Roundtable Discussion: Dorff Reviews Factors for Selecting Chemotherapy and Other Later-Line mCRPC Treatments
During a Targeted Oncology™ Case-Based Roundtable™ event, Tanya B. Dorff, and participants, discussed the case of a patient with metastatic castration-resistant prostate cancer who has already received enzalutamide and docetaxel.
Tanya B. Dorff, MD (Moderator)
Associate Professor
Department of Medical Oncology and Therapeutics Research
Section Chief, Genitourinary Disease Program
City of Hope
Duarte, CA

CASE SUMMARY
A 75-year-old man presented with intermittent right hip pain. His physical examination was unremarkable except for a prostate nodule on the rectal exam. He was given an ECOG performance score of 1. His prostate-specific antigen (PSA) level was 16.2 ng/mL, and his transrectal ultrasound scan biopsy showed Gleason grade group 5 (5 + 4). He had a negative bone and abdominal/pelvic CT scan and was diagnosed with stage cT2N0M0 disease. External beam radiation therapy and androgen deprivation therapy were initiated and planned for 24 months. Six months after initiation of therapy, his PSA level was undetectable, so he was considered asymptomatic. He did not return for PSA follow-up.
Thirty-six months later, the patient scheduled an office visit and reported increasing hip pain and urinary frequency. His PSA level was now 29.4 ng/mL, and he had a testosterone level of 300 ng/dL. His bone scan showed evidence of 2 new lesions in the right hip, and an abdominal/pelvic CT scan showed a 2.1-cm left pelvic lymphadenopathy and blastic lesions corresponding to the uptake on the bone scan. Germline and somatic testing were negative for pathogenic alterations.
The patient started treatment with enzalutamide (Xtandi) 160 mg orally every day. His PSA level decreased to a nadir of 3.9 ng/mL 4 months after starting enzalutamide, and his bone pain was resolved. After 8 months on enzalutamide, his PSA level was 12.6 ng/mL, but he was unavailable for intense PSA follow-up. Four months later, he returned with a PSA level of 48.1 ng/mL. Abdominal/ pelvic CT scan showed enlargement of known pelvic lymph nodes. The bone scan showed progressive disease with new lesions, and he reported new back pain and progressive fatigue. His ECOG performance status was 1. He was now considered to have metastatic castration-resistant prostate cancer (mCRPC).
The patient then started on 75 mg/m2 of docetaxel (Taxotere) given every 3 weeks plus 10 mg daily of prednisone. The patient clinically responded, with resolution of pain, improved energy, and a declining PSA. However, with 4 cycles completed, the patient developed worsening bilateral digital neuropathy, so therapy was stopped before cycle 5. Three months later, he had a rising PSA, new back pain, and shortness of breath on exertion. An abdominal/pelvic CT scan now shows enlargement of known pelvic lymph nodes and 1 new liver lesion (< 2 cm).
DORFF: How do you normally manage docetaxel adverse events [AEs]? This patient was stopped after 4 cycles because of some neuropathy. What’s a typical number of cycles that you can get through with your patients? What do you use to decide when and what’s enough?
DEKKER: I continue until the [PSA] nadir or the patient develops dose-limiting toxicities. I probably would have done slightly differently when this patient was at the nadir. I probably would have started him on a secondary maintenance process, but I was not there. I would choose to do a lutetium Lu 177 vipivotide tetraxetan [Pluvicto] evaluation.
He clearly did not have an optimal response to hormonal therapy, but he had response to chemotherapy. He’s [approximately] 80 years old. I always can give him cabazitaxel [Jevtana], and after that, what else [do I have left]? I’ll use a different mechanism of action. There [may be] a long waiting list for lutetium Lu 177 vipivotide tetraxetan. A patient [I see] started cabazitaxel yesterday.
DORFF: Does anyone want to comment on how many cycles of docetaxel they typically utilize?
PHAM: I do the same. I try to get to at least 6 cycles, but until maximum response. I was wondering about an abstract at ASCO [2022 American Society of Clinical Oncology Annual Meeting] that showed continuation of enzalutamide [after progression] with docetaxel [improving] PFS [progression-free survival].1 Is that something that’s going to be more widely used? I usually just would stop it like they did in this case, but that’s another question I had.
DORFF: Yes, that’s an interesting point. I usually stop [enzalutamide treatment].
PHAM: I think if [disease is] stable and they’re doing well, then I’d continue [with docetaxel]. I think the maximum I’ve gotten to do is 10 or 11 cycles. Usually at that point there’s some toxicity.
DORFF: I agree.
FARJAMI: I used to go very liberal. If the patient is responding, one can go up to 10 cycles. It depends on the patient’s profile. But I have to say that in the last few months, finally I was able to get my patient on lutetium Lu 177 vipivotide tetraxetan.
Now we’re facing these patients who have been chronically beaten up previously with radiation, with damaged bone marrow, and extensive chemotherapy, so they cannot actually qualify for lutetium Lu 177 vipivotide tetraxetan. We have problems with patients who have refractory anemia, and they end up doing some bone marrow biopsies. Sometimes it’s bone marrow metastases, and sometimes it’s chronic bone marrow suppression. So that’s another challenge that makes me think twice regarding the duration and AEs of chemotherapy in these patients when we are looking for the next line of treatment.
DORFF: That is a great point. Marrow reserve is a huge issue as we get into later lines of therapy.
MURAD: I usually use 6 cycles. I know that sometimes the PSA can take a while to come down, but I usually stop at 6 cycles.
DORFF: Thanks for raising that. It can be frustrating for patients when they come back for cycle 2 or 3 and their PSA is not going down yet, but you really can see those later drops after cycle 3 or even 4. I do imaging if I get to cycle 3 or 4 with no clear PSA drop just to try to understand what’s going on. So there is a minimum that you’ve got to try to get through, barring a [bad] reaction.
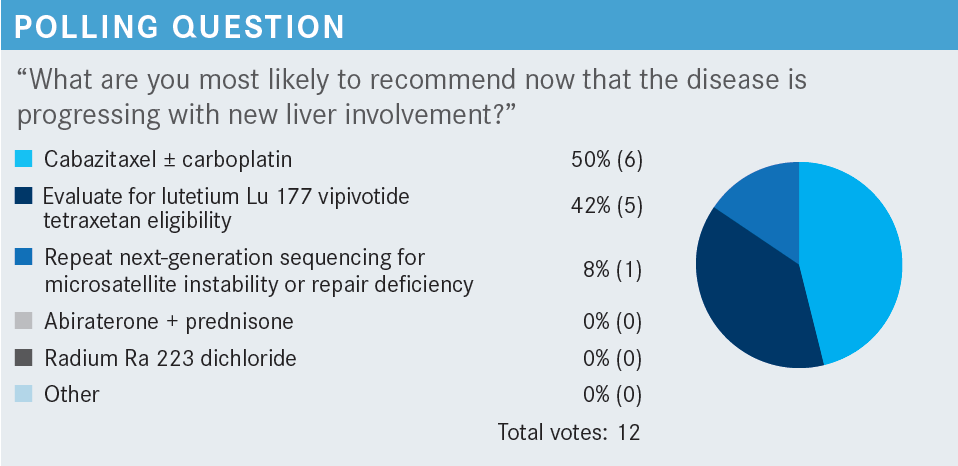
This wasn’t an option in the poll, but would you have wanted to biopsy the liver lesion the patient has?
DEKKER: I probably wouldn’t because he had a very high Gleason score from the beginning. If he came with Gleason score 6, I would be more suspicious of small cell transformation. Gleason score 9 behaves as a typical adenocarcinoma.
DORFF: Very interesting. I think if we didn’t use NGS [next-generation sequencing] at the beginning, that would be a strong reason to biopsy, in addition to looking for [a] neuroendocrine [tumor]. But I agree. To some extent, just having the high Gleason score and the liver metastasis could mean an aggressive variant by clinical features. That’s why cabazitaxel plus carboplatin was an option on the list of next-line treatment.
DEKKER: Dr Dorff, how often do you see negative PSMA [prostate-specific membrane antigen] scans?
DORFF: That’s a good question. I have seen patients with not a fully negative PSMA PET scan. But I recently had a patient with 3 liver metastases, and 2 were negative and 1 had a little bit of PSMA uptake. For him, I’m thinking that lutetium Lu 177 vipivotide tetraxetan is probably not going to be so effective. There’s not so much experience in visceral metastases, and it may not be as effective. It’s something that we need to learn a bit more about.
You must do the scan because the label requires it, but someone can have low-level expression. Even if you want to use all your agents, you want to pick one with a better chance first in case you don’t get to that next line of therapy.
FARJAMI: But if it’s negative, is that a stronger reason to do the biopsy? Just making sure this is not another primary.
DORFF: That is a good point. It could be not only another primary, but neuroendocrine differentiation, which classically doesn’t express PSMA. Himisha Beltran, MD, [of Dana-Farber Cancer Institute] has done some work showing that some neuroendocrine prostate cancers still do express PSMA.2
I do think if you have some negative liver metastases out of the blue on the PSMA PET scan and everything is lighting up, then definitely biopsy. Patients can get a second cancer too. I don’t know about you, but I see so much prostate cancer with almost everything. I’ve had a few patients who developed colon cancer while they had prostate cancer.
DISCUSSION QUESTIONS
- How do you select next line of therapy for a patient with mCRPC who has received docetaxel and an androgen receptor (AR)–targeted therapy?
- What factors do you consider when deciding on treatment?
DEKKER: To me, it would be more of the nature and pace of progression. If somebody is progressing rapidly, it’s one discussion. We have maybe one more shot. If somebody is having slow semi-indolent progression, one may think of how to optimize, or sequence, or what to prioritize now vs later.
DORFF: Yes, that makes a lot of sense. What other factors do you weigh strongly?
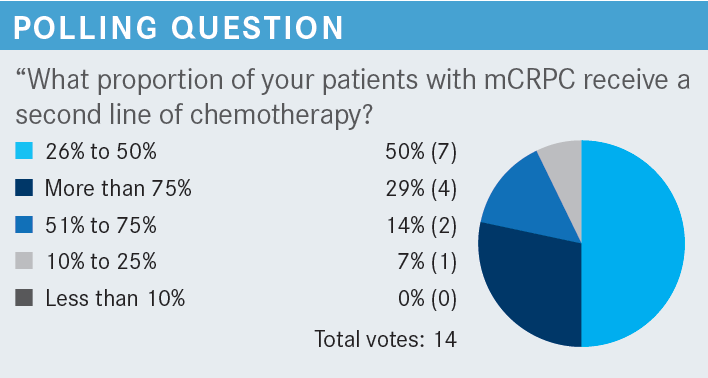
YEH: Performance status is always important if you’re thinking about second-line chemotherapy. If they have a poor performance status, then chemotherapy is pretty much out, which eliminates one choice right there.
DORFF: Yes, I think performance status is huge. Also, social support. I’m more nervous giving a second-line chemotherapy because the patient’s obviously a little bit more heavily pretreated, maybe a little bit frailer if they don’t have good social support. How about age? Does age factor into people’s decisions?
YEH: I think as I get [more experience], age is only a number.
TANG: I agree with that. Age is just a number from my standpoint. It really depends. You have a 60-year-old with diabetes, hypertension, obesity, and you have an 80-year-old who can do marathons. I don’t think age matters more than the performance status.
KRIJANOVSKI: The location of the metastasis [is a factor] because if you have only bone metastases, radium Ra 223 dichloride [Xofigo] could be employed instead of chemotherapy, assuming no further therapy is indicated or desired for other reasons like neuropathy.
DORFF: Yes, I think it’s important to remember that radium Ra 223 dichloride is an option. In the VISION trial [NCT03511664], patients had received prior radium Ra 223 dichloride. That wasn’t an exclusion. So for someone with bone-predominant metastases, that might be the right choice at that moment.
Do you struggle to refer patients for radium Ra 223 dichloride and comanage them with the nuclear medicine or radiation oncology department?
KRIJANOVSKI: It does take a little bit of time to get things situated. It’s not [as immediate] as [you’d] like. I frequently continue second-generation AR therapy and maybe even continue through the treatment. I know it’s not a standard of care, but it helps with disease control. But I have [treated] maybe 3 or 4 [of these patients], so not that many, and these patients had significant neuropathy and diabetes; they couldn’t tolerate any chemotherapy. And that worked well for the duration of response.
DORFF: So for you, it was the right thing for the patients that you were willing to go through the logistics. Because I think that’s going to be an issue with lutetium Lu 177 vipivotide tetraxetan too.
KRIJANOVSKI: Correct. I think at some point they were trying to see [whether] that treatment should be employed sooner as therapy. But it is difficult to [use] with anemia, and [there is a] little bit of dissatisfaction with how quickly a response might come. So a little bit of patience is necessary. Again, the patient had family support and was otherwise stable, not significantly symptomatic, and the pain was under control, so I was able to finish the entire course and had some response for some time. But it’s only in carefully chosen patients.
DORFF: How often are financial considerations an issue? Do some patients refuse certain treatments in your practice?
KRIJANOVSKI: Yes. The financial issue with second-generation AR therapy specifically is a challenge because it’s outpatient treatment. Intravenous therapy is not as difficult to deliver in terms of insurance. For second generation, you want to try apalutamide [Erleada] and other options, but you end up potentially providing generics for enzalutamide and abiraterone acetate [Zytiga].
FARJAMI: We have a little bit of a challenge with lutetium Lu 177 vipivotide tetraxetan in the community. Some of the payers are not completely familiar with it, so there are some delays in the approval to get this treatment for our patients.
DORFF: Have you seen patients end up with a share of cost, like an out-of-pocket cost, with lutetium Lu 177 vipivotide tetraxetan?
FARJAMI: Again, it’s not very clear. I think because it’s relatively new, and some of these IPAs [independent physician associations] or HMOs [health maintenance organizations] don’t have clear coding for that. I [think] they prioritize the less expensive options.
DORFF: Yes, I think it’ll be interesting to see. We don’t have those data yet from our own small group that we’ve treated, but I think for some patients on radium Ra 223 dichloride, there were co-pays, which we don’t think about for infusion therapy like chemotherapy.
DISCUSSION QUESTION
- If a patient didn’t tolerate docetaxel, does that make you worry about giving cabazitaxel?
KRIJANOVSKI: I think cabazitaxel is better tolerated than docetaxel. I’ve had a couple of patients [for] whom we skipped docetaxel and went to cabazitaxel with an adjusted dose, and they did quite well. And we followed with a platinum agent.
FARJAMI: I have to say one of the challenges is the age of our patients. We see a lot of octogenarians and even nonagenarians with the diagnosis of prostate cancer who are still seeking some form of treatment. Beyond the hormonal therapy, we try not to look at the age of the patient, but still, we must respect their physiology. [For a] patient in their late 80s, considering chemotherapy is always a challenge.
Another problem is the label indication of lutetium Lu 177 vipivotide [tetraxetan]. I think there are many patients whom we would desperately like to treat with less toxic treatments, but unfortunately, the current label is inhibitory.
DORFF: Agreed.
CASE UPDATE
A decision was made to start cabazitaxel.
DISCUSSION QUESTION
- What dose of cabazitaxel are you most likely to use for a patient like this: 25 mg/m2, 20 mg/m2, or something else?
FARJAMI: It depends on their bone marrow reserve and how they tolerated docetaxel. How much neutropenia? Will they be supported with growth factors? Those have an impact, but becuase we are getting older and older patients, sometimes our starting dose is 20 mg/m2.
DORFF: Does anyone ever try to increase cabazitaxel to 25 mg/m2 after they start at 20 mg/m2?
DEKKER: I participated in the clinical trial that originally led to approval in the phase 2 setting, and 25 mg/m2 even at that time was very difficult.
DISCUSSION QUESTION
- Have you used carboplatin plus cabazitaxel? In what scenario(s) did you use it?
FARJAMI: I’ve used carboplatin and cabazitaxel, and we have had patients [for] whom we are going back to carboplatin plus a taxane regimen post cabazitaxel.
DORFF: So it’s like a third-line regimen in that setting?
FARJAMI: As a third-line regimen in fit patients who are waiting for lutetium Lu 177 vipivotide [tetraxetan]. The other thing that I sometimes use carboplatin in is HRD [homologous recombination deficiency] mutations—so in patients [whom] we have treated with PARP inhibitors.
DORFF: Yes, that makes sense.
KRIJANOVSKI: Certainly, in patients with low PSA, I use carboplatin plus cabazitaxel.
DORFF: A low PSA? Yeah, that’s one of the aggressive variant characteristics.
BAGHIAN: A CDK12 mutation. There were some reports that showed that it’s a negative prognostic marker. A case series showed improvements with patients who had that mutation when given carboplatin plus cabazitaxel.
DORFF: There are emerging prognostic markers that suggest resistance to taxanes, and that would be another group [for whom] it would make a lot of sense to use the combination.
JANG: In the MAGNITUDE trial [NCT03748641], the patients with CDK12 mutation in HR [hormone-resistant] disease didn’t respond well.3 It implies that the [platinum-based chemotherapy] may not work very well in that setting, so one might want to think again. Because as far as I know, in HR patients, CDK12 is the only one that had no significant benefit. They looked at ATM and the whole array of HRR [homologous recombination repair] genes, and what they noticed is that the CDK12 is the one that doesn’t respond, and the ATM also has minimum response. So it implied that [platinum-based chemotherapy] may not work too well in the CDK12-positive patients.
DORFF: In patients with an HRR alteration, might you think of adding carboplatin to cabazitaxel?
JANG: Definitely in the PALB- and BRCA-positive patients, we know that they’re going to be more platinum sensitive. It’s an array of responses, so we must consider that, but for the BRCA and PALB mutations, I will consider carboplatin.
DORFF: If we think about a patient who does great with docetaxel, they’re responding, they’re not getting neuropathy, so we keep going and we get to 8 or 10 cycles, does that have any influence on what treatment you think they might do well with in the future? Is that a positive or negative for cabazitaxel or for other treatments?
JANG: I think it implies that they’re going to handle chemotherapy well. If somebody can handle 8 cycles of docetaxel without significant neuropathy or major myelosuppression, you know this is a good candidate. Maybe they have good bone marrow reserve. They should do well on cabazitaxel.
REFERENCES
1. Merseburger A, Attard G, Boysen G, et al. A randomized, double-blind, placebo (PBO)- controlled, phase 3b study of the efficacy and safety of continuing enzalutamide (ENZA) in chemotherapy-naïve, metastatic castration-resistant prostate cancer (mCRPC) patients (pts) treated with docetaxel (DOC) plus prednisolone (PDN) who have progressed on ENZA: PRESIDE. J Clin Oncol. 2022;40(suppl 6):15. doi:10.1200/JCO.2022.40.6_suppl.015
2. Bakht MK, Hayward JJ, Shahbazi-Raz F, et al. Identification of alternative protein targets of glutamate-ureido-lysine associated with PSMA tracer uptake in prostate cancer cells. Proc Natl Acad Sci U S A. 2022;119(4):e2025710119. doi:10.1073/pnas.2025710119
3. Efstathiou E, Smith MR, Sandhu S, et al. Niraparib (NIRA) with abiraterone acetate and prednisone (AAP) in patients with metastatic castration-resistant prostate cancer (mCRPC) and homologous recombination repair (HRR) gene alterations: second interim analysis (IA2) of MAGNITUDE. J Clin Oncol. 2023;41(suppl 6):170. doi:10.1200/ JCO.2023.41.6_suppl.170
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More