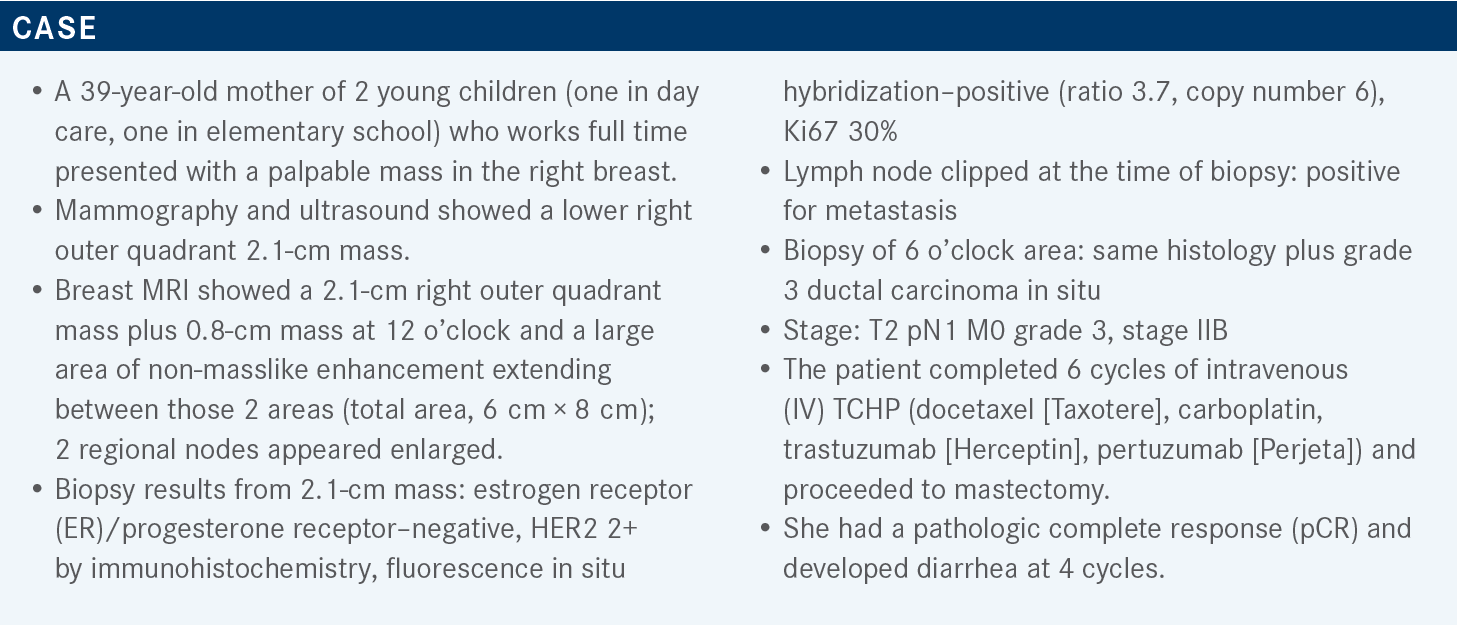
Mamounas Discusses Treatment Combinations in HER2-Positive Early-Stage Breast Cancer
During a Targeted Oncology™ Clinical Case Forum™ event, Terry P. Mamounas, MD, MPH, discussed the treatment landscape for patients with HER2-positive breast cancer.
Terry P. Mamounas, MD, MPH
Medical Director, Comprehensive Breast Program
Orlando Health Cancer Institute
Orlando, FL

Targeted Oncology: What are the recommended regimens for HER2-positive breast cancer?
MAMOUNAS: In the NCCN [National Comprehensive Cancer Network] guidelines, some of the preferred regimens for HER2-positive breast cancer are paclitaxel plus trastuzumab, TCH, [and] TCHP. If there is no residual disease, continue up to 1 year of trastuzumab plus or minus pertuzumab. Otherwise, with residual disease, ado-trastuzumab emtansine [Kadcyla] is an option. Some of the other regimens are anthracycline-containing with docetaxel or paclitaxel.1
Which data support pertuzumab plus chemotherapy and trastuzumab in the adjuvant setting?
There are newer data from the APHINITY trial [NCT01358877], which used adjuvant pertuzumab, trastuzumab, and chemotherapy. A total of 4805 patients were equally randomly assigned to chemotherapy, trastuzumab, and pertuzumab vs chemotherapy, trastuzumab, and placebo, with about 2400 patients in each arm. Randomization was within 8 weeks from surgery, and then the adjuvant anti-HER2 therapy was given for 1 year.2
The primary end point was invasive disease–free survival [IDFS], but its definition was a little bit different from the Standardized Definitions for Efficacy End Points criteria because it didn’t include the second nonbreast primary [tumors]. There was a secondary end point of IDFS with second nonbreast primary [tumors] included, and additional end points like DFS, overall survival [OS], relapse-free interval, distant relapse–free interval, and health-related quality of life.
The stratification factors were nodal status, hormone receptor status, chemotherapy regimen [anthracycline vs nonanthracycline], geographic region, and protocol version A and B. There were 2 versions of the protocol, which doesn’t matter at this point. The clinical cutoff date for the first analysis was December 2016, when the data were first reported, with a median follow-up of about 45.4 months.2
What was the efficacy of the APHINITY trial?
After 8.4 years of follow-up, the data showed an OS rate of 92.7% with pertuzumab vs 92.0% with placebo, which was not statistically significant [P = .078]. The OS for the node-positive cohort had a 1.9% advantage but about a 0.9% disadvantage for the node-negative cohort.
ATTENDEES AT THE TEXAS SOCIETY OF CLINICAL ONCOLOGY 2022 ANNUAL CONFERENCE; FRIDAY, OCTOBER 21, AND SATURDAY, OCTOBER 22, 2022.

The node-negative cohort in this trial has not had any evidence of benefit, but the node-positive cohort had a little bit more. Although, one is not going to see P values here because this is an exploratory subset analysis.3 For the IDFS, which was the original primary end point, there was about a 2.6% difference—88.4% for pertuzumab vs 85.8% for placebo, with a HR of 0.77 [95% CI, 0.66-0.91]—so about a 23% reduction in recurrence. Some of these additional events occurred in patients who were triple positive, ER positive, and HER positive.
For the node-positive cohort, the high-risk patients, there was about a 4.9% absolute difference with an unadjusted hazard ratio of 0.72 [95% CI, 0.60-0.87], so a 28% reduction in recurrence. For the node-negative patients, a 1% advantage for the placebo and the curves was superimposable. But for the node-positive patients, there’s a clinically meaningful difference of about 5% with the addition of pertuzumab.3 The IDFS for the hormone receptor–positive cohort in the original publication had about a 0.4% difference in the arms. But at 8 years follow-up, we see about a 2.8% difference, which is not surprising.
The ER-negative/HER2-positive population [was] overrepresented in the first analysis, but now we see accumulation of events from year 3 to year 8. So with a 2.8% difference and a relative reduction of 0.75 [95% CI, 0.61-0.92], the reduction in recurrence is 25%, like the overall population.3
What data support the use of fixed-dose combination (FDC) subcutaneous trastuzumab/pertuzumab/ hyaluronidase-zzxf (Phesgo) in this setting?
The fixed combination of trastuzumab, pertuzumab, and hyaluronidase or subcutaneous injection is FDA approved for HER2-positive breast cancer. One can use it for anything that you would use IV trastuzumab, so either as neoadjuvant or adjuvant therapy and in the metastatic first-line therapy setting combined with docetaxel.4 There are a lot of studies supporting this. One study supports pertuzumab plus trastuzumab use [NCT00545688]; another study [NCT03493854] evaluated the pharmacokinetics of the FDC compared with IV trastuzumab plus pertuzumab to show that they’re equally effective and have the same concentrations of drug.
The other studies led to the approval of pertuzumab and trastuzumab [NCT00976989, NCT02132949]. The FeDeriCa phase 3 trial [NCT03493854] essentially took patients with operable or locally advanced, inflammatory HER2-positive breast cancer from stage II up to stage IIIc with a primary tumor over 2 cm or node-positive disease—so the neoadjuvant indications. It was the investigator’s choice what type of chemotherapy to give on both arms, either the dose-dense doxorubicin [Adriamycin], cyclophosphamide [Cytoxan], and paclitaxel [Taxol] [ddAC-T] or AC for 4 cycles followed by docetaxel. One arm had IV pertuzumab and trastuzumab, and the other arm had the FDC, which were added to either paclitaxel or docetaxel. Surgery took place, and patients continued whatever formulation they were assigned to before.5 The primary end point was noninferiority of the cycle 7 trough concentration of pertuzumab. The secondary end point was also the cycle 7 trough concentration of trastuzumab as well as the efficacy in terms of pCR comparing the 2 arms.5
How did patients respond on the FeDeriCa trial?
The data of the trough concentration were noninferior. In fact, numerically there was more trastuzumab/pertuzumab in the blood concentration trough at cycle 7. Of course, the dose in the FDC is a little different than the IV dose. The pCR was identical between the 2 groups. That and the noninferiority of the cycle 7 trough concentration of the drugs led to the approval of the FDC. The adverse events for the IV and the FDC are similar, except for the local reactions. Diarrhea, cardiac dysfunction, interstitial lung disease, neutropenia are all similar between the 2 arms. Most of them were grade 1 and 2.5
The time of administration of the IV vs subcutaneous FDC differ. IV pertuzumab is given over 30 to 60 minutes, and then 30 to 60 minutes for observation, and then another 30 to 90 minutes for trastuzumab, and 120 to 360 minutes for observation. So the whole experience may be up to 6 hours vs 5 to 8 minutes for subcutaneous FDC injection and then 15 to 30 minutes for observation.6
ATTENDEES AT THE TEXAS SOCIETY OF CLINICAL ONCOLOGY 2022 ANNUAL CONFERENCE; FRIDAY, OCTOBER 21, AND SATURDAY, OCTOBER 22, 2022.

What other trials have looked at this regimen in HER2-positive breast cancer?
The second study on subcutaneous FDC was the PHranceSCa study [NCT03674112], which was a study of patient preference. They asked patients which formulation they preferred. They took patients with HER2-positive early-stage breast cancer who had completed neoadjuvant pertuzumab, trastuzumab, chemotherapy, and surgery.
The 160 patients were then randomly assigned 1:1 to either IV trastuzumab and pertuzumab or the subcutaneous FDC pertuzumab and trastuzumab for 3 cycles. They collected toxicity information and then they switched patients from the IV to subcutaneous arms or vice versa for another 3 cycles. After this, patients selected which formulation they wanted to continue for 18 cycles.7
The primary end point was patient preference, and there were a lot of secondary end points. To make a long story short, 85% of the patients preferred the subcutaneous formulation over the IV, and 15% preferred the IV. For the continuation formulation, 87% chose the subcutaneous formulation after experiencing both methods.7 The main reasons for the subcutaneous preference were less time in the clinic and more comfortable administration. If you look at the reasons for choosing the IV, I think it was mostly habit. They had the IV, so [they wanted to] continue the IV, but most wanted the subcutaneous.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Breast Cancer, version 3.2022. Accessed February 6, 2023. https://bit.ly/3JExrFT
2. Piccart M, Procter M, Fumagalli D, et al. Interim overall survival analysis of APHINITY (BIG 4-11): a randomized multicenter, double-blind, placebo-controlled trial comparing chemotherapy plus trastuzumab plus pertuzumab versus chemotherapy plus trastuzumab plus placebo as adjuvant therapy in patients with operable HER2-positive early breast cancer. Presented at: 2019 San Antonio Breast Cancer Symposium; December 10-14, 2019; San Antonio, TX. https://bit. ly/3wZnPOq
3. Loibl S, Jassem J, Sonnenblick A, et al. VP6-2022: Adjuvant pertuzumab and trastuzumab in patients with early HER-2 positive breast cancer in APHINITY: 8.4 years’ follow-up. Ann Oncol. 2022;33(9):P986-987. doi:10.1016/j.annonc.2022.06.009
4. Phesgo. Prescribing information. Genentech Inc; 2020. Accessed February 6, 2023. https://bit.ly/3HBdQnl
5. Tan AR, Im SA, Mattar A, et al; FeDeriCa study group. Fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection plus chemotherapy in HER2-positive early breast cancer (FeDeriCa): a randomised, open-label, multicentre, non-inferiority, phase 3 study. Lancet Oncol. 2021;22(1):85-97. doi:10.1016/S1470-2045(20)30536-2
6. DuMond B, Patel V, Gross A, Fung A, Weber S. Fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection in patients with HER2-positive breast cancer: a multidisciplinary approach. J Oncol Pharm Pract. 2021;27(5):1214- 1221. doi:10.1177/1078155221999712
7. O’Shaughnessy J, Sousa S, Cruz J, et al; PHranceSCa study group. Preference for the fixed-dose combination of pertuzumab and trastuzumab for subcutaneous injection in patients with HER2-positive early breast cancer (PHranceSCa): a randomised, open-label phase II study. Eur J Cancer. 2021;152:223-232. doi:10.1016/j.ejca.2021.03.047