Roundtable Discussion: Hammers Breaks Down Efficacy of Combination Therapy in Clear Cell Renal Cell Carcinoma
During a Targeted Oncology™ Case-Based Roundtable™ event, Hans Hammers, MD, PhD, and participants discussed their experiences using lenvatinib to treat patients with advanced clear cell renal cell carcinoma.
Hans Hammers, MD, PhD (Moderator)
Professor, Department of Internal Medicine
UT Southwestern Medical Center
Dallas, TX
CASE SUMMARY
A 59-year-old African American woman with a left renal mass underwent left radical nephrectomy in December 2019, revealing clear cell renal cell carcinoma (RCC). Nine months later, she developed nodules in both lungs, with mediastinal (35 × 38 mm) and retroperitoneal lymph nodes. A lung biopsy confirmed stage IV RCC with clear cell histology and a Karnofsky performance status of 90%. Her hemoglobin level was 11.1 g/dL, and her corrected calcium, neutrophils, and platelets were within normal limits. The patient then received pembrolizumab (Keytruda) plus lenvatinib (Lenvima) as part of a clinical trial.
DISCUSSION QUESTIONS
- Do you have experience using lenvatinib in RCC, with either everolimus (Afinitor) or pembrolizumab?
- What are your reactions to the data from the CLEAR study (NCT02811861) of lenvatinib plus either pembrolizumab or everolimus? How will you counsel patients regarding this regimen?
- What is your impression of the safety/tolerability of this regimen?
- Are you familiar with the recommended dosages for this regimen?
- How will use of this combination in the front line impact your second-line decision-making?
HAMMERS: Who has experience with lenvatinib in RCC, either in combination with everolimus or pembrolizumab? What has your experience been?
KLARNET: I’ve used this combination. In fact, we just had a patient whom I saw today. She had a nephrectomy in 2008 and just now recurred with pulmonary metastasis at quite a long interval [in order to] properly choose this regimen. I’ve used it before, and we have to watch for the hypertension, but it’s an effective regimen to use.
HAMMERS: Hypertension is a common issue, so I like to see patients have their blood pressure controlled before I start this particular regimen. I have a low threshold. If the patient is not yet on blood pressure medicine, start them on a calcium channel blocker, an angiotensin-converting enzyme inhibitor, or whatever your favorite agent is.
Also work closely [with their cardiologist], if they already see a cardiologist, or with the primary care physician to give an early warning that this patient will most likely need to see them for blood pressure [management].
MUKHERJEE: I’ve used lenvatinib with pembrolizumab, and patients generally tolerate [this regimen] pretty well. Initially, there is a bit of a run-in with diarrhea and hand-foot [syndrome], so I’ve never [ended] up using the full dosage. I’ve had to dose reduce a little, but this is otherwise a pretty well-tolerated regimen.
IGID: I have used this regimen, as well. Leading into it, I already thought I [would] probably dose reduce just [from] looking at the studies, and I did. It was for the hand-foot syndrome, not so much [for] the vascular adverse events [AEs].
HAMMERS: Do some of you dose reduce right away, or do some of you work more with breaks [in treatment]? I’m just curious, because some of us treat for 1 or 2 weeks, give some breaks, then just restart at the same dose.
GALAMAGA: Yes, I would say that understanding the toxicities, I usually start low and ramp up…. My frustration with these studies is the comparator, just like in lymphoma studies where our comparator was chlorambucil [Leukeran], which nobody uses. Sunitinib [Sutent] is a great comparator, but [where] is the ipilimumab [Yervoy] plus nivolumab [Opdivo] comparator?
It’s hard to say this [regimen] is clearly superior. The struggle is: Where do I use my immuno-oncology [IO]/IO combination vs a tyrosine kinase inhibitor [TKI]/IO combination? Why would it work for one patient vs another? What are the molecular characteristics of certain patients that would lead me to one direction? That’s my struggle as we move forward to these regimens, which are great. They give us a lot of choices, but the struggle is saying, “OK, which is superior? Which is the best among the best that we have available?”
HAMMERS: Yes, I agree. Many of us would love to see randomized trials comparing one regimen vs another, unfortunately, that will not happen. Even in the cooperative groups there was some brief discussion around it, but that may never happen, but I think you’re absolutely correct. It’s important to look at the aggregate of the data and the long-term outcomes, as there are differences between these regimens. What kind of patients would you choose this regimen for?
AMBIKA: Before that, a quick question: What do you think about the OPTIC [RCC] trial [NCT05361720] design—the VEGF signature vs the IO signature? That sounds promising, when it comes to the biomarker. I was wondering [whether] you have an opinion about it.
HAMMERS: Yes. I don’t want to digress too much. I have a strong opinion about it, so take this with a grain of salt. The problem is that some of these signatures were derived in a regimen that has nothing to do with the one they want to randomize it to. I would say that signature was negative in the CheckMate 214 biomarker study [NCT02231749]. We will get some more data on the [CheckMate] 9ER study [NCT03141177]. Pay attention to that, [whether] it works there. It’s not as clean-cut and not as easy to predict responses from signatures derived in one combination and apply them to another. That’s probably the fairest way to describe it. It’s interesting to do some of these studies, but we have to learn a lot more.
AMBIKA: Yes, so I would use this mostly in patients with a lot of liver disease burden, where you want an immediate response and, for example, [for patients with] liver metastases, in those kinds of situations. Maybe even in patients with a lot of [central nervous system] disease. I had more trouble with this combination in a few patients. I had a patient who developed troponin leakage, and I was worried whether it was myocarditis from the IO therapy. It turned out it was more from the lenvatinib.
HAMMERS: Yeah, the troponin is a complicated thing. In fact, at UT Southwestern [Medical Center], we now tend to get a baseline troponin [level], quite frankly because a lot of patients are actually vascular bypass, so you may get some feeling about that a little earlier, even before getting the baseline. It can be quite helpful.
How do you counsel patients when you start them on this regimen? What do you tell them about this regimen? How do you start that discussion?
AMBIKA: Yes, I’ll tell the patients that among the [combinations], if you just go with the complete response rate numbers, this one is superior, at least numerically.1 However, depending on the profile, you can expect AEs. My feeling is that if we can get the patients through the first 3 to 4 months, most of them will do pretty well after that.
HAMMERS: OK. What do you think about the safety and tolerability? When you hear that 70% of the patients will dose reduce,1 is that something that makes you shy away from a regimen like this? Or is it more like, “Well, we are used to TKIs and all these things, and we’re not that scared?” What are your thoughts when you hear some of those numbers?
MUKHERJEE: [It is important to] educate the patients on what to expect, like making sure they have loperamide [Imodium] and that they know they’re going to have some degree of hand-foot syndrome and to let us know so we can either interrupt or dose reduce. As long as the patients are aware of what to expect. Nowadays, there’s not a lot of mucositis like [there was] when I started with cabozantinib [Cabometyx] and sunitinib. [However], with the lowering of the dose, these patients have been able to tolerate this regimen better.
HAMMERS: Yes. Dr Galamaga said he likes to start at the lower dose [and] maybe ramp up. Who among you does the same thing, seeing these data? Is this a common theme, or is everybody different here?
I’ve heard about the ramping up, but I haven’t done that approach. It makes sense, though. When I counsel my patients, I guess 70% [have AEs], [but] that doesn’t discourage me from giving this drug. I do tell my patients that they likely will have some [AEs]. A lot of it is expectation management, because you don’t want them to get discouraged after the first round, then not even try dose reductions.
The initial discussion is important [to ensure] patients are kept on the regimen. I just encourage them [and tell them that] if we have to dose reduce, we have to. A lot of times, my experience is that patients do tolerate it. [The rate of dose reductions is] not 70%, at least in my cohort of patients.
HAMMERS: Does anyone else have thoughts [regarding] safety, toxicity, or discussion with patients?
HAO: I haven’t used this regimen, but if I use it, I will probably start with a lower dose and then ramp it up. With lenvatinib, I’m a little concerned, from my experience in [hepatocellular carcinoma], even [with] a lower dose. I have a patient who has profound fatigue, which is very hard to control. Having listened to you [here today, I think] the fatigue is probably just an individual experience. So if I use this regimen, I would start with a lower dose and ramp it up.
HAMMERS: Yes, and these are all fair things. You care about your patients, and you want safety. Familiarity with the regimen will grow with time as you use it.
Coming back to that, you are used to using lenvatinib in the second-line and third-line settings, so if you were to move this up into the first line, what would you then do in the second line? Does that impact your decision-making? Do you think, “Well, if I use this first, what am I going to use in the second or third line?” What are your thoughts in that regard?
GAO: Dr Hammers, I probably did not catch all the information for the [phase 3] CLEAR trial. Did they look at the overall survival [From the Data2]?
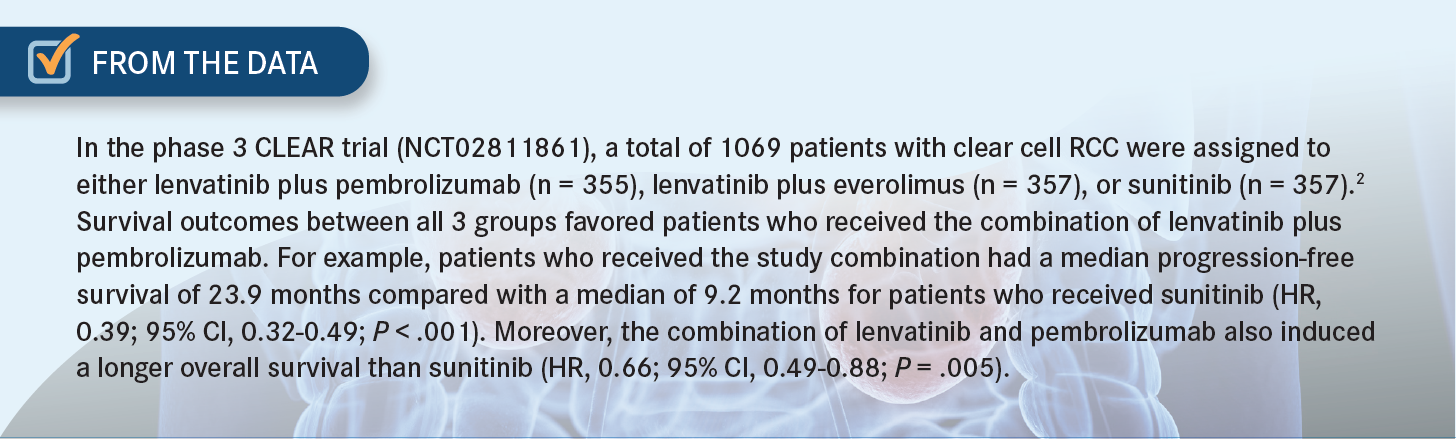
HAMMERS: Yes, they looked at [overall survival], and it was positive [for lenvatinib plus pembrolizumab vs sunitinib [HR, 0.72; 95% CI, 0.55-0.93].3
GAO: At the beginning of the COVID-19 pandemic, I talked with my patients about this regimen. A lot of my patients heard that we were going to use infusion plus a pill and that they [would] have to travel to the infusion site regularly to receive the treatment in addition to the [radiation and chemotherapy].
A lot of them chose to just use the TKI after I revealed all the pros and cons, including the progression-free survival and that [we could] reserve the IO therapy for the second line. So, I’m thinking that for some patients, after we rotated the TKI, if they still had progressive disease or they could not tolerate more treatment with a TKI, we could certainly use the combination of lenvatinib with ipilimumab or the combination of pembrolizumab with ipilimumab.
In addition to that, once you start the infusion, some patients [get] a central line or chest port, and then they have to carry the port the whole time. Even if you stop the pembrolizumab after 2 years, they have to travel to the infusion center and flush the port every 6 to 8 weeks. This is something that, when we talk with the patient, it would be better to just let them know first.
HAMMERS: Yes, certainly. During COVID-19, I think all of us made some adjustments to how we do this. [However], I would say for most of us, and for me, I like to [use] IO therapy early. But personally, I almost never place a port if the patient doesn’t have bad veins, simply because it doesn’t matter if [the drug] extravasates, because you don’t cause any tissue damage. In fact, they’re working now on subcutaneous administration of this antibody. You will see trial data coming. Patients cannot get any of the PD-1 inhibitors subcutaneously; that’s going to be a major change that will hopefully help with some of that.
REFERENCES
1. Choueiri TK, Eto M, Kopyltsov E, et al. Phase III CLEAR trial in advanced renal cell carcinoma (aRCC): outcomes in subgroups and toxicity update. Ann Oncol. 2021;32(suppl 5):S678-S724. doi:10.1016/annonc/annonc675
2. Motzer R, Alekseev B, Rha SY, et al; CLEAR Trial Investigators. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289-1300. doi:10.1056/NEJMoa2035716
3. Porta CG, Eto M, Motzer RJ, et al. Updated efficacy of lenvatinib (LEN) + pembrolizumab (PEMBRO) vs sunitinib (SUN) in patients (pts) with advanced renal cell carcinoma (aRCC) in the CLEAR study. Ann Oncol. 2022;33(suppl 7):S660-S680. doi:10.1016/annonc/annonc1072
Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Peers Discuss Management of IO/TKI Toxicities and Dosing Strategies in Frontline RCC
March 11th 2025During a Case-Based Roundtable® event, Elizabeth M. Wulff-Burchfield, MD, and other participants discussed their experiences with the frontline combination regimens for advanced renal cell carcinoma.
Read More
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen