Gergis Explains the Differences Between Acute and Chronic GVHD
Usama Gergis, MD, MBA, reviewed that difference in acute and chronic graft-versus-host disease and the treatment available for each
Usama Gergis, MD, MBA

Usama Gergis, MD, MBA Professor of Oncology Director, Bone Marrow Transplant and Immune Cellular Therapy Sidney Kimmel Cancer Center Thomas Jefferson University Hospital Philadelphia, PA, reviewed that difference in acute and chronic graft-versus-host disease (GVHD) and the treatment available for each.
Targeted OncologyTM: How would you treat a patient with GvHD in the second line?
GERGIS: If you [have a patient with] second-line acute GVHD, your answer should be ruxolitinib [Jakafi] because it’s the only drug that has been tried in phase 3 trials. If you get a [case of] chronic GVHD, your answer should be ibrutinib [Imbruvica].
What is the efficacy of peripheral blood stem cells (PBSC) versus bone marrow from unrelated donors in patients with acute and chronic GvHD?
[Results from] a phase 3 study of bone marrow versus stem cells for unrelated donors [showed] the acute GVHD population [cumulative incidence] was the same between both.1 For the chronic population, the bone marrow did better [PBSC 53% vs bone marrow 41%; P = .01]. This was published almost 8 years ago, [and it] was reported almost 10 years ago, but we still use stem cells.
This has not changed practices, and the reasons are, number 1, there was more primary graft failure on the bone marrow than the PBSC, and number 2, it’s pretty involved to do bone marrow harvest, although I have done it for 15 years, at least a few every month.
The benefit of bone marrow versus PBSC—and this benefit was only studied in unrelated donors, not in matched related donors—was seen across all organs affected with chronic GVHD except lungs, [gut, and serosa].2 So, there was no real benefit in the lungs.
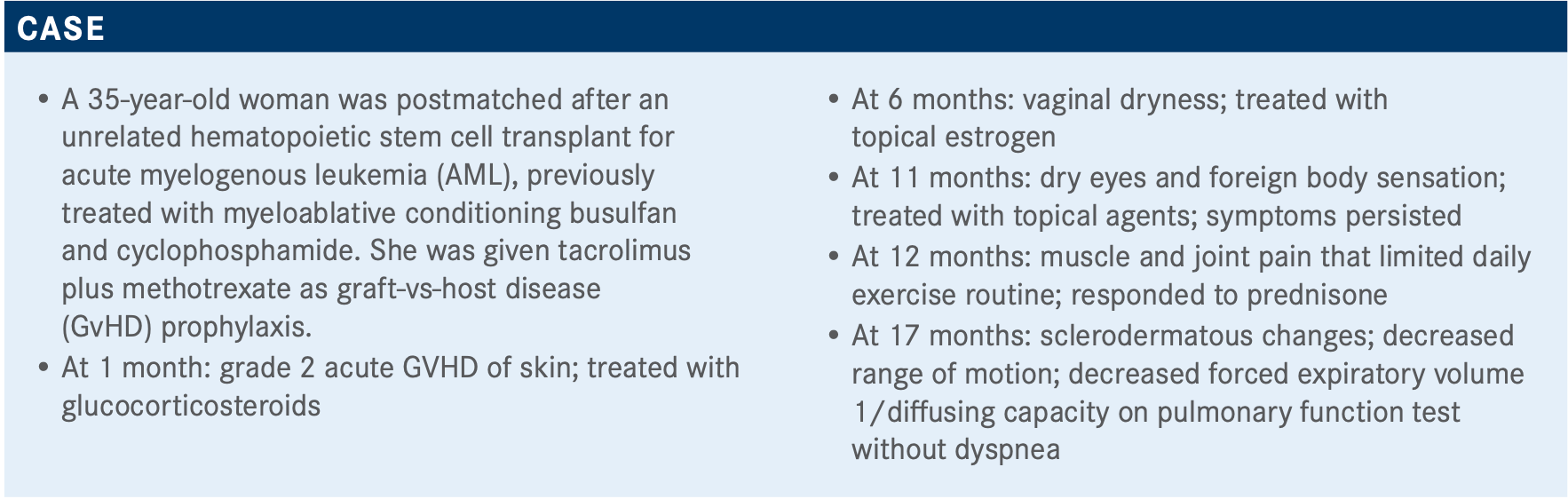
Can you explain the difference between acute and chronic GvHD?
Chronic GVHD is more complicated and involved than acute GVHD. In acute, you have the skin, gastrointestinal organs, and the liver [that may be affected]. That’s it. In chronic, all the patient’s other organs can be affected. The patient’s weight can be affected. [Chronic GVHD is] more debilitating over a long time and [can] go unrecognized for a while. [If a patient is] experiencing acute GVHD, you see them twice a week, whereas if the patient has chronic GVHD, you probably see them once a month. So you can see a very stark change in your patients within that month if they lose 10% of their body weight and they already lost a lot of weight in the period right after [transplantation], so that can be obvious to you.
[In my institution], we have the GVHD clinic where we [grade the patient based on] studying the degree of fibrosis, how many organs are affected, the patient’s range of motion, and the degrees in range of motion. We do frequent pulmonary function tests and various [other] testing. By looking at all the affected organs, you reach a grade, and that can be mild, moderate, or severe [chronic GVHD].
How do you treat moderate-to-severe chronic GVHD at initial presentation and in the second line?
First-line treatment for chronic GVHD are steroids. For second line, there are many agents [to consider]. I’ve tried most of them. I like photopheresis because it’s not pharmacological, but it’s pretty involved. Your patient will need a permanent catheter, and they will need to come to the transplant center twice a week, and you see a response after a long time. It takes an average of 50 photopheresis sessions for a response. But the beauty of photopheresis [is that] you could try it with other agents, so it’s not mutually exclusive. You could use it with ruxolitinib, ibrutinib, or any other agents.
The answer will be ibrutinib [for chronic GVHD], and that’s based on the [results of a] phase 2 clinical trial that treated 42 patients with steroid-refractory chronic GVHD, and the efficacy was 69% [best overall response rate], and 31% complete response rate.3
What do you think of these poll results?

Everybody agrees on giving ibrutinib. When I gave this talk a couple months ago, lenalidomide [Revlimid] was not included in the poll. I added it because [recently], a nice study in Blood came out from the National Institutes of Health where they tried lenalidomide at a small dose, 2 mg, in steroid-refractory chronic GVHD. It’s a large trial; I think it’s about 100 patients. They’ve seen responses that are comparable with ibrutinib....I treated a patient for multiple myeloma; he received a transplant for multiple myeloma, and now, 6 months later, he has chronic GVHD and some clonal plasma cells. So for him, I was comforted to know the results of the lenalidomide trial.
How does ruxolitinib play a role in this setting?
Ruxolitinib was reported in the REACH3 trial [NCT03112603] with very good responses in chronic GVHD.4 I think it probably will get approved for that indication. Looking at this study about 2 years ago, nothing was studied well in this indication, and ibrutinib was approved.
REACH3 was a large trial, almost 300 patients, and everybody was randomized to ruxolitinib 10 mg twice a day versus best available treatment. They looked at everybody about 6 months later for response.
What should physicians keep in mind when treating?
Chronic GvHD is pretty involved. Your patients will need a multidisciplinary approach. You need to pay attention to their bones. In the first 100 days post transplant, the average bone aging is 17 years.
So although we’re trying to treat acute GVHD, viruses, and prevent relapses, [by putting] your patients on some steroids, you are aging your patients’ bones by 17 years only in the first 100 days. No matter what you do, give your patients vitamin D, calcium, and Fosamax [alendronate sodium].
REFERENCES:
1. Anasetti C, Logan BR, Lee SJ, et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367(16):1487-1496. doi:10.1056/NEJMoa1203517
2. Flowers ME, Martin PJ. How we treat chronic graft-versus-host disease. Blood. 2015;125(4):606-615. doi:10.1182/blood-2014-08-551994
3. Waller EK, Miklos D, Cutler C, et al. Ibrutinib for chronic graft-versus-host disease after failure of prior therapy: 1-year update of a phase 1b/2 study. Biol Blood Marrow Transplant. 2019;25(10):2002-2007. doi:10.1016/j.bbmt.2019.06.023
4. Zeiser R, Polverelli N, Ram R, et al. Ruxolitinib (RUX) vs best available therapy (BAT) in patients with steroid-refractory/steroid-dependent chronic graft-vs-host disease (cGVHD): primary findings from the phase 3, randomized REACH3 study. Blood. 2020;136(suppl 1):22-24. doi:10.1182/blood-2020-137694

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More











