Pennell Examines Targeted Therapies in EGFR-Mutated NSCLC
Nathan A. Pennell, MD, PhD, discussed the case of 66-year-old patient with EGFR-mutant non–small cell lung cancer, during a virtual Case Based Peer Perspectives event.

Nathan A. Pennell, MD, PhD, associate professor, director, Lung Medical Oncology Program, Taussig Cancer Institute, Cleveland Clinic, in Cleveland, Ohio, discussed the case of 66-year-old patient with EGFR-mutant non–small cell lung cancer (NSCLC), during a virtual Case Based Peer Perspectives event.
Targeted Oncology™: Would you initiate immunotherapy at this point or wait for molecular panel test results?
PENNELL: Regarding recommendations about up-front molecular panel testing, we know that patients with nonsquamous, non– small cell lung cancer need to be routinely tested for genomic alterations because we have effective treatments for those. The College of American Pathology [CAP], International Association for the Study of Lung Cancer, and Association for Molecular Pathologists have come together with guidelines recommending that every patient be tested up front for EGFR, ALK gene fusions, and ROS1. BRAF was not included in the most recent guidelines because the panel closed their deliberations before the approval of dabrafenib [Tafinlar] and trametinib [Mekinist] in lung cancer, but the American Society of Clinical Oncology’s guidelines then added those agents as a standard recommendation. The National Comprehensive Cancer Network [NCCN] endorses that as well.1
NTRK is not included in the major guidelines, but it is a recommendation, especially through NCCN, mostly because there is highly effective treatment if you find it. A major downside of NTRK is that it is so rare, probably something in the range of 0.1% to 0.3%, or 1 of every 300 to 1000 patients with lung cancer. I personally have not yet seen a patient with NTRK.
I think we’ll have agents approved in the RET fusion space, in the MET exon 14, and then possibly in EGFR exon 20 insertion mutations, all in the next year or so. It’s becoming clear that you need to do multiplex testing, and you can’t just do a single polymerase chain reaction test or an immunohistochemistry test or a fluorescence in situ hybridization [FISH] test. You’re going to exhaust your tissue, and it’s going to end up costing way too much and taking way too long. You need to do a single multiplex test such as next-generation sequencing [NGS] routinely for these patients, and that is the recommendation from NCCN and the CAP guidelines.
The truth is that Cleveland Clinic still uses hotspot testing— using a limited NGS panel with companion FISH, although we’re hoping to move to a more comprehensive NGS panel sometime soon. I think as we identify more mutations that require checking, that [change] becomes more pressing. Also, PD-L1 is to help guide patients eligible for frontline single-agent PD-1 therapy versus chemotherapy plus PD-1.
Do you perform molecular testing on patients with squamous cell lung cancer?
The guidelines still haven’t come around to that. I am aware of studies showing that [genomic aberrations] can be found in squamous cells. I’ve done [some] digging, and some [evidence] suggests that [those aberrations] aren’t as common in squamous cell as some studies have said, and that it may be quite rare. So, as of right now, we’re not routinely testing patients with squamous cell lung cancer, although for any refractory patient after standard treatment, it’s not unreasonable to do prompt genomic testing. A subset of patients with squamous cell will have mixed adenosquamous [lung cancer], and those patients can have drivers.
What are some reasons for obtaining liquid biopsies for these patients?
In my use of liquid biopsies, it’s less about not having enough tissue and more about timing. In the case of tissue biopsy, sometimes the hospital where the patient had the biopsy done is the challenge because we don’t know where the tissue has been sent, or it’s been sent somewhere and we don’t know how to obtain the tissue. [We may not know] who ordered it and when it’s coming back, or the patient needs treatment but weeks are going by and we don’t have those results. Liquid biopsy has been useful in at least getting some up-front results, though. In some hospitals, you can order liquid biopsies at the same time as tissue biopsies, and that can improve the whole process.
Are there drawbacks of relying on liquid biopsies for diagnostic purposes?
I think the primary concern with liquid biopsies is that as stand-alone tests, they may not be as sensitive as tissue tests. Of course, tissue tests themselves are not perfect; they’re subject to sampling and preparation and fixation and the quality of the DNA and RNA that comes out of them.
Most of the time, when you see discordance between liquid and solid [biopsies], it’s something technical that caused that test to fail. But, more likely, you’ll see a positive result in tissue that failed in liquid. It seems to be related to tumor burden. Patients who have bone metastases or liver metastases are positive on a liquid biopsy, whereas people who have lung-only disease are relatively limited—with malignant infusions, etcetera—which may result in negative liquid biopsies, at least in my experience.
The general recommendation is that although liquid biopsies can be useful, they shouldn’t replace tissue biopsies. If you get a negative result on a liquid biopsy, you should follow it up with a tissue test.
I prefer to order a liquid biopsy because it’s so fast. Lack of insurance coverage is probably the main barrier to not having the liquid biopsy for everyone. The evidence suggests that you get more positive test results by doing both tests.
Regarding a lack of tissue harvesting: I think that having reliable communication and understanding from your interventionalists—the [doctors] who are getting your biopsies, whether it’s [via] interventional radiology [IR] or bronchoscopy—is invaluable, because when they’re in there getting that fine needle aspiration [FNA], they don’t have to just do a single pass. Even if they can get only an FNA, they can usually get multiple passes. If the interventional radiologist is working closely with the pathologist, you can often get enough tissue provided from 1 lesion. But it depends a lot on how it’s done and whether the IR [person] is aware ahead of time that they need [to get enough] tissue.
What are the treatment options for this patient considering his molecular testing results?
The patient does not have a lot of symptoms but does have a brain metastasis. The patient also has an EGFR exon 19 deletion and high PD-L1. I’m leaning toward an EGFR tyrosine kinase inhibitor [TKI] as frontline treatment.
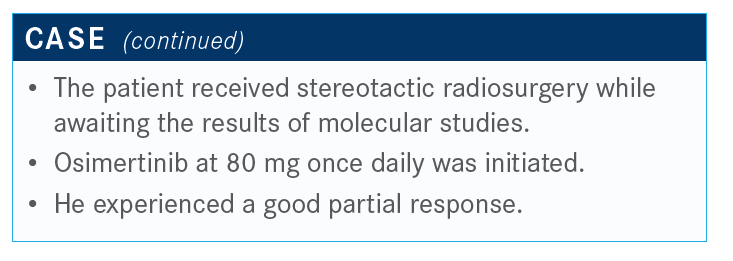
The brain metastasis might be a decision factor. Some agents that we use now, such as osimertinib [Tagrisso], have some pretty good activity in the central nervous system [CNS]. We could consider referring this patient for stereotactic radiation and/or surgery versus no surgery, given that I think there’s a lesion in the vision center. It’s a decision on stereotactic radiation versus treating with primary systemic therapy. This might be a case in which we don’t know the right answer. At Cleveland Clinic, an osimertinib plus gamma knife trial is going on [NCT03535363], although it’s not a randomized trial.
We do know that the CNS response rate is similar to the systemic response rate with osimertinib. But at the same time— as has been pointed out to me by my colleagues in radiation oncology—during the period between scans, if patients’ lesions were to grow significantly, their risk of complications from gamma knife grows significantly. It’s much less morbid to treat them when they’re small.
So in the case of a patient whose testing results [didn’t com back for] a week or 2, especially when you don’t know at that time that they had an EGFR mutation like this patient, he probably would be referred for gamma knife radiation while waiting for test results.
Are there options besides osimertinib available for these patients?
Options other than osimertinib would include a first-generation or second-generation TKI: erlotinib [Tarceva], afatinib [Gilotrif], or dacomitinib [Vizimpro].
If the patient is progressing and we see [they are] T790M positive, you could switch to osimertinib, which might, potentially, lengthen the patient’s disease control. Perhaps [you could] use chemoimmunotherapy, based on the IMpower150 [NCT02366143] trial results. However, patients in IMpower150 had already progressed from an EGFR TKI treatment prior to the trial, so it didn’t include first-line patients. Now we also have some positive trials with erlotinib with ramucirumab [Cyramza] that yielded an impressive progression-free survival [PFS] of about 19 months [NCT02411448].2
What do the NCCN guidelines say for this setting?
Generally, they suggest that the use of PD-1 or PD-L1 inhibitors is contraindicated in the presence of an oncogene, which would predict lack of benefit.1
What data do we have that demonstrate the benefit of avoiding the use of an immune checkpoint inhibitor (ICI) in a patient with an EGFR mutation?
The trial conducted by Aaron Lisberg, MD, and colleagues is among the most meaningful, although it’s small, in [showing] why you should not give an ICI to a patient with EGFR mutations.3
This was a phase 2 trial, and all patients were EGFR mutation positive, PD-L1 positive, and previously untreated. A total of 75% of the enrolled patients had high PD-L1 expression, and they were treated with a TKI with pembrolizumab in the first-line setting.
The investigators intended to enroll 25 patients, but they had to halt accrual after 11 patients because they did not see a single response in any of the patients with a confirmed EGFR mutation. There was 1 response, but that patient was later confirmed to not have an EGFR mutation. So 10 of 10 patients did not respond, even though three-quarters of them were PD-L1 positive. And, importantly, most of these patients switched over to a TKI. Most patients received a TKI even after going off pembrolizumab, but a couple of them died and one of them had a grade 5 pneumonitis risk event after being treated with osimertinib.
The take-home message is that patients with an EGFR mutation tend to not respond even in the presence of a high PD-L1. If you think about it, PD-L1 positivity is a secondary reaction. There is an immune response that is essentially inducing local cytokines. PD-L1 is reacting to an inflammatory response in a patient who is likely to benefit from ICIs.
Data have shown that patients with an EGFR mutation and other driver oncogenes have constitutive high expression of PD-L1, because everything is essentially turned on in patients who have driver oncogenes. It is not a reaction to an immune response, and therefore you simply can’t trust PD-L1 expression as a meaningful biomarker in driver oncogene patients.
Additionally, if you give someone pembrolizumab, which has a half-life of weeks to months, that patient is going to have it in their system for a long time when you might want to be giving them a TKI.
What are the safety considerations associated with ICIs and EGFR-TKI sequencing?
A number of toxicity concerns exist. There have been a number of phase 1 trials as well as retrospective experiences of patients with EGFR mutations who received PD-L1 or PD-1 inhibitors and then went on to osimertinib. Adam J. Schoenfeld, MD, and colleagues demonstrated a 15% risk of severe immune related adverse effects [irAEs].4 This was observed in all-comers. Patients who received treatment within 3 months of a checkpoint inhibitor had a much higher rate [of irAEs]. That is my general rule of thumb: to wait at least 3 months after giving an ICI before using osimertinib if possible.
This safety profile is not unique to EGFR inhibitors. It has been observed in patients who are ALK positive, as well. Usually, we see more hepatotoxicity in combinations with drugs like alectinib [Alecensa], ceritinib [Zykadia], and pegaptanib [Macugen]. It’s probably risky to combine a checkpoint inhibitor with a TKI. This is one of the biggest reasons it’s critically important to get that molecular testing done before you start the patient on immune therapy.
Chee Khoon Lee, PhD, and colleagues conducted a meta-analysis of multiple phase 3, second-line trials with atezolizumab [Tecentriq], nivolumab [Opdivo], and pembrolizumab [Keytruda].5 These studies, in general, showed that patients with the EGFR mutation received no hint of a survival benefit. In fact, there may have been a hint of harm in patients treated with ICIs compared with chemotherapy.
Lee further demonstrated that there was no significant difference [between the chemotherapy and ICI arms], but there was a trend to favor the chemotherapy arm in patients with EGFR mutations.
That’s not to say this combination can never work; some evidence shows that patients who were previously treated with TKIs and who are treated with chemotherapy plus a checkpoint inhibitor may benefit. That comes from the IMpower150 study, which was platinum and either paclitaxel or nab-paclitaxel [Abraxane], bevacizumab [Avastin], and atezolizumab.6 About 20% of the patients on the trial had an EGFR mutation or an ALK gene fusion, although most of them were patients who were EGFR positive. There seemed to be a similar magnitude of PFS and overall survival [OS] benefit seen in the [population with mutations] compared with the overall population. It wasn’t statistically significant, and it was a small subset, but the hazard ratio is essentially the same. And just recently I saw that, with updated [results], it is still holding true that the patients with mutations seemed to be doing better on that trial.
If you’re going to use an ICI in a patient with an EGFR mutation, after TKIs have been exhausted, if you’re going to switch them to chemotherapy, that would be a time to consider [doing so].
What evidence do we have about using osimertinib in the first-line setting?
The FLAURA study [NCT02296125] evaluated patients with EGFR mutations.7 It evaluated osimertinib versus either erlotinib [Tarceva] or gefitinib [Iressa], and the primary end point was PFS.
The investigators allowed patients with untreated CNS metastases to participate. The PFS of the osimertinib arm was 19 months compared with 10 months, which is exactly what you would expect with a first-generation inhibitor.
The important end point in this study was OS, and the OS was statistically significantly improved compared with first-generation inhibitors, with about a 7-month difference between median OS. One of the most remarkable things about this is that the median survival of these patients is 38.6 months. That’s in excess of 3 years, median, for our patients with newly diagnosed metastatic lung cancer, which is absolutely extraordinary if I think back to what it was like at the beginning of my career when the stage IV patients’ median OS was [about] 10 months.
Some oncologists have considered waiting and treating with a first-generation inhibitor. Would patients do just as well? Importantly, although I don’t think this gets emphasized enough, the FLAURA trial did that. The investigators followed patients who progressed and crossed over to osimertinib from the control arm. In fact, 47% of people in the standard-of-care, first-generation TKI arm crossed over to osimertinib. This is exactly what you would anticipate the T790M population being, which is about half of people. Despite the number of patients crossing over, there was still an OS benefit in support of osimertinib.
I think [FLAURA] was a sequencing trial, and it failed to be better with sequencing and osimertinib. I think this just confirms that this should be the best available treatment until, of course, there’s one that is better.
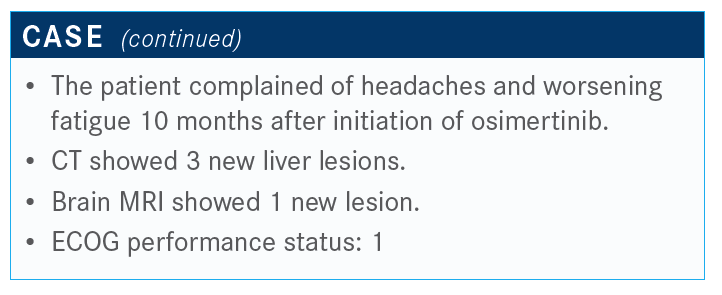
Would you consider ordering a new biopsy in a patient on osimertinib at the time of progression? Would it be tissue or liquid?
You would want to rule out a progression to small cell lung cancer, which we know happens in somewhere around 10% of people who progress on EGFR inhibitors. I think, in that case, liquid biopsy won’t give you the answer; you have to do a tissue biopsy. I think this is a good reason to consider a biopsy at progression.
The progression to small cell lung cancer is not subtle. Patients usually have rapid progression that’s way out of proportion to what you might expect. EGFR mutations like C797S, which is a new gatekeeper mutation, are relatively rare. It’s not anywhere close to the 50% we saw with T790M. MET amplification is somewhere in the 15% to 20% range, so there is no real dominant mechanism of resistance.
In a patient who is chemotherapy naïve, I would reserve further testing for either exhausting standard options or for enrolling in a clinical trial. I think the tissue biopsy, to rule out small cell, makes perfect sense.
In terms of other options, [consider that] this patient has lots of liver metastases and brain metastases. If it was just a brain metastasis, local therapy, such as gamma knife radiation, might make sense and then [treatment would] continue on. Some studies show that patients can continue on treatment for a longer period if they get local therapy. In local progression or focal progression, I think we would probably not want to add an ICI to treat this patient.
References:
- NCCN. Clinical Practice Guidelines in Oncology. Non-small cell lung cancer, version 6.2020. Accessed June 26, 2020. nccn.org/professionals/physician_gls/pdf/nscl.pdf.
- Nakagawa K, Garon EB, Seto T, et al; RELAY Study Investigators. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(12):1655-1669. doi:10.1016/S1470-2045(19)30634-5
- Lisberg A, Cummings A, Goldman JW, et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1+, tyrosine kinase inhibitor naïve patients with advanced NSCLC. J Thorac Oncol. 2018;13(8):1138-1145. doi:10.1016/j.jtho.2018.03.035
- Schoenfeld AJ, Arbour KC, Rizvi H, et al. Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann Oncol. 2019;30(5):839-844. doi:10.1093/annonc/mdz077
- Lee CK, Man J, Lord S, et al. Clinical and molecular characteristics associated with survival among patients treated with checkpoint inhibitors for advanced non-small cell lung carcinoma: a systematic review and meta-analysis. JAMA Oncol. 2018;4(2):210- 216. doi:10.1001/jamaoncol.2017.4427
- Reck M, Mok TSK, Nishio M, et al. Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir Med. 2019;7(5):387-401. doi:10.1016/S2213-2600(19)30084-0
- Soria J-C, Ohe Y, Vansteenkiste J, et al; FLAURA Investigators. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113-125. doi:10.1056/NEJMoa1713137

Amivantamab/Lazertinib Shows OS and PFS Benefits in EGFR-Mutated NSCLC
April 21st 2025During a live event, Xiuning Le, MD, PhD, discussed updated intracranial efficacy, overall survival, and safety of amivantamab plus lazertinib in patients with EGFR-mutated non–small cell lung cancer.
Read More
Kim Evaluates New Regimens for EGFR+ Lung Cancer
January 20th 2025During a Community Case Forum event in partnership with the Medical Oncology Association of Southern California, Edward S. Kim, MD, MBA, discussed the FLAURA2 and MARIPOSA trials of newer regimens for EGFR-positive lung cancer.
Read More