptive or engineered T cellbased therapies(FIGURE 1).35
“Living Drugs”: An Overview of Adoptive T-Cell Therapies
In adoptive cell therapy (ACT), the intrinsic antitumor cytotoxic activity of the host immune system, especially antitumor cytotoxic T lymphocytes (CTLs), is harnessed to target and eliminate tumor cells by adoptive transfer of tumor-associated antigen-specific CTLs derived either from the tumor itself (tumor infiltrating lymphocytes [TILs]) or from peripheral blood (patient lymphocytes engineered to target tumor antigens in CAR T- or engineered T-cell receptor [TCR] cellular therapies). A remarkable feature of all types of ACT is the potential for personalization. All current ACT treatments use autologous T cells as the initial resource that is then customized to generate a “living drug” highly specific to the individual patient and their cancer. The fundamentals, current scope, and emerging concepts of ACT in cancer are the focus of a presentation by Patrick Hwu, MD, division head, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center during the Society for Immunotherapy of Cancer’s 34th Annual Meeting (SITC 2019).
TIL Therapy: Modulating the TILTumor Microenvironment Interaction
Steven A. Rosenberg, MD, PhD, and colleagues lay the foundation for TIL therapy nearly 40 years ago when they demonstrated that lymphocytes extracted from freshly resected melanomas, expanded ex vivo, and infused back into the patients could induce high response rates in patients with metastatic melanoma.6Solid tumors are infiltrated by many immune cells, including T and B lymphocytes, natural killer cells, dendritic cells, and macrophages. Among these, TILs are thought to indicate an antitumor immune response and have been identified as favorable prognostic indicators in many cancers including melanoma and breast cancer.7,8TILs also affect treatment response; for instance, the relative abundance of CD8-positive (+) TILs predicted response to antiPD-1 therapy in melanoma and the presence of TILs, along with PD-L1 expression, correlated with pathologic complete response rates to neoadjuvant chemotherapy in breast cancer.9,10
“We started utilizing [TIL therapy] first in melanoma,” said Hwu, who was previously at the National Cancer Institute working with the TIL pioneer Rosenberg on some of the earliest ACT studies, “but we’re now investigating [TIL immunotherapy] in a number of other cancer types, including pancreatic, ovarian, and colon cancers.” Clinical data on TILs in metastatic melanoma have been consistently promising, and TILs have been produced successfully for other cancers.
Clinical data on TILs for metastatic melanoma have consistently been promising, and TILs have been successfully produced for other cancers.5The high mutation-al load and high neoantigen rates are thought to account for the significant and consistent clinical benefit of TIL therapy in patients with metastatic melanoma, whereas the heterogeneity in these key attributes, as well as key differences in the tumor microenvironment (TME), may account for the variability in tumor reactivity of TILs in other solid tumors. Hwu and colleagues are evaluating strategies to enhance the survival and activity of TILs in the context of the tumor microenvironment. In one such innovative approach, they have inserted the gene encoding a dominant-negative form of the transforming growth factor (TGF)-β _receptor into immune cells.
Tumors, tumor-associated stromal cells, and regulatory T cells (Tregs) produce large quantities of TGF-β, which acts as a key immunosuppressant in the TME.11Introduction of the decoy TGF-β _receptor depletes TGF-β _in the TME without invoking TGF-β _immunosuppressive activity, which allows the TILs to mount a robust antitumor immune response. Speaking to the clinical utility of this approach, Hwu said, “[Using this approach], we have obtained clinical responses in metastatic melanoma patients with disease resistant to the standard-of-care [therapy], including the immune checkpoint blockade agents, such as anti-PD-1 antibodies. Even if the patients had progressed after antiPD-1 therapy, this mode of [TIL] therapy has yielded durable responses in some patients thus far.” He added that they use of the TGF-β _decoy receptor may be a feasible approach in other ACTs.
CAR T-Cell Therapies Overcoming Resistance
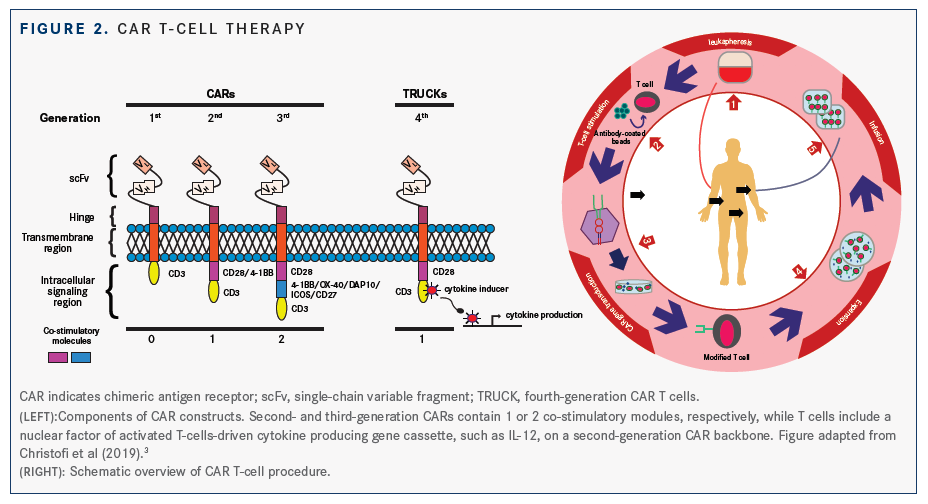
CAR T-cellbased immunotherapy relies on the recognition of antigens expressed on the tumor cell surface by the synthetic CARs transduced into autologous T cells. CARs are synthetic receptors generally constructed by fusing an antigen-specific single-chain antibody fragment with signaling molecules of the TCR/CD3 complex, usually the CD3ζ _chain. Although CD19 is the most studied CAR target, the intracellular domain of the engineered CAR may also contain costimulatory modules that stimulate T cell activation, proliferation, and cytokine production(FIGURE 2).3,12CAR-T cell therapy has yielded promising data in hematologic malignancies, especially B-cell neoplasms.13“As the work on CD19-targeted CAR T-cell therapy has matured, it looks like some patients progress even after an initial response to the CAR T therapy,” Hwu said, alluding to the significant clinical challenge of resistance to CAR T-cell therapy. He pointed to studies that have helped uncover the key mechanisms of development of resistance to CAR T-cell therapy, including loss of tumor antigen (eg, loss of tumor CD19 expression) and loss of T cell “fitness” over time.1417
Engineered TCR-Based Therapies: A Look Ahead
In TCR gene therapy, a novel TCR is introduced into patient-derived T cells by engrafting genes that encode TCR-α _and β _chains to allow the cells to recognize tumor antigens in an MHC-dependent manner.18The potency of TCRs depends on their interaction with peptide- MHC complexes that are tumor-specific or are enriched in the tumor. Tumor-associated antigens can be encoded by mutated genes (neoantigens) or can be derived from proteins that are overexpressed in tumors. TCRs from T cells harboring HLA alleles matching the class in the antigen-presenting cells recognize peptide-major histocompatibility complex (pMHCs)and ultimately promote the killing of cancer cells. While most current TCR therapies use MHC class Irestricted TCRs to genetically modify CD8+ T cells or bulk T cells for patient treatment, recent evidence suggests that TCR-engineered MHC class II-restricted CD4+ T cells may also have utility in cancer immunotherapy. “Many groups are now trying to develop a library of TCR genes to target various tumors, based on what tumor antigens and human leukocyte antigen (HLA) alleles are being expressed in individual patients, to allow for transduction of the HLA-matched TCRs for adoptive T-cell transfer,” Hwu said. “This approach has [already been] demonstrated to be successful in synovial cell sarcoma.” Combo Therapy Tackles Challenges, Adds Clinical Benefits Immune checkpoint inhibitors (ICIs), which target coinhibitory checkpoint receptors CTLA-4 or the PD-1/PD-L1 axis, have demonstrated remarkable clinical activity in many cancers; however, despite their unprecedented success, response to ICIs is neither universal nor uniform. “Less than half of the patients respond to treatment with ICI monotherapy and many cancers lack the baseline immunogenicity and/or immune checkpoint pathway proteins necessary for susceptibility to immunotherapy, resulting in dramatic variations in response rates (5% to ~90%) across tumor types,” said Leisha Emens, MD, PhD, professor of medicine and director of translational immunotherapy at the Women’s Cancer Research Center, UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania. “Finding a way to bring the benefit to more patients and convert nonresponders to responders, finding a way to rescue patients who progress, and extending and deepening the response are all high-priority goals for research. Finding ways to overcome these challenges will allow us to bring the survival benefit of immunotherapy to more patients,” she said. Emens, who will be focusing on combination immunotherapies in her presentation during SITC 2019, noted that these reasons underlie the rationale for exploring combination immunotherapies. In addition, she stated that combinations can help harness tumor biology and integrate immune-targeted therapies with historical treatment modalities, such as radiation and chemotherapy, to provide synergistic benefits to patients.
A Framework to Design Rational Combinations With Immunotherapy Agents
Speaking to the foundational premise of combination immunotherapies, Emens said, “Many improvements can be made with immunotherapy combinations, and the combination modalities should be based on the mechanism of induction of the antitumor immune response.” She elaborated on how this response has been described with the “cancer immunity cycle,” a series of stepwise events that must be initiated, progress, and expand iteratively.19“If you understand which [step or steps are] defective in a given patient’s tumor, then you can design combinations that fill the gap and let the immune cycle be completed. If this design is predicated on underlying mechanisms and is clinically sustained, the combination can perform as a self-perpetuating cycle, where the T-cell response continues until the tumor is eliminated,” Emens said. Current and emerging evidence support further development of combinations of immunotherapies, including ICIs, with other therapies or agents as well as other immunotherapy agents in the same class or different classes. For instance, the addition of pembrolizumab (Keytruda), an antiPD-1 antibody, to standard chemotherapy with pemetrexed and a platinum-based drug resulted in significantly longer overall survival (OS; 12-month OS, 69.2% vs 49.4%; HR for death, 0.49) and progressionfree survival (PFS; 8.8 vs 4 months) than chemotherapy alone in patients with previously untreated metastatic nonsquamous non–small cell lung cancer (NSCLC) without EGFR or ALK mutations.20Similarly, the combination of radiation therapy, which can promote the activation of antitumor T cells, thereby augmenting sensitivity to subsequent immunotherapy, with CTLA-4 blockade with ipilimumab (Yervoy), improved responses in chemotherapy-refractory metastatic NSCLC where antiCTLA-4 antibodies had failed to demonstrate significant efficacy alone or in combination with chemotherapy.21Further, combining 2 different ICIs, nivolumab (Opdivo) and ipilimumab, improved PFS, OS, and overall response rates versus ipilimumab alone in patients with advanced melanoma.22,23Emens outlined data from combination immunotherapy studies that are coupling immunotherapy agents to novel drugs and therapies, predicated on optimizing the anti-tumor immune response based on tumor-, disease-, and mechanism-specific features. Rational, mechanism-based, novel combinations can help overcome resistance, relapse, or progression after immunotherapyas in a recent study of a combination of pembrolizumab and intratumoral SD-101, a synthetic cytosine-phosphate-guanosine (CpG) oligonu that stimulates Toll-like receptor 9 (TLR9) in patients with unresectable or metastatic malignant melanoma. Early data showed that this combination was well tolerated and induced immune activation at the tumor site, without additional toxicity over pembrolizumab alone.24 Other examples of pioneering combinations mentioned by Emens include pembrolizumab with epacadostat in patients with advanced solid tumors25; nivolumab in combination with ALT-803, an interleukin-15 superagonist, in metastatic NSCLC26; and oncolytic virotherapy with talimogene laherparepvec (Imlygic) in combination with pembrolizumab in advanced melanoma.27“My goal is to review the combination of immunotherapies and their importance and provide a framework for how to think about developing innovative combinations,” said Emens of her presentation. Some of the key factors to consider in development of immunotherapy combinations include setting clear parameters to define the clinical activity of a combination immunotherapy relative to the activity of either single agent in the context of the tumor type in which it is being tested; evaluating pharmacodynamic changes with agnostic and high-throughput systems-biology technologies; and accounting for the effect of treatment context, drug dose, and treatment sequencing. Emens notes that while combination immunotherapies may help expand the numbers of patients deriving benefit from immunotherapy, it is also important to consider the potential for unexpected and/or synergistic toxicities with these combinations.
Combinations on the Horizon
The development of immunotherapeutic agents has transformed the treatment landscape of cancer across cancer types and yielded remarkable clinical benefits in responding patients, including those with advanced cancers previously thought to be intractable or difficult to treat. As the field matures, there is great optimism for the range of therapies in use or in development for recruiting the body’s immune system to the anticancer combat.
“I think that immune cell therapy is important and T cell therapy is very exciting. I predict that it is an area that will be growing in importance in coming years for all cancers,” said Hwu. He alluded to ongoing investigations to identify biomarkers predictive of response to TIL therapy as another avenue of growth in immunotherapy.
Emens expressed similar optimism: “I believe that we will be able to make immunotherapy work for almost any tumor. If you understand the immunobiology of that specific tumor, you can design ways of eliminating it that capitalize on the antitumor response.” She added, “The development of combinations should consider the immunobiology of the patient’s tumor, the mechanism of each agent, and how they might interact when given together.
References
- Virchow RLK. Cellular Pathology as Based upon Physiological and Pathological Histology. Philadelphia: J. B. Lippincott; 1863. bit.ly/2P4GenF. Accessed August 27, 2018.
- David H. Rudolf Virchow and modern aspects of tumor pathology.Pathol Res Pract. 1988;183(3):356-364. doi: 10.1016/S0344-0338(88)80138-9.
- Christofi T, Baritaki S, Falzone L, Libra M, Zaravinos A. Current perspectives in cancer immunotherapy. Cancers. 2019;11(10):1472. doi: 10.3390/ cancers11101472.
- Zhang H, Chen J. Current status and future directions of cancer immunotherapy.J Cancer. 2018;9(10):1773-1781. doi: 10.7150/jca.24577.
- Rohaan MW, Wilgenhof S, Haanen JBAG. Adoptive cellular therapies: the current landscape.Virchows Arch Int J Pathol. November 2018. doi: 10.1007/s00428-018-2484-0.
- Rosenberg SA, Packard BS, Aebersold PM, et al. Use of tumor-infiltrating lymphocytes and interleukin-2 in the immunotherapy of patients with metastatic melanoma: a preliminary report.N Engl J Med. 1988;319(25):1676- 1680. doi: 10.1056/NEJM198812223192527.
- Geukes Foppen MH, Donia M, Svane IM, Haanen JBAG. Tumor-infiltrating lymphocytes for the treatment of metastatic cancer.Mol Oncol. 2015;9(10):1918-1935. doi: 10.1016/j.molonc.2015.10.018
- Denkert C, von Minckwitz G, Darb-Esfahani S, et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018;19(1):40-50. doi: 10.1016/S1470-2045(17)30904-X.
- Daud AI, Loo K, Pauli ML, et al. Tumor immune profiling predicts response to anti-PD-1 therapy in human melanoma.J Clin Invest. 2016;126(9):3447-3452. doi: 10.1172/JCI87324.
- Wimberly H, Brown JR, Schalper K, et al. PD-L1 expression correlates with tumor-infiltrating lymphocytes and response to neoadjuvant che-motherapy in breast cancer.Cancer Immunol Res. 2015;3(4):326-332. doi: 10.1158/2326-6066.CIR-14-0133.
- Dahmani A, Delisle J-S. TGF-β in T cell biology: implications for cancer immunotherapy.Cancers. 2018;10(6):194. doi: 10.3390/cancers10060194.
- Tariq SM, Haider SA, Hasan M, et al. Chimeric antigen receptor T-cell therapy: a beacon of hope in the fight against cancer.Cureus. 2018;10(10):e3486. doi: 10.7759/cureus.3486.
- Ott PA, Dotti G, Yee C, Goff SL. An update on adoptive T cell therapy and neoantigen vaccines.Am Soc Clin Oncol Educ Book. 2019;(39):e70-e78. doi: 10.1200/EDBK_238001.
- Majzner RG, Mackall CL. Tumor antigen escape from CAR T cell ther-apy.Cancer Discov. 2018;8(10):1219-1226. doi: 10.1158/2159-8290. CD-18-0442.
- Boyiadzis MM, Dhodapkar MV, Brentjens RJ, et al. Chimeric antigen receptor (CAR) T therapies for the treatment of hematologic malignancies: clinical perspective and significance.J Immunother Cancer. 2018;6(1):137. doi: 10.1186/s40425-018-0460-5.
- Fraietta JA, Lacey SF, Orlando EJ, et al. Determinants of response and resistance to CD19 chimeric antigen receptor (CAR) T cell therapy of chronic lymphocytic leukemia.Nat Med. 2018;24(5):563-571. doi: 10.1038/s41591-018-0010-1.
- Target antigen downregulation and other mechanisms of failure after axicabtagene ciloleucel (CAR19) therapy.Blood. 2018;132(suppl 1;abstr 732). doi: 10.1182/blood-2018-99-120206.
- Ping Y, Liu C, Zhang Y. T cell receptor-engineered T cells for cancer treatment: current status and future directions.Protein Cell. 2018;9(3):254- 266. doi: 10.1007/s13238-016-0367-1.
- Chen DS, Mellman I. Oncology meets immunology: the cancer immunity cycle.Immunity. 2013;39(1):1-10. doi: 10.1016/j.immuni.2013.07.012.
- Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic nonsmall cell lung cancer.N Engl J Med. 2018;378(22):2078-2092. doi: 10.1056/NEJMoa1801005.
- Formenti SC, Rudqvist N-P, Golden E, et al. Radiotherapy induces responses of lung cancer to CTLA-4 blockade.Nat Med. 2018;24(12):1845- 1851. doi: 10.1038/s41591-018-0232-2.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma.N Engl J Med. 2015;373(1):23- 34. doi: 10.1056/NEJMoa1504030.
- Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma.N Engl J Med. 2017;377(14):1345-1356. doi: 10.1056/NEJMoa1709684.
- Ribas A, Medina T, Kummar S, et al. SD-101 in combination with pembrolizumab in advanced melanoma: results of a phase Ib, multicenter study.Cancer Discov. 2018;8(10):1250-1257. doi: 10.1158/2159-8290.CD-18-0280.
- Mitchell TC, Hamid O, Smith DC, et al. Epacadostat plus pembrolizum-ab in patients with advanced solid tumors: phase I results from a multi-center, open-label phase I/II trial (ECHO-202/KEYNOTE-037).J Clin Oncol.September 2018:JCO2018789602. doi: 10.1200/JCO.2018.78.9602.
- Wrangle JM, Velcheti V, Patel MR, et al. ALT-803, an IL-15 superagonist, in combination with nivolumab in patients with metastatic non-small cell lung cancer: a non-randomised, open-label, phase 1b trial.Lancet Oncol. 2018;19(5):694-704. doi: 10.1016/S1470-2045(18)30148-7.
- Ribas A, Dummer R, Puzanov I, et al. Oncolytic virotherapy promotes intratumoral T cell infiltration and improves anti-PD-1 immunotherapy.Cell.2017;170(6):1109-1119.e10. doi: 10.1016/j.cell.2017.08.027.