Heymach Compares Chemoimmunotherapy Regimens for ES-SCLC
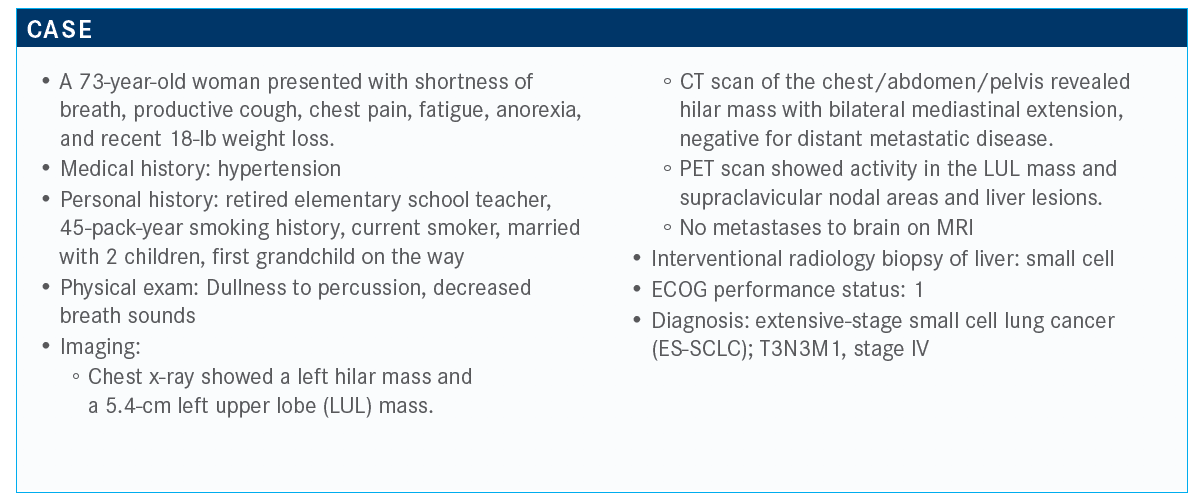
John V. Heymach, MD, PhD, reviewed the case of a 73-year-old women with extensive-stage small cell lung cancer during a virtual Case Based Peer Perspective event.
John V. Heymach, MD, PhD

John V. Heymach, MD, PhD, chair of Thoracic/Head and Neck Medical Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX, reviewed the case of a 73-year-old women with extensive-stage small cell lung cancer (ES-SCLC) during a virtual Case Based Peer Perspective event.
Targeted Oncology™: What percentage of your patients do you start in the inpatient setting?
HEYMACH: For me, it’s probably 10% to 15%, if I had to guess—a handful of patients in the last year. Sometimes it’s because of superior vena cava [SVC] syndrome or a collapsible lung [that]
they’re admitted. I’ll start [the patient] as an inpatient often. One other thing I’ll mention—and we always mention this to fellows—is that even if you have lung collapse or SVC syndrome,
you can still start chemotherapy or chemoimmunotherapy. You don’t need radiation, because chemotherapy will work quickly in general.
What would your treatment approach be in this case?
The approach here [is] chemotherapy or chemoimmunotherapy there anything else you would do in this setting?
Yes. There were liver metastases here as well. The National Comprehensive Cancer Network guidelines [suggest] chemotherapy and atezolizumab [Tecentriq] or chemotherapy and durvalumab [Imfinzi]. That’s new. That’s just come out in 2020 as an option. Chemotherapy [with] etoposide is still a possibility.1
Just [as a reminder], the durvalumab study was done with either carboplatin or cisplatin. The atezolizumab study was done with just carboplatin. Occasionally people use irinotecan. I can’t think of too many reasons to do it in the first-line setting.
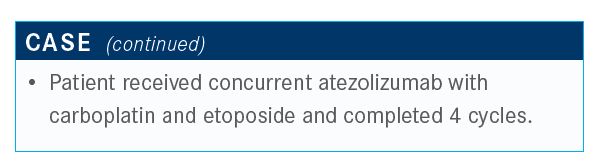
What are the data that support the use of this combination in this patient population?
[That would be] the IMpower133 study [NCT02763579].2 It used chemotherapy, but the chemotherapy was carboplatin and etoposide for 4 cycles. There’s some controversy because some people said, “Four is undertreating, we often would go to 6.” I think that’s an open issue. Although at the end of the day, it looks like 4 versus 6 probably doesn’t make a lot of difference in terms of the chemotherapy. Anyway, [this study investigated] chemotherapy versus chemotherapy plus atezolizumab, and then atezolizumab maintenance therapy is part of the regimen.
It was raised before [that these results were] not a home run, but it was a clear, significant, positive result. The difference is about 2 months in median overall survival [OS], so 10.3 versus 12.3 months. The hazard ratio for survival was 0.7 [P = .007], and the progression-free survival [PFS] is barely different [4.3 vs. 5.2 months with atezolizumab; HR, 0.77; P = .02]. You see little difference [in OS] in the beginning. When there’s a difference, it tends to come out later. In fact, it even tends to come out after the chemotherapy is done. If you look at the number of months, 4 cycles of chemotherapy is only 3 months, and at 3 months you see no real difference. It looked like the benefit of atezolizumab was kicking in later in the regimen, suggesting it’s priming the immune system and giving a delayed response.
The 2-year OS difference through the first 8 months [showed] little difference.3 At 1 year, the survival [rate was] 51.9% versus 39.0%. At 18 months, 34.0% versus 21.0%. A 13 [percentage point] increase in your likelihood of being alive at 18 months, 12% at 1 year. That’s a solid and real improvement, even if it’s not osimertinib [Tagrisso], for first-line, EGFR-mutant [disease]. It’s a clear, substantial difference.
Does the benefit seen with atezolizumab extend to patients with other high-risk features? Do any of these subgroups inform your use of atezolizumab?
There were broad benefits [with] the addition of atezolizumab. Maybe a little less benefit with brain metastases [HR, 0.96], but across the board, this is broadly helping patients. [With] tumor mutational burden [TMB], there’s a modest effect. At a higher TMB, there was a bit of benefit [HR, 0.58], but the lower TMB still had benefit as well [HR, 0.79]. I don’t use TMB to inform the decision-making here.
The response rate was not higher [64.4% vs 60.2% with atezolizumab]. In fact, it was slightly lower in the atezolizumab group when you look overall. The PFS was not appreciably different. As it was raised before, it doesn’t help response rate or PFS, but it is showing a benefit for OS of 2-months difference.
What are your thoughts on the decision to use carboplatin versus cisplatin?
When oncologists run out of topics to debate, they can always go back to this one. When you look at the cisplatin versus carboplatin data, cisplatin is consistently better. In my practice, if a patient has curable [or] potentially curable disease, limited stage, I use cisplatin. If I’m going to be adding radiation, I use cisplatin or if a patient is young and otherwise healthy, I’ll at least start off with cisplatin instead of carboplatin. For the majority of patients, if they’re in their 70s [or have] any sign of renal dysfunction, in general, I’m starting the majority with carboplatin. The differences between them are likely small in terms of efficacy, and the differences in toxicity are
real. I only will use cisplatin either in a limited-stage case or with a younger patient who wants to be aggressive.
Would you consider substituting cisplatin for carboplatin with atezolizumab?
The IMpower150 [NCT02366143] regimen only used carboplatin for 4 cycles.4 We’ll get to the durvalumab study, the CASPIAN study [NCT03043872] afterward. There, they did use both of them. If I were going to use cisplatin, I would go with durvalumab there, because the data include that.
What data support the use of the other chemoimmunotherapy regimen you mentioned, chemotherapy plus durvalumab?
The study supporting the use of durvalumab is the CASPIAN study.5 The CASPIAN has 3 arms. One is EP and in this case, EP is etoposide and cisplatin or carboplatin, so that’s 1 difference with this study—you can use cisplatin. Second difference is it allowed you to go up to 6 cycles. There was optional prophylactic cranial irradiation after or durvalumab with EP. In this case, it was up to 4 cycles with the platinum followed by durvalumab surveillance. This let you give a more aggressive chemotherapy regimen for up to 6 cycles—a little diff erent than the IMpower150 study. There’s a third arm of durvalumab with tremelimumab, so PD-1 plus CTLA-4 [inhibition]. We don’t have the results yet of that to discuss at this point.
Results look similar to the [IMpower133] study. There was a hazard ratio of 0.73 [P = .0047]. The difference here is about 2.7 months instead of 2 months, 10.3 versus 13 months [with durvalumab]. PFS is a touch longer, but like the other study, PFS is not any longer here [5.4 vs 5.1 months with durvalumab]. It’s a late separation in the curves in both of these studies.
As in the last study, [there was] broad benefit across all major subgroups for small cell. The response rate was a bit higher in the CASPIAN study. With the addition of durvalumab, the response rate goes up to 68% as compared with 58% with EP. If you look at the 12-month [rate of patients] remaining in response, [it was] 23% versus 6%. Your likelihood of continuing the response is substantially higher at 12 months. Whether you get durvalumab or not, at 6 months, both groups are often in response, but it’s later. It looks like what it’s affecting is the duration of response, how long you’re staying in response in this regimen.
What was the safety profile like with this regimen?
The AEs here are interesting; again, [it was] well tolerated. In fact, some of the toxicities occurred at a lower rate in the durvalumab arm than in the EP arm. I’ll be honest, I’m not sure what to make of this, but [the rate of] grade 3/4 neutropenia was 24% versus 33%; anemia, 9% versus 18%. Is this just luck? It’s unclear, but certainly this regimen is not adding signifi cant toxicity and is well tolerated.
How would you compare these 2 chemoimmunotherapy regimens for patients with ES-SCLC?
Interestingly, comparing the IMpower133 and the CASPIAN studies, OS was prolonged in both, up to 12.3 months in IMpower133; 13 months in CASPIAN.2,5 There were no big differences in PFS. For immune-related AEs with the atezolizumab plus EP, it was 41.4% versus 19.6% in the CASPIAN study. There are some theoretical reasons why PD-L1 blockade might have lower toxicity than PD-1, but that’s a big difference. I guess the difference in toxicity is surprising, both using the common toxicity criteria. Is this going to be borne out in subsequent studies? I’m not sure, but that is one of the interesting differences: similar or greater improvement in OS with CASPIAN and this interesting signal of lower toxicities overall.
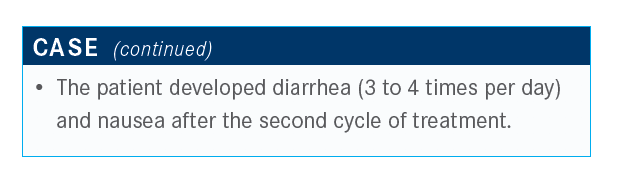
What is your approach to managing the diarrhea in somebody getting immunotherapy like this? How quick are you to jump to a biopsy to see if they have immunerelated colitis?
What makes it even trickier to jump is these patients often are immunosuppressed because of the chemotherapy. I don’t think anybody’s enthusiastic about doing a colonoscopy in the setting of immunosuppression during chemotherapy. I think if you’re just getting immunotherapy, maybe it’s a little easier to jump to a biopsy than during chemotherapy.
I try to wait it out and see if it’s substantial before doing a biopsy to see if it’s colitis or not. Of course, [with] this regimen, we always want to keep that possibility in mind.
What are your thoughts on the 2 options available for immunotherapy: atezolizumab and durvalumab?
There’s a little more flexibility with the [durvalumab] regimen there as well, but it’s good that we do have 2 options, whereas we didn’t have any options before. It’s certainly a win for the patients.
References:
1. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Small Cell Lung Cancer. National Comprehensive Cancer Network. Version 4.2020. Posted July 7, 2020. Accessed July 17, 2020. https://bit.ly/3g2kWCx
2. Horn L, Mansfi eld AS, Szczęsna A, et al; IMpower133 Study Group. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220-2229. doi:10.1056/NEJMoa1809064
3. Reck M, Liu SV, Mansfi eld AS, et al. IMpower133: Updated overall survival (OS) analysis of first-line (1L) atezolizumab (atezo) + carboplatin + etoposide in extensive-stage SCLC (ES-SCLC). Ann Oncol. 2019;30(suppl 5):v710-v717. doi:10.1093/annonc/mdz264
4. Socinski MA, Jotte RM, Cappuzzo F, et al; IMpower150 Study Group. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa1716948
5. Paz-Ares L, Dvorkin M, Chen Y, et al; CASPIAN Investigators. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394(10212):1929-1939. doi:10.1016/S0140-6736(19)32222-6

Kim Evaluates New Regimens for EGFR+ Lung Cancer
January 20th 2025During a Community Case Forum event in partnership with the Medical Oncology Association of Southern California, Edward S. Kim, MD, MBA, discussed the FLAURA2 and MARIPOSA trials of newer regimens for EGFR-positive lung cancer.
Read More
Roundtable Roundup: Lung Cancer Molecular Testing and ALK-Targeted Treatment
January 18th 2025In separate, live virtual events, Vincent K. Lam, MD, and Chul Kim, MD, MPH, discuss molecular assays and treatment options for a patient with metastatic non–small cell lung cancer (NSCLC), with participants.
Read More
Conservative Management Is on the Rise in Intermediate-Risk Prostate Cancer
January 17th 2025In an interview with Peers & Perspectives in Oncology, Michael S. Leapman, MD, MHS, discusses the significance of a 10-year rise in active surveillance and watchful waiting in patients with intermediate-risk prostate cancer.
Read More
What Is Dark Zone Lymphoma, and Is It Clinically Relevant?
January 16th 2025Dark zone lymphoma includes aggressive B-cell lymphomas with shared molecular features. While some respond to escalated treatment, others remain resistant, highlighting the need for targeted approaches to improve outcomes.
Read More