Multiple Drug Types Play a Role in the Myeloma Landscape, Depending on the Line of Therapy
Tulio E. Rodriguez, MD, weighs the various treatment options available for a patient with multiple myeloma.
Tulio E. Rodriguez, MD

Tulio E. Rodriguez, MD, director, Bone Marrow Transplant and Cellular Therapy Program, at Advocate Health Care, in Chicago, IL weighs the various treatment options available for a patient with multiple myeloma.
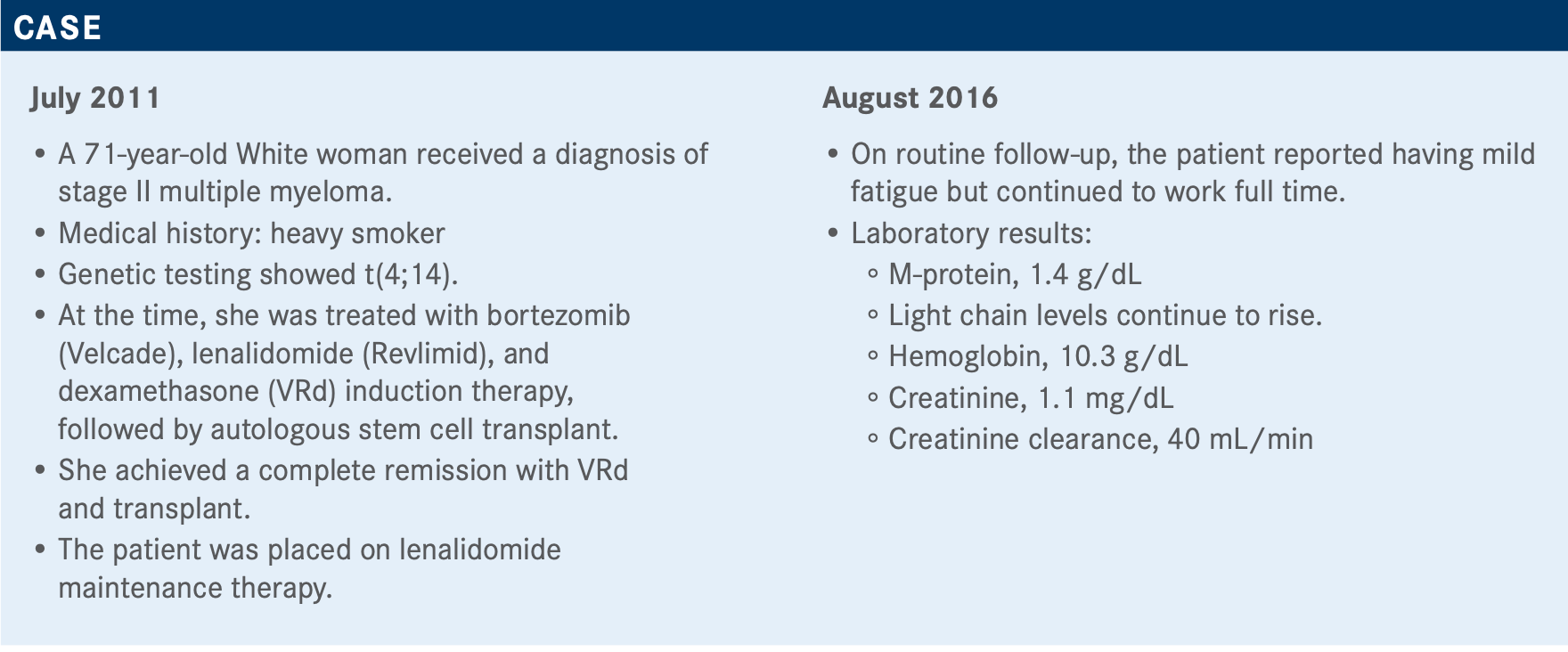
Targeted OncologyTM: As there are several options in this setting, would you use a monoclonal antibody at first relapse, choose another proteasome inhibitor (PI), or switch to another immunomodulatory drug?
RODRIGUEZ: There is no right or wrong answer. It’s secondline therapy. There are several regimens that have been recommended in the NCCN [National Comprehensive Cancer Network] guidelines, but it’s not that we can say we can [choose one] over the other. There are data to support some of these interventions, but certainly, it’s more complex than just the treatment.
What would your consideration be for the next line of therapy for this patient?
You can consider proceeding with reinduction. But it’s going to depend on the performance of the patient at that point and if there’s any further emergence of risk factors.
It’s also going to depend on how the person responded to firstline therapy. I will always consider how the person responded to that therapy and if there was any complication from that therapy. Some people receive PIs and have significant neuropathy; most of the time, it is because of the PIs. They get better, but some other cases persist, and something that we need to keep in mind is that there are other drugs that can cause neuropathy. We know that bortezomib, for example, has been associated with neuropathy, but I’ve seen patients who continue lenalidomide, and 3% or 4% will develop neuropathy with that drug. We need to keep all those factors in mind.
We have NCCN-preferred triplet regimens, and we are used to treating patients with 3-drug combinations. I want to argue that there’s always the patient who is [a good candidate for] a 2-drug combination, but, for the most part...it seems 3 drugs appear to give [better] responses compared with 2 drugs.1
What are some of the data supporting triplets over doublets in this setting?
The CASTOR trial [NCT02136134] compared bortezomib and dexamethasone [Vd] versus daratumumab [Darzalex] with Vd. PFS [progression-free survival] at the time of the analysis, even though the median follow-up was short, was not reached for the experimental combination of daratumumab-Vd and for Vd was reported as 7.2 months [HR, 0.39; 95% CI, 0.28-0.53].2 In the POLLUX trial [NCT02076009], combining the anti-CD38 antibody daratumumab with lenalidomide and dexamethasone [Rd], you saw the same phenomenon. Median PFS was not reached with the combination of daratumumab-Rd in contrast with 13.5 months with Rd [HR, 0.37; 95% CI, 0.27-0.52].3
An interesting study in multiple myeloma is ICARIA-MM [NCT02990338], using isatuximab [Sarclisa] with pomalidomide [Pomalyst] and dexamethasone [Pd]. You have a median PFS of 11.5 months [for that combination] versus 6.5 months for Pd alone [HR, 0.596; 95% CI, 0.436-0.814].4
The duration of response in all 3 trials was very good partial response [VGPR]: 59.2% versus 29.1% (P <.001) for daratumumab-Vd versus Vd in CASTOR, 75.8% versus 44.2% (P <.001) for daratumumab-Rd versus Rd in POLLUX, and 27% versus 7% for isatuximab-Pd versus Pd in ICARIA. They all seem to favor a 3-drug combination.2-4
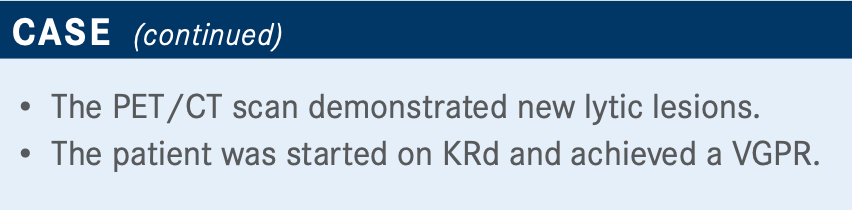
The ASPIRE trial [NCT01080391] used KRd [carfilzomib (Kyprolis), lenalidomide, and dexamethasone], a combination of drugs that we have been using for a long time. Once again, it proved the notion that 3 drugs appear to work better than 2-drug combinations [HR, 0.69; 95% CI, 0.57-0.83]5 for the patient who can manage the 3-drug approach. For patients who might not be in good shape, in contrast to our case, I think that some physicians will approach this by starting with a 2-drug combination and, as soon as performance improves, add the third drug to the therapy.
How has COVID-19 affected your practice?
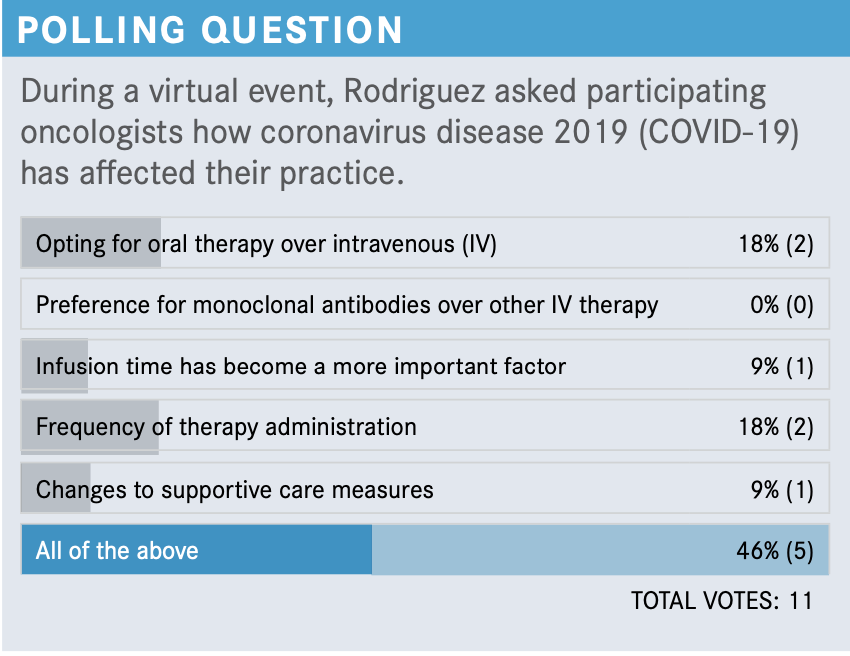
We have been trying to support our patients as much as we can, and we try to avoid changing too many therapies because of the pandemic....That said, [that’s] if we keep the same therapies and same approaches. Some of our practices, the institutions, have even adopted visitor restrictions on caregivers who used to come with the patients.
I have to admit, sometimes we have to go a little bit faster because somebody is waiting for the patient or they’re going to have to pick them up again. That’s been a disruption in some ways. But, for the most part, most of the patients have been receiving the therapy that they need. Our population has been a victim of this pandemic...not only patients with COVID-19 but also those patients with breast cancer, leukemia, and multiple myeloma that require some therapy.
I have one [patient] who insisted on [being treated via] telemedicine, and that was the only way we were able to continue her care—a young woman, actually. So, [fear of COVID-19] is to be taken into consideration, as well.
What factors determine which treatment to use in the second-line setting?
Related factors that we consider when we choose a secondline therapy for patients such as this include being refractory to lenalidomide, age, efficacy, convenience, infusion time, and cost. Also [included are] genetic risk; geography; and comorbidities like renal insufficiency, cardiovascular disease, and performance. We pay attention to the mechanism of action, safety, toxicity to prior therapy, and patients who had neuropathy or pulmonary embolism secondary to prior treatments. These are therapy-related factors we have to keep in mind in patients’ disease factors.
Mechanisms of action are certainly important. This patient received a second-line PI in combination with an immunomodulatory drug and dexamethasone. Those are not surprising. I think carfilzomib, from the standpoint of a PI, is one of the preferred drugs of many oncologists as second-line therapy.
What would the best approach be for this patient in the third line after KRd?
Elotuzumab [Empliciti] has been researched for patients who might be frailer, in whom a quick response is not necessarily something we are pursuing. Dana-Farber [Cancer Institute] was promoting this combination for some time, more for frail patients and patients with not as good performance [status].
New agent combinations for patients with multiple myeloma may change your way of practicing...[for example], CAR [chimeric antigen receptor] T-cell immunotherapy. It is fascinating what is happening with multiple myeloma therapy right now with all these options: immunotherapy with CAR, bispecific T-cell engagers, etc.
[Melflufen] is also a provocative and interesting approach. Watch your [patient’s] eyes, but we are used to that. We’re using the dexamethasone eye drops. It is an interesting mechanism of action in patients who would otherwise probably not have too many options.
We can talk about venetoclax [Venclexta], which has not been approved by the FDA for multiple myeloma. But I’m sure there are data out there and [physicians who] have probably used that drug for patients with multiple myeloma. [There is] also selinexor [Xpovio].
Do you agree with the treatment choice for the patient?
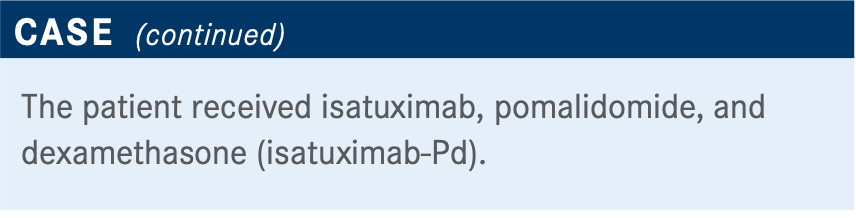
I have used isatuximab several times in that combination with Pd. The ICARIA-MM study used the anti-CD38 antibody isatuximab with Pd for relapsed/refractory multiple myeloma. The design was a randomization of 1:1 in 307 patients. The patients needed to have received 2 or more lines of therapy, including lenalidomide and a PI; however, no pomalidomide because pomalidomide was part of the study. Isatuximab was weekly for cycle 1, days 1, 8, 15, and 22, and every other week in cycle 2 in combination with Pd, which was the standard Pd regimen. [Treatment continued] until the patient progressed or there was evidence of [unacceptable] toxicity.4
The primary end point was—as in many of these trials—PFS by independent review committee; there were also secondary end points, including overall response rate and overall survival [OS]. The median age was 67 years; 40% were between 65 and 74 years old, 20% were older than 75 years. Eleven percent had a history of lung complications, 20% had high cytogenetic risk, and the number of prior lines of therapy at baseline was 3. Ninety- three percent of patients were lenalidomide refractory, 76% were refractory to a PI, and 73% were double refractory.
The study achieved the primary end point of PFS, which was 11.5 months for the isatuximab-Pd versus 6.5 months for Pd, and this was statistically significant [HR, 0.596; 95% CI, 0.44-0.81; P =.001].
This benefit was observed in all categories, especially in patients who were 75 years or older [HR, 0.48; 95% CI, 0.24- 0.95]. [These included] even patients who had some renal insufficiency, an estimated baseline GFR [glomerular filtration rate] less than 60 mL/min [HR, 0.50; 95% CI, 0.30-0.85], patients who had high-risk cytogenetics [HR, 0.66; 95% CI, 0.33-1.28], and patients who were refractory to lenalidomide [HR, 0.59; 95% CI, 0.43-0.82]. The subgroup data showed patients did better with the addition of isatuximab to Pd.
In regard to survival, the follow-up was short; however, it was meaningful for OS. [At 12 months], there was a trend of 72% [OS rate] for isatuximab-PD versus 64% for Pd [HR, 0.687; 95% CI, 0.461-1.023]. The lines separated at 12 months.4
The response rate was higher for the combination of isatuximab-Pd compared with Pd, and the VGPR was 27% versus 7%, respectively. MRD [minimal residual disease] also favored the combination of isatuximab-PD, and even though [the negativity rate] was 5%, this was in the population that was refractory. In the control arm, MRD negativity was 0%; no patient became MRD negative.
There were infusion reactions, which is something we see frequently with any protein. We have seen that with rituximab [Rituxan], daratumumab, or any ATG [antithymocyte globulin] that we infuse; isatuximab-Pd was no exception. [The rate of grade ≥3 AEs in the isatuximab-PD arm] was about 86% [versus 71% in the Pd arm]. The discontinuation rate was only 7.9% in the isatuximab-Pd group. The addition of isatuximab significantly improved the effectiveness of Pd, with an acceptable toxicity profile. There were some cases of neutropenia, which was unexpected [grade ≥3, 85% for isatuximab-Pd vs 70% for Pd].
How would you compare daratumumab and isatuximab?
There are differences between daratumumab and isatuximab [regarding] mechanism of action and some toxicities that isatuximab has that daratumumab doesn’t. However, these have not been proved in the clinical setting...and there’s no head-to-head comparison of these 2 monoclonal antibodies.
[With isatuximab,] the infusion rate seems to be better tolerated and a little bit faster because of the way that you adopt the practical consideration in these 2 monoclonal antibodies or you can play with the concentration. You can concentrate the drug more and/or accelerate the infusion time. With daratumumab, the total time of infusion can go from 7 hours to 4 hours to 3.5 hours, and you can go as low as 2 hours with isatuximab. Daratumumab now has been approved for subcutaneous administration, but in our hospital, there are no oncologists who have used daratumumab subcutaneously.
If a patient progresses on daratumumab, would you put them on isatuximab, or vice versa?
If it’s an immediate failure, no, I will probably not use isatuximab in the absence of any new data. These are new drugs that have some mechanism of actions that might be deferred slightly, and we don’t know if they’re going to translate. And when I say we, I’m talking about me and people who study myeloma. I’m not so sure if the company knows or doesn’t know. I’m not aware of any clinical data showing that those differences can make a clinical impact. I will probably not pursue it. It’s not like going with pomalidomide after lenalidomide. There are some people who still might respond to the second-line or third-line immunomodulatory drug. Here, I’m not aware that data are out there.
Which of the 2 monoclonal antibodies would be your first choice for anti-CD38?
Lately, I’ve been using isatuximab more often. Again, we don’t yet use subcutaneous daratumumab. Perhaps because of the infusion reaction that I was seeing before with daratumumab, I was intrigued about what would have been the case [for it] or what would have been the case for isatuximab. I’ve seen transfusion reactions with isatuximab. That being said, none of them required hospitalization or intervention with daratumumab....I have seen a couple, not often, but yes, a couple of infusion reactions have required observation; in that case, there was an intensive care unit admission and that patient survived. That pushed me to explore isatuximab, and so far, I’ve not had any major issues.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 4.2021. December 10, 2020. Accessed January 12, 2021. https://bit.ly/3sLly6g
2. Palumbo A, Chanan-Khan A, Weisel K, et al; CASTOR Investigators. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(8):754- 766. doi:10.1056/NEJMoa1606038
3. Dimopoulos MA, Oriol A, Nahi H, et al; POLLUX Investigators. Daratumumab, lenalid- omide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(14):1319- 1331. doi:10.1056/NEJMoa1607751
4. Attal M, Richardson PG, Rajkumar SV, et al; ICARIA-MM Study Group. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexa- methasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): a randomised, multicentre, open-label, phase 3 study. Lancet. 2019;394(10214):2096- 2107. doi:10.1016/S0140-6736(19)32556-5
5. Stewart AK, Rajkumar SV, Dimopoulous MA, et al; ASPIRE Investigators. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372(2):142-152. doi:10.1056/NEJMoa1411321








