Data Show That PD-L1 Status Affects the Efficacy of Pembrolizumab in Non–Small Cell Lung Cancer
Ravi Salgia, MD, PhD, discussed the case of a 59-year-old patient with non–small cell lung cancer during a virtual Targeted Oncology Case-Based Roundtable event.
Ravi Salgia, MD, PhD, the Arthur & Rosalie Kaplan chair in Medical Oncology at City of Hope discussed the case of a 59-year-old patient with non–small cell lung cancer during a virtual Targeted Oncology Case-Based Roundtable event.
Targeted OncologyTM: What is the significance of pembrolizumab (Keytruda) for patients like this one with non–small cell lung cancer (NSCLC) without a molecular driver alteration?
SALGIA: [In the KEYNOTE-189 trial (NCT02578680)], Leena Gandhi, MD, PhD, when she was over at the Dana-Farber Cancer Institute, looked at overall survival [OS] and progression-free survival [in NSCLC] with platinum therapy, pemetrexed [Alimta], and pembrolizumab and compared it with placebo in combination with chemotherapy.1 That was further updated by Shirish Gadgeel, MD, MBBS, in the Journal of Clinical Oncology in 2020, and the results were quite impressive.2 The median OS was 22.0 months [with the pembrolizumab combination] versus 10.7 months [with the placebo combination (HR, 0.56; 95% CI, 0.45-0.70)]. This has revolutionized our practice. In patients whose tumors have higher PD-L1 expression, the median survival was much better [not reached vs 10.1 months with the placebo; HR, 0.59; 95% CI, 0.39-0.88].2
If PD-L1 expression is greater than 50%, is it better to use a single-agent immune checkpoint inhibitor or a combination?
There’s a certain algorithm being developed. In our clinical practice, and what more and more people are saying is, if the patient has really bulky disease and really symptomatic disease, combine [an immune checkpoint inhibitor] with chemotherapy. If you think you have time to wait for the immunotherapy to work its magic, so to speak, and you can do this with, let’s say, an every-3-week or an every-6-week regimen, then do it that way. I use the patient’s performance status and the tumor volume as my gauge.
The best thing is to use your clinical judgment. [Oncologists] have such great knowledge in terms of how patients will do. As soon as they see that patient in the clinic, they know [whether to use a] triplet therapy or single agent. I always know.
Every once in a while, I know that a patient needs a triplet therapy, but they may not be able to tolerate the carboplatin because they are much older. I start with the pemetrexed and the pembrolizumab and then after 2 cycles I add the carboplatin back in.
I think all of those things are allowed. This is not fixing a car engine, as an example. It’s really, truly medicine and there’s an art to the medicine. No question about that.
The [National Comprehensive Cancer Network (NCCN)] recommendations suggest: If it’s an older patient with poor performance status and they can tolerate only 1 therapy, you can consider that.3 The quadruplet regimen is a bit tougher to tolerate if their performance status is high.
What is the relationship between pembrolizumab and PD-L1 status?
The KEYNOTE-042 study [NCT02220894] compared pembrolizumab with carboplatin/paclitaxel or carboplatin/ pemetrexed.4,5 In this case PD-L1 greater than or equal to 1% was an eligibility criterion. [In patients where PD-L1 was] greater than 50%, you see a nice separation in the OS [Kaplan-Meier curves]. The median OS goes from 20 months [for PD-L1 ≥50] to 17.7 months [for PD-L1 ≥20%] to 16.7 months [for PD-L1 ≥1%], for just pembrolizumab alone.4 This was presented by Tony Mok, MD, in Lancet.5 With a PD-L1 of 1% to 49%, there was up to 13.4 months’ median OS [with pembrolizumab] as compared with 12.1 months [with chemotherapy (HR, 0.92; 95% CI, 0.77-1.11)].
What about quadruplet therapy with atezolizumab (Tecentriq), carboplatin, paclitaxel, and bevacizumab (Avastin)?
So, then we come to [IMpower150 (NCT02366143)], which was presented by Mark Socinski, MD, and published in the New England Journal of Medicine.6,7 This was a pretty intense study: 1:1:1 randomization of atezolizumab/carboplatin/paclitaxel versus atezolizumab/carboplatin/ paclitaxel/bevacizumab versus carboplatin/paclitaxel/ bevacizumab, and then maintenance. In theintention-totreat [group, OS rate for] the quadruplet at 24 months was 43.4% as compared with 33.7% with the triplet [carboplatin/ paclitaxel/bevacizumab]; hazard ratio, 0.78 [95% CI, 0.64-0.96], and P value of .02.
What is the relevance of TMB in this disease setting?
[CheckMate-227; NCT02477826], by Matthew Hellmann, MD, and colleagues, was another important study because this one looked at a PD-L1–selected population but they also looked at the TMB.8-10 David Carbone, MD, PhD, at The Ohio State University, published in the New England Journal of Medicine several years ago that once patients get nivolumab [Opdivo], you can look at TMB as a molecular marker as well and that patients with high TMB tend to respond better.11
Would nivolumab/ipilimumab (Yervoy) be appropriate in a case like this?
[In CheckMate 227, with] nivolumab/ipilimumab versus chemotherapy, there was separation of the [OS] curves.8-10 One thing we should keep in mind: When nivolumab/ipilimumab got approved for small cell lung cancer,12 it was a different way of giving it, as compared with that for NSCLC. When I give the nivolumab/ipilimumab regimen, patients with small cell lung cancer do poorly. But then this regimen itself is relatively well tolerated [in NSCLC]. Suresh Ramalingam, MD—the senior author on this paper with Hellmann—showed that nivolumab/ipilimumab is a reasonable regimen as well to use for [both] squamous and nonsquamous histologies.9
Does it matter which antibody test you use to measure PD-L1 expression?
People can get confused about PD-L1 expression. The PD-L1 expression is done by 28-8 antibody, whereas the pembrolizumab is [done with] the 22C3 antibody.
[Oncologists should] talk to their pathologist as well. Sometimes, also, you have to educate the pathologist and colleagues who are doing the biopsies. But it is important to do the proper molecular biomarker.
What adverse effects (AEs) would you watch for in this patient?
With anti–CTLA-4 therapy and immune checkpoint inhibition, expect AEs, of course. One has to manage these AEs. It can be anything: hypophysitis, thyroiditis, pneumonitis, nephritis, hepatitis, or colitis. We’ve even seen blood dyscrasias or blood disorders: immune thrombocytopenia, neutropenia. We’ve even seen hypereosinophilia as a reaction to immunotherapy. So all of those you have to keep in mind. Steroids are our friends when it comes to this.
What is the importance of EGFR and ALK alterationswith nivolumab?
[CheckMate 9LA (NCT03215706)] compared nivolumab/ipilimumab with chemotherapy.13 More and more as we go forward—these are all in TV commercials, too. You can get Keytruda or you can get Opdivo—[in the] TV commercials, they always say at the very end, “EGFR and ALK mutations and translocations are not allowed.”
You have to keep that in mind. The IMpower150 study did allow EGFR and ALK and they did see responses,6,7 but if you look at the Physicians’ Desk Reference for the approval sheet for the quadruplet regimen—that’s the carboplatin/paclitaxel/bevacizumab/atezolizumab— it doesn’t say that approval for EGFR now. I think the company didn’t want that in there. But more information to come in the future, I’m sure.
[In CheckMate 9LA, the OS] curves separate out very nicely.13 This was by Martin Reck, MD, and presented at the American Society of Clinical Oncology [Annual Meeting] for nivolumab/ipilimumab plus chemotherapy versus chemotherapy. Response rate was 38% versus 25% [odds ratio, 1.9; 95% CI, 1.4-2.6]; median OS, 15.6 months versus 10.9 months [HR, 0.66; 95% CI, 0.55-0.80]. PD-L1 status made a difference: the higher, the better.
Are physicians adequately educated about toxicities that occur with immunotherapy?
Safety, AEs—we talked a lot about that. Any kind of “-itis” that can occur, we’ve seen it and one has to manage it. Patients go to the emergency room. We have to treat those patients as well, so we have to do a lot of in-service for our emergency room physicians because they’re not familiar with how to take care of immune toxicities. They’re getting better, depending on the institution, but still, a lot of teaching has to be done. Even the hospitalists that take care of our inpatients have to be taught a lot about the management of these toxicities.
How do payers factor into treatment decisions?
Nivolumab/ipilimumab has been approved for the first-line treatment of [patients with] metastatic NSCLC.12 Atezolizumab, in patients with high PD-L1 expression, has just gotten approved as well in May.14 So it’s really a dealer’s choice, but I always say it’s also a choice base on the payers. What deals do you have and with which insurance companies?
The FDA also approved the test, but it’s not the 22C3. It’s not the 28-8 that’s for nivolumab; it’s the SP142. That’s the companion diagnostics. So your pathologists have to be savvy as to how they report this.
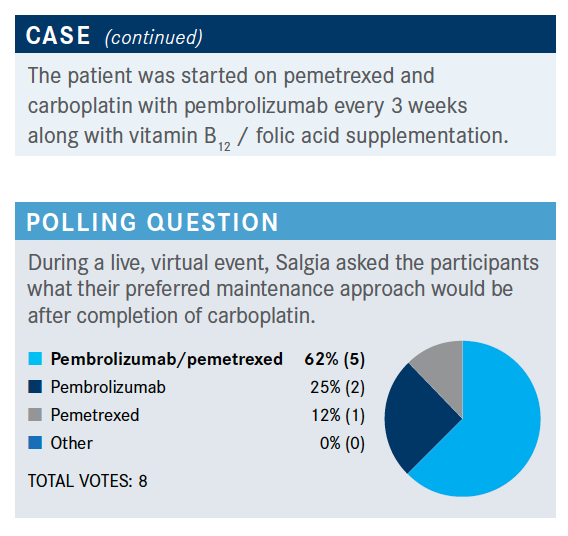
How do you choose between these maintenance options?
It really depends on how important and what the toxicity profile is for your patient. At the same time, sometimes you do the doublet, the pemetrexed/pembrolizumab, and then you might have to drop one or the other depending on the toxicity that develops.
What would you choose as a second-line treatment for this patient?
The patient received docetaxel and ramucirumab [as second-line therapy based on] the REVEL study [NCT01168973], published in the Lancet by Edward Garon, MD, at the University of California, Los Angeles, which compared ramucirumab [Cyramza]/docetaxel [Taxotere] to docetaxel.15,16 Median OS was 10.5 months [with ramucirumab plus docetaxel] versus 9.1 months [with docetaxel (stratified HR, 0.86; 95% CI, 0.75-0.98; P = .023)]. So it is important.
This is one of the only regimens that’s available to us at this moment in time after immunotherapy. I think right now it’s a very difficult question to answer: Are there other immunotherapy [options]? Could one do CTLA-4 in combination with other PD-1 or PD-L1 inhibition if the patient’s disease progresses on the first immune checkpoint inhibition? Could you combine it with LAG-3, or could you do other potential therapeutics? To be determined. We are looking forward to that as we go into the next year.
References:
1. Gandhi L, Rodr.guez-Abreu D, Gadgeel S, et al; KEYNOTE-189 Investigators. Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med. 2018;378(22):2078-2092. doi:10.1056/NEJMoa1801005
2. Gadgeel S, Rodr.guez-Abreu D, Speranza G, et al. Updated analysis fromKEYNOTE-189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non–small-cell lung cancer. J Clin Oncol. 2020;38(14):1505-1517. doi:10.1200/JCO.19.03136
3. NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer,version 6. June 15, 2020. Accessed March 15, 2021. https://bit.ly/31aF6nS
4. Lopes G, Wu YL, Kudaba I, et al. Pembrolizumab (pembro) versus platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1%: open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 2018;36(suppl 18). doi:10.1200/JCO.2018.36.18_suppl.LBA4
5. Mok TSK, Wu YL, Kudaba I, et al; KEYNOTE-042 Investigators. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819-1830. doi:10.1016/S0140-6736(18)32409-7
6. Socinski MA, Jotte R, Cappuzzo F, et al. Overall survival (OS) analysis of IMpower150, a randomized Ph 3 study of atezolizumab (atezo) + chemotherapy (chemo) Å} bevacizumab (bev) vs chemo + bev in 1L nonsquamous (NSQ) NSCLC. J Clin Oncol. 2018;36(suppl 15):9002. doi:10.1200/JCO.2018.36.15_suppl.9002
7. Socinski MA, Jotte RM, Cappuzzo F, et al; IMpower150 Study Group. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa171694
8. Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093-2104. doi:10.1056/NEJMoa1801946
9. Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non–small-cell lung cancer. N Engl J Med. 2019;381(21):2020-2031. doi:10.1056/NEJMoa1910231
10. Ramalingam SS, Ciuleanu TE, Pluzanski A, et al. Nivolumab + ipilimumab versus platinum-doublet chemotherapy as first-line treatment for advanced nonsmall cell lung cancer: three-year update from CheckMate 227 part 1. J Clin Oncol. 2020;38(suppl 15):9500. doi:10.1200/JCO.2020.38.15_suppl.9500
11. Carbone DP, Reck M, Paz-Ares L, et al; CheckMate 026 Investigators. Firstlinenivolumab in stage IV or recurrent non–small-cell lung cancer. N Engl J Med. 2017;376(25):2415-2426. doi:10.1056/NEJMoa1613493
12. FDA approves nivolumab plus ipilimumab and chemotherapy for first-line treatmentof metastatic NSCLC. FDA. Updated May 27, 2020. Accessed December 21, 2020. https://bit.ly/35tnarl
13. Reck M, Ciuleanu TE, Cobo Dols M, et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. J Clin Oncol. 2020;38(suppl 15):9501. doi:10.1200/JCO.2020.38.15_suppl.9501
14. FDA approves atezolizumab for first-line treatment of metastatic NSCLC withhigh PD-L1 expression. FDA. May 18, 2020. Accessed March 15, 2021. https://bit.ly/2HNJx1U
15. Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384(9944):665-673. doi:10.1016/S0140-6736(14)60845-X
16. Reck M, Paz-Ares L, Bidoli P, et al. Outcomes in patients with aggressive or refractory disease from REVEL: a randomized phase III study of docetaxel with ramucirumab or placebo for second-line treatment of stage IV nonsmall- cell lung cancer. Lung Cancer. 2017;112:181-187. doi:10.1016/j.lungcan.2017.07.03815.
