Roundtable Discussion: Challenges in Adjuvant Treatment for Patients With NSCLC
During a Targeted Oncology Case-Based Roundtable event, Ticiana Leal, MD, discussed the case of a patient with non–small cell lung cancer with a group of peers.
Ticiana Leal, MD
During a Targeted Oncology Case-Based Roundtable event, Ticiana Leal, MD, assistant professor of Medicine, University of Wisconsin School of Medicine and Public Health, and director, Thoracic Oncology Program at the University of Wisconsin Carbone Cancer Center discussed the case of a patient with non–small cell lung cancer with a group of peers.
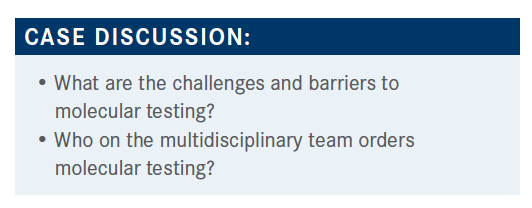
MAGDALENA FLEJSIEROWICZ, MD: In our system, [testing] is done automatically on adenocarcinomas. So the surgeons are the ones who order those tests, and then, if the patients get to see the medical oncologist very early, we are the ones sending it or ordering it. Most of the time, it’s done by whoever is doing the surgery.
GEETIKA SRIVASTAVA, MD: At our institution, it will come to the tumor board, and then typically the medical oncologist makes that recommendation saying that we will recommend molecular testing with adjuvant approval of treatment. It’s typically the medical oncologist who orders next-generation sequencing, and at the University of Colorado they have their own in-house testing, which is pretty robust and covers the whole panel.
FRANCIS CUEVAS, MD: So it’s not routinely ordered. For early-stage patients, the medical oncologist would see the patient first for the discussion of adjuvant therapy. Then we order just the EGFR test because right now, it’s the only [mutation] that’s actionable in early-stage disease. So it’s the medical oncologist, and for adjuvant setting, it’s just EGFR testing.
TICIANA LEAL, MD: For those that are not routinely testing, can you give us your perspective on how that has gone, why you don’t routinely test, and what the challenges have been?
BIRENDRA KUMAR, MD: I was not routinely testing but have changed now. I’m trying to do more and more because we have an approval for a drug....Also, in our place, one surgeon [may] order it and the other doesn’t order it. I think [the surgeon] leaves it up to the medical oncologist to decide.
KURT DEMEL, MD: At our institutions, it is solely the medical oncologist’s rule to coordinate medical testing. I agree with Dr Kumar and Dr Cuevas regarding actionable molecular markers in the early-stage process. I think we’re all learning about the ADAURA trial [NCT02511106], and EGFR would be the single actionable mutation that we’d order at this point in time for patients with early-stage disease.
LEAL: [If] surgeons are the ones ordering it at your institution, how did that get set up? Because I’m hearing that, for the majority of other participants, it is really the role of the medical oncologist. So how did you get the surgeons to test patients? I think that’s great.
FLEJSIEROWICZ: I said that it’s part of the tumor board, the recommendations, most of the time. So then there is this person who works with the surgeon—[usually] nurses or nurse navigators—and they’ll get the process going.
LEAL: So do most people, then, discuss all of these patients with early-stage lung cancers pre- or post resection at their tumor board?
FLEJSIEROWICZ: They do both; we do both: Pre- and post resection.
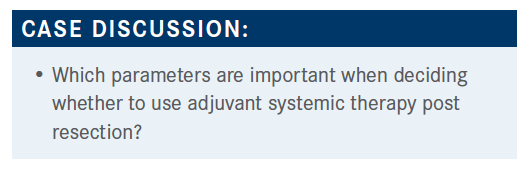
JACQUELINE MULLVAIN, MD: The size of the tumor and then the lymph node status are going to strongly push you in the direction of adjuvant chemotherapy. But I think for patients who have a borderline-size tumor, sometimes it’s high-grade histology or visceral pleural invasion. And then a lot of it comes down to age of the patient, overall health of the patient. Are they a cisplatin candidate, what’s the histology of the tumor, what drug are you using with the platinum doublet, and how are they going to tolerate that? So I think a lot of it has to do with the pathology characteristics here and then also the general fitness of the patient.
LEAL: How do you view adjuvant chemotherapy? Do you feel like that’s an important component of postoperative therapies for patients with the right clinical decision-making that was mentioned?
MULLVAIN: Yes, in a fit patient, especially somebody who has lymph node disease or a larger tumor, I think that adjuvant chemotherapy is important. In somebody who is a borderline cisplatin candidate or who has a lot of comorbidities, I try to be realistic about the benefit of adjuvant chemotherapy and the fact that the survival benefit overall is fairly small.
I think in a fit patient, yes, I would push them [and say], “You had curative intent surgery. We’re going to do everything we can to cure your lung cancer.” But in somebody who’s borderline or their criteria for chemotherapy are less clear, we sometimes discuss that: “Yes, there is an overall survival benefit of chemotherapy, but I want to be up front that toxicities can be fairly high and the survival benefit is fairly low.”
DEMEL: I would echo [that], and I think that size, lymph node status, and histology are very important as are medical comorbidities. I agree that with the data to date, I would try to proceed with a cisplatin doublet in the appropriate histology. I also think that quality-of-life concerns need to be taken into [account].
LEAL: Is this something that you have a discussion about, whether it’s curative or not [with patients]? What kind of approach do you have in the postoperative setting for your patients with lung cancer?
PRIYA KUMAR, MD: I think I would also discuss the overall prognosis and the fact that it’s poor in patients with resected lung cancer. Therefore, we ought to make an effort to treat micrometastases. It’s 4 cycles of treatment, and I would at least attempt a cycle in patients who are able to tolerate it, especially in patients with lymph node–positive disease.
LEAL: We now have a new therapy for patients with early-stage resected non–small cell lung cancer [NSCLC]. For patients with resected stage 1B and above NSCLC, chemotherapy is standard therapy according to National Comprehensive Cancer Network guidelines.1 Having a discussion about adjuvant chemotherapy, as many of you have already said, is definitely a standard approach that we use for high-risk patients. Now we have the addition of osimertinib [Tagrisso] for patients with resected NSCLC.
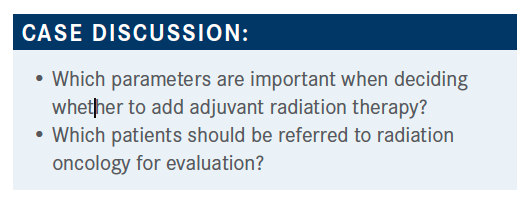
FLEJSIEROWICZ: We present every patient, like I said. They are part of the tumor board, and automatically, we involve them. I think that many times, not even [just] with lung but any other diseases, patients are asking me questions. They heard about radiation: One neighbor had it; why doesn’t she have it? So I tend to have their opinion and something in writing, or at least talk to the patient about why yes or why no because many times [they are] confused. I always tell them it’s complementary—it’s not\ like one is better than the others—so I tend to have them see radiation oncology regardless.
P. KUMAR: I think with recent data from the European Society for Medical Oncology meeting, radiation [for] N2 disease has become a little more complicated. It showed less benefit, but I still send them to radiation oncology to discuss the data..
LEAL: What are your thoughts about the ADAURA data?. Do you think they are practice changing? What are the strengths and weaknesses of the study, and how has that affected your discussion with your patient in the postoperative setting?
MULLVAIN: I found [these] data to be exciting, but I haven’t used [osimertinib in this setting] yet, mainly because most of the resected patients I see are stage IA, so it hasn’t come about. I am seeing a man who has resected N2 disease and his molecular studies are pending, so maybe he’ll be the person [I use it in]. However, I would say osimertinib is a drug that, in the metastatic setting, I’m really familiar with and I’ve had great results with.
My anxiety with this study is the same as when we started using chemoimmunotherapy in the first-line setting for metastatic disease; it’s just you always wonder what comes next. I think that’s what worries me about [these] data....What do you do in year 4 if somebody recurs?
SRIVASTAVA: I haven’t used it myself yet, just because I haven’t seen a patient since the approval who fits criteria. I think the FDA approval is for 3 years. That makes me wonder why 3 years to just delay the inevitable. So that’s my only [concern] in terms of wondering why 3 years. Because as previous data [showed], statistically it was sometimes not significant. Was it the length of time for which they got the disease? Are we just delaying recurrence that’s going to happen later?
At the same time, given with adjuvant chemotherapy, the benefit is small. Often with stage II [disease], you’re talking single-digit benefits. I think, for that reason, I do find it encouraging, and at least it’s something better to offer patients.
VISHAL RANA, MD: I’m very encouraged with the data. The degree of benefit is so startlingly better than all previous EGFR inhibitors. The curves were so wide apart; it gives a sense that there is probably some sort of eradication of micrometastatic disease. Survival benefit may not be as much, but I hope to see some survival benefit. This is a much more effective EGFR inhibitor than what we have previously been using, so the hope is that it is indeed eradicating some micrometastatic disease. To this point, the fact that there’s significant difference in central nervous system [CNS] relapse is also telling us that it is, indeed, eradicating some micrometastatic disease in the CNS as well. So, yes, I will use this, more so for patients with stage II and stage III disease. In patients with stage IB [disease], the benefit is not as stark, but for stage II and stage III, I’ll certainly be using it.
DEMEL: I find these results encouraging. I think the [next] question is: If the data [are] so encouraging, but not in the 60:40 split between chemotherapy and nonchemotherapy, then which patients can we drop the chemotherapy from?
LEAL: Yes, I think you bring up a good point because I think when you review the breakdown of who the 40% were that did not receive chemotherapy, they were more likely to be in the stage IB population. I don’t think it answers the question “Can we skip chemotherapy?” I don’t think the ADAURA trial answered that question.
In my mind, chemotherapy is still a standard adjuvant therapy that we know improves survival. I agree that it’s a modest benefit—we all know the toxicities that patients, unfortunately, sometimes go through with adjuvant chemotherapy—but it is the therapy that has been shown to improve OS [overall survival]. Looking at the ADAURA trial, I would still offer adjuvant chemotherapy to my patients as a standard approach, followed by adjuvant osimertinib, with the caveats and the discussions [that] there’s a CNS disease-free survival [DFS] benefit. Although the treatment is well tolerated, there are adverse effects, additional visits, additional appointments; we’re talking about longer-term treatment for a patient population that is trying to get back to the workforce.
I think Dr Mullvain also brought up an important point. When there is recurrence, what are the mechanisms of resistance? I think it will depend on when patients recur. Do they recur on therapy, or do they recur following therapy completion? And how long after [do they recur]? Those are data that we currently don’t have, but certainly this is something that we’re going to learn more about in the future, and that will be important to get better sense of.
LEAL: For those of you who say you want to wait for OS data, a lot of our patients with EGFR [mutations] are part of Facebook groups and patient advocacy groups. How will you have this discussion with a patient who does not want to wait for the OS benefit?
RABIH FAHED, MD: I will not wait for the OS. I think in all comers and different tumor subtypes, many regimens were adopted and are becoming standard based on DFS. My approach, at least for the eligible patient: I would consider osimertinib in the adjuvant setting. I may have a different threshold on discontinuing treatment for patients with stage IB [disease] if the quality of life is affected, but I would definitely [use it for patients with] stage II and stage IIIA [disease]. I think I would consider the appropriate dose reduction and try to keep the patient on treatment as long as possible.
LEAL: How would you discuss this with your patient?
RAO MUSHTAQ, MD: When I see my patient with an EGFR mutation to their tumor, I tell them about the ADAURA trial. I mention that we have 3 trials [that] have not shown DFS translating into OS. We are very much hopeful about osimertinib— the chances are there might be some OS benefit—but if there is a patient who has IIIA and is not a candidate for chemotherapy, I will definitely offer osimertinib.
My other concern is that osimertinib is the best drug available for EGFR mutation, [so] what if my patient progresses? What will be the next option? Will it be the same chemotherapies? So unless we have another option for a next-generation EGFR tyrosine kinase inhibitor, I will be a bit careful about just using osimertinib in all of my patients, unless I have OS data.
LEAL: Is anybody concerned with cost or toxicity, or [does anybody] have concerns about that in your own practice?
STEPHANIE TREXLER, PHARMD: Yes, I know that we have 1 patient on it, and she had no issues with insurance so far or toxicities that I know of. Since it’s FDA approved, hopefully there won’t be insurance issues. I would be interested to see the quality-of-life data from the trials, and I know they looked at that, but I don’t think it’s reported yet. So that’s something that I was looking for—since it’s a new therapy for the adjuvant setting—because if patients have a rash or diarrhea, even if it’s not grade 3, it could still affect their quality of life.
It [also] really depends on the patient’s insurance. So if they have Medicare, it could be quite expensive until they get through the doughnut hole, for example. However, if they have a state insurance, it might be free.
LEAL: Yes, the drug is definitely expensive and certainly not widely available in other countries. I do think cost is something that will be taken into consideration, especially in countries where osimertinib is not available, not even [just] in the metastatic settings.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 4.2021. Accessed March 25, 2021. https://bit.ly/3rlZVrb
2. Le Pechoux C, Pourel N, Barlesi F, et al. An international randomized trial, comparing post-operative conformal radiotherapy (PORT) to no PORT, in patients with completely resected non-small cell lung cancer (NSCLC) and mediastinal N2 involvement: primary end-point analysis of LungART (IFCT-0503, UK NCRI, SAKK) NCT00410683. Ann Oncol. 2020;31(suppl 4):S1178. doi:10.1016/j.annonc.2020.08.2280
3. Wu YL, Herbst RS, Mann H, Rukazenkov Y, Marotti M, Tsuboi M. ADAURA: phase III, double-blind, randomized study of osimertinib versus placebo in EGFR mutationpositive early-stage NSCLC after complete surgical resection. Clin Lung Cancer. 2018;19(4):e533-e536. doi:10.1016/j.cllc.2018.04.004

Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More