Piotrowska Addresses Immunotherapy Treatment in NSCLC With Mutations
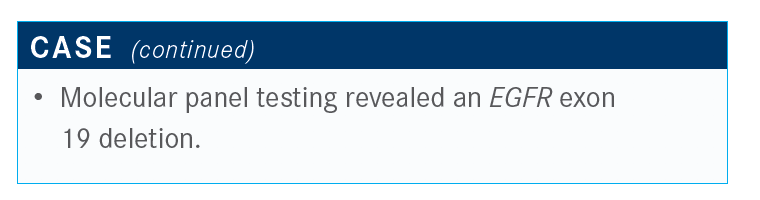
During a virtual Case Based Peer Perspective series, Zofia Piotrowska, MD, discussed the case of a 66-year-old man with non–small cell lung cancer and a genetic mutation.
Zofia Piotrowska, MD

During a virtual Case Based Peer Perspective series, Zofia Piotrowska, MD, assistant professor,Harvard Medical School Massachusetts General Hospital in Boston, MA, discussed the case of a 66-year-old man with non–small cell lung cancer and a genetic mutation.
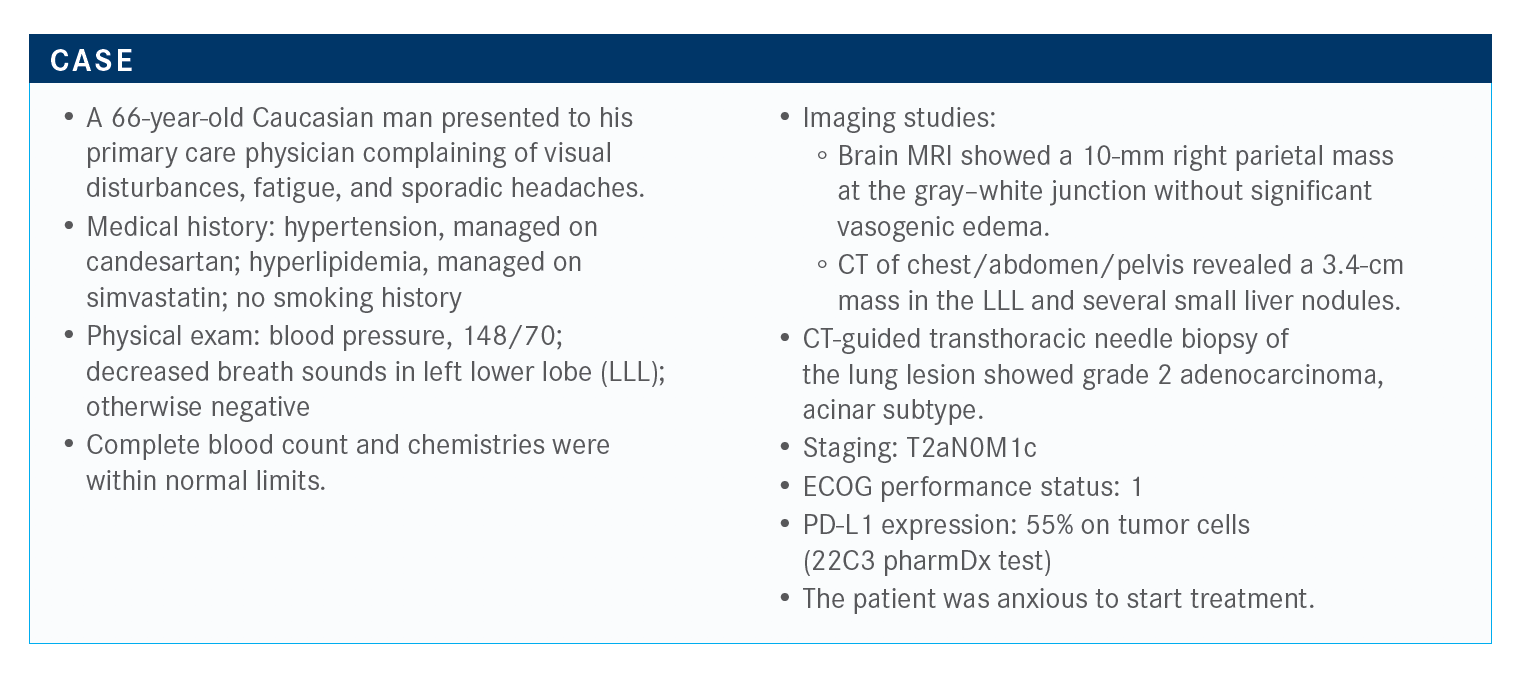
Targeted Oncology™: Would you have sent out for molecular testing if this patient had squamous cell histology?
PIOTROWSKA: The recommendations [for biomarker testing] are for the patients with adenocarcinoma and nonsquamous histology. Although if you look in the updated NCCN [National Comprehensive Cancer Network] guidelines, what they say is that for patients with squamous cell histology, consider molecular testing in patients with particular features, such as neversmokers and younger patients.1
We rarely do testing in these patients, but sometimes find targetable drivers in squamous cell carcinoma. Or they have adenosquamous disease and you’ve picked up a squamous component.
What targetable drivers are you testing for in your practice?
I have been impressed with the flurry of activity from the FDA recently. It feels as though every Friday, I’m getting multiple emails about new approvals, both in the immunotherapy space and with several new targeted agents, including selpercatinib [Retevmo] for RET fusion–positive lung cancer2 and capmatinib [Tabrecta] for MET exon 14 skipping mutations.3 Both are new targets that now have an FDA-approved [indication] as of May of this year.
What that translates to is the fact that the list of recommended targets that we should be testing for is rapidly increasing. You can see the minimum testing list here now includes 6 genes and PD-L1. The NCCN guidelines…emphasize the fact that, when possible, broad NGS [next-generation sequencing] should be used and is more practical.1
I think it’s a lot easier to do that than doing sequential tests for EGFR and ALK first and then going back to that tissue to run the next test, the way that we used to do it. If you can get all these answers in one fell swoop, it saves tissue and gives you more information.
At this point, would you start the patient on chemoimmunotherapy or a targeted agent considering their molecular testing?
The guidelines [recommend that] for patients who have an oncogene, you should use a targeted therapy before using immunotherapy. Even with immunotherapy, we can reserve that for possibly after chemotherapy for these patients.
[There was] a small study…that was prospectively done. It planned to look at patients with known EGFR-positive disease, high PD-L1 [expression] greater than 1%, although the majority of patients had greater than 50% expression, and treated patients with first-line pembrolizumab [Keytruda].4
The planned enrollment was 25 patients, but it was terminated early after the first 11 patients were accrued because of lack of efficacy. What we saw among these 11 patients was that there was 1 response. However, that patient turned out not to have an EGFR mutation on confirmatory testing. The patients were treated with pembrolizumab. They did not respond. And then, as we often would, they were then put on a TKI [tyrosine kinase inhibitor] subsequently.4
There were 2 deaths on the study out of 11 patients. One was attributed to pneumonitis. There was also grade 3 hepatitis. This was a small study, but I think a striking number of bad outcomes in these patients treated with TKIs after immunotherapy emphasizes the fact that using first-line pembrolizumab may not only be ineffective, but more importantly, may limit our ability to deliver more effective therapy down the road.
A review that came out of Memorial Sloan Kettering [Cancer Center] last year looked at 41 patients who had received immunotherapy, PD-1 or PD-L1 blockade, followed by osimertinib [Tagrisso]. We saw a signal for high rates of pneumonitis that was worrisome. Fifteen percent of patients had developed pneumonitis with a median onset of 20 days after osimertinib. All of them required treatment with steroids, and most required hospitalization.5
Interestingly, this did not occur when patients received a TKI followed by PD-L1 blockade. This seemed to be more common of an effect with osimertinib [following immunotherapy], where the rate of severe immune-related AEs [adverse events] was 15% versus erlotinib where 0 out of 20 patients had a severe immune-related AE.5
This is important to be aware of. I saw a patient just this week who had a cycle of carboplatin and pemetrexed [Alimta] plus pembrolizumab and then was about to start osimertinib, and I advised waiting because I was worried. I often get asked how long you should wait to start osimertinib, but we don’t have a great answer to that question. We know the immunotherapy drugs have a long half-life. But in this study, it did seem as though the 3-month mark was at least a sign indicating that…patients seemed to do better than starting within 3 months of pembrolizumab.
Would you use bevacizumab (Avastin), as it has been shown to work better for patients who have an EGFR or ALK alteration?
The study you’re referring to is IMpower150 [NCT02366143], which looked at the quadruplet combination of carboplatin, paclitaxel, bevacizumab, and atezolizumab [Tecentriq]. Unlike in KEYNOTE-189 [NCT02578680], which excluded EGFR-positive disease, IMpower150 with the 4-drug regimen, some I’ve heard call it the kitchen sink approach, did include EGFR-positive tumors. The number of patients on that study with sensitizing EGFR mutations was relatively small, but they did see a benefit in the overall study for the combination of the 4-drug combination versus chemotherapy alone. Interestingly, what we saw was that the benefit was not upheld in the chemoimmunotherapy arm without the bevacizumab, suggesting there seemed to be some magic to the [addition of the] agent.6
For my patients progressing on a TKI, I haven’t widely adopted the IMpower150 regimen. I find it to be tougher [to tolerate] than carboplatin/pemetrexed for these patients, which I think can work well and is generally well tolerated. The rates of neuropathy and alopecia are big concerns. But I do know others that have used it, and I think if you wanted to use immunotherapy in a young, fit, and robust patient who really wants to give it a shot, that would probably be the regimen. It would be the most data-driven option in terms of a chemotherapy and immunotherapy regimen for these patients.
Do you ever use bevacizumab along with carboplatin and pemetrexed or the chemotherapy alone?
I do sometimes, but not always. I find that it adds toxicity. I used to use it more. I don’t know if there’s a reason, or if we’ve just all become used to using carboplatin and pemetrexed plus pembrolizumab. I will use it if I have a patient for whom we’re trying to throw everything at, but don’t want to use immunotherapy.
The other thing, and this is off label, but for a patient who has brain metastases on osimertinib that are well controlled but have systemic disease progression, I worry that the osimertinib is providing some ongoing CNS [central nervous system] control. In those cases, I’ve sometimes put them on carboplatin and pemetrexed and continued the osimertinib, and I find that that’s generally well-tolerated. There’s a little bit more myelosuppression. It can help [prevent] brain progression. I’ve had a few patients where it’s been stopped, and then the brain kind of explodes, even despite the CNS penetration of pemetrexed.
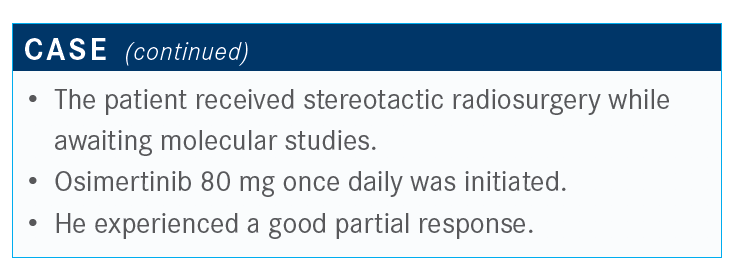
What data support the initiation of osimertinib therapy?
This is one of the more important studies to review, the FLAURA trial [NCT02296125] that looked at first-line osimertinib versus first-generation EGFR inhibitors. These were patients who were treatment-naive with exon 19 deletion or exon 21 L858R mutations and good performance status. There were nearly 560 patients in this study, and they were randomized to either osimertinib or the standard of care, which could be either erlotinib [Tarceva] or gefitinib [Iressa], with a primary end point of progression-free survival.7
What we saw was that osimertinib significantly improved the progression-free survival, nearly doubling it from 10.2 to 18.9 months, with a hazard ratio of 0.46 [95% CI, 0.37-0.57; P < .001]. We then see the updated overall survival data, which was just published at the beginning of this year in the New England Journal of Medicine, we see an improvement in these patients from 31.8 months to 38.6 months and a hazard ratio of 0.80 [95.05% CI, 0.64-1.00; P = .046).8
People ask about the rates of crossover. Of the patients in the standard-of-care arm who went on to receive our subsequent treatment, 50% of them did go on to receive osimertinib. Even with that rate of crossover, we still saw a survival benefit [with the TKI]. I think taking these data together, FLAURA has been a practice-changing study, certainly here in the United States and in Europe.
What is the difference between EGFR exon 19 and exon 21 mutations?
The magnitude of benefit in this study, and particularly with overall survival, was higher in the exon 19 deletion population than the L858R population. I think this is consistent with the fact that we’ve known from prior studies that patients with deletion 19 tend to do better. In general, that hasn’t affected my practice. I still use osimertinib for those patients, but they do tend to do less well.
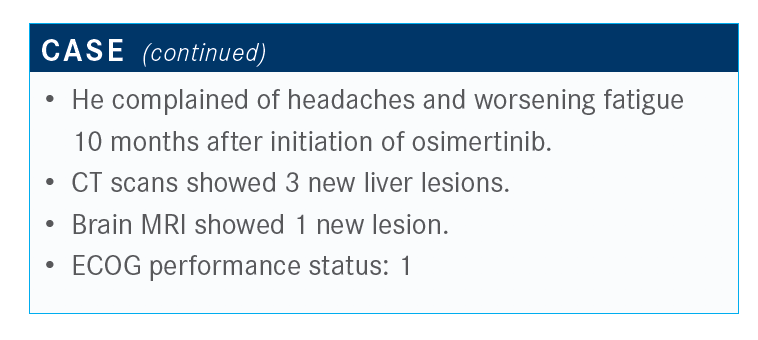
What do you do for patients who progress on osimertinib? Do you order testing, and, if so, what type?
This is not a common scenario because many of these patients do well for a long time. The resistance mechanisms, in some ways, were easy to plan for when patients progressed with first-generation EGFR inhibitors. Half of patients [developed a] T790M resistance mutation. Then you would put them on osimertinib, and it was simple.
It’s a lot more complicated with osimertinib resistance, and there’s no main driver of resistance. There are some common themes. The C797S mutation is a tertiary mutation that can lead to osimertinib resistance. It develops in about 20% of patients who received second-line osimertinib and, so far, from the data we’ve seen, it may be even less common [after use in the] first-line setting.
People talk about when the fourth-generation EGFR inhibitor is going to come out. Unfortunately, I think it won’t be quite this magic bullet that osimertinib was, because so few of these patients tend to have this mutation. It’s not going to be as effective across the board to target it.
A subset of these patients, probably up to 20%, develop MET amplification. Right now, I’ll tell you frankly, that’s something that I’m hoping to find in my clinical practice because we do have some data from the TATTON trial [NCT02143466] which showed that patients could then go on to a combination of a MET and EGFR inhibitor.9 Those are patients who certainly could access clinical trials. Or you can also consider off-label osimertinib plus crizotinib [Xalkori]. There have been some case reports that can be referenced.
There is also a subset of these patients who develop histologic transformations, and this is the 1 point where I’d caution against looking at liquid biopsies, because a subset of these patients will have transformation to small cell lung cancer. Now, we’ve also seen [transformation] to squamous cell histology. If nothing else, that will impact chemotherapy selection. You will miss that on a liquid biopsy, particularly if you have a patient who has rapid disease progression that for whom you think the clinical characteristics have changed. I do think it’s important to consider a tissue biopsy, because if they have small cell lung cancer, then you have to get them on the etoposide-based therapy.
References:
1. NCCN Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 6.2020. National Comprehensive Cancer Network. June 15, 2020. Accessed June 15, 2020. https://bit.ly/2BhS49Z
2. FDA approves selpercatinib for lung and thyroid cancers with RET gene mutations or fusions. FDA. May 8, 2020. Accessed July 20, 2020. https://bit.ly/2OHeKUj
3. FDA grants accelerated approval to capmatinib for metastatic non–small cell lung cancer. FDA. May 6, 2020. Accessed July 20, 2020. https://bit.ly/2WF7lJp
4. Lisberg A, Cummings A, Goldman JW, et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1+, tyrosine kinase inhibitor na.ve patients with advanced NSCLC. J Thorac Oncol. 2018;13(8):1138-1145. doi:10.1016/j.jtho.2018.03.035
5. Schoenfeld AJ, Arbour KC, Rizvi H, et al. Severe immune-related adverse events are common with sequential PD-(L)1 blockade and osimertinib. Ann Oncol. 2019;30(5):839-844. doi:10.1093/annonc/mdz077
6. Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for fi rst-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa1716948
7. Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non–small-cell lung cancer. N Engl J Med. 2018;378(2):113-125. doi:10.1056/NEJMoa1713137
8. Ramalingam SS, Vansteenkiste J, Planchard D, et al. Overall survival with osimertinib in untreated, EGFR-mutated advanced NSCLC. N Engl J Med. 2020;382(1):41-50. doi:10.1056/NEJMoa1913662
9. Oxnard GR, Yang JC, Yu H, et al. TATTON: a multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann Oncol. 2020;31(4):507-516. doi:10.1016/j.annonc.2020.01.013

Key Trials From ASH 2024 Impact Treatment for Plasma Cell Disorders Going Forward
February 20th 2025Peers & Perspectives in Oncology editorial board member Marc J. Braunstein, MD, PhD, FACP, discussed the significant advancements in multiple myeloma treatment at the 2024 ASH Annual Meeting and Exposition.
Read More