Brose Explores Treatments for a Patient With RET-Mutated Thyroid Cancer
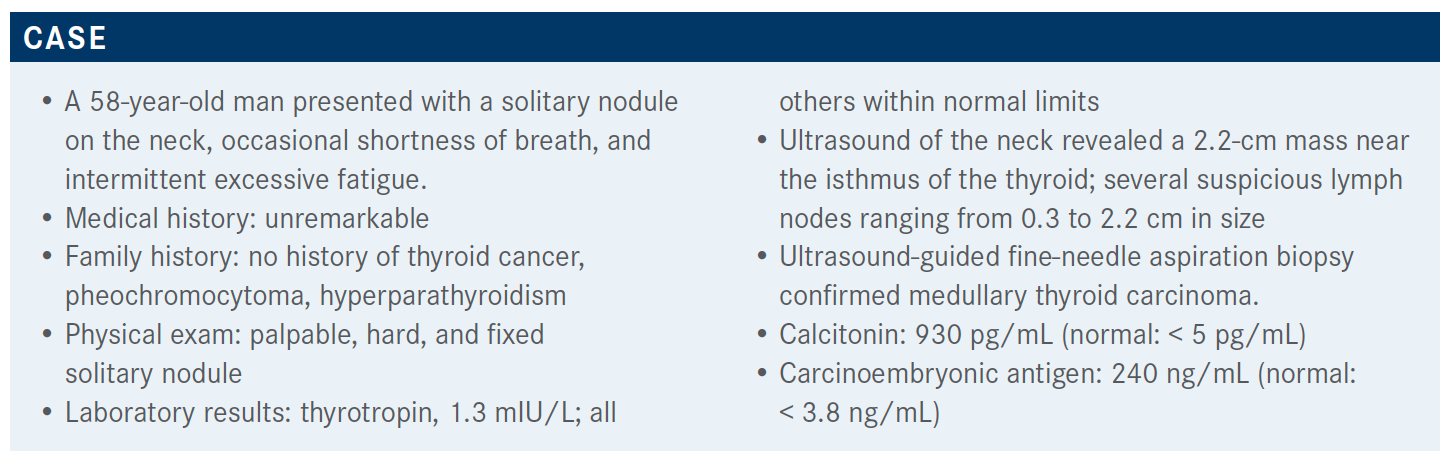
During a virtual Targeted Oncology Case-Based Roundtable event, Marcia S. Brose, MD, PhD, discussed the case of a 58-year-old patients with RET-mutated thyroid cancer.
Marcia S. Brose, MD, PhD

During a virtual Targeted Oncology Case-Based Roundtable event, Marcia S. Brose, MD, PhD, director, Center for Rare Cancers and Personalized Therapy and director, Thyroid Cancer Therapeutics Program at the Abramson Cancer Center of University of Pennsylvania, discussed the case of a 58-year-old patients with RET-mutated thyroid cancer.
Targeted OncologyTM: For a patient with medullary thyroid cancer (MTC), is there a situation where you would consider watching and waiting instead of therapy?
BROSE: If they have more than 1 liver metastasis and [the tumor is] over 1 cm, I usually don’t wait too long if they have a RET mutation because there is such a good option for them. I might wait a little bit longer if I’m talking about the other kinase inhibitors with more [toxicities].
I’m fine with watch and wait if you know what you’re waiting for. What that means is: when I have a patient and I don’t know them, or they’ve just received a diagnosis, I have no clue what their velocity is, and letting them go 6 months without a scan is a very long time, especially when they weren’t adequately staged upfront. The first thing I would do is get adequate staging up front, and if I didn’t know [already], I would probably get a first set of scans at 3 months so that if their disease is growing, I can intervene.
My concern is that for many patients, symptoms from their disease don’t always disappear. You can end up with [issues] like pleural effusion or cough, and even though the disease goes away, that persistent cough doesn’t. So I like to jump before we have symptoms.
I had a patient who has been on surveillance for 20 years; I [started seeing] her at 10 [years in]. But my point is that this patient has indolent MTC, but I have to prove it, and I [do that] by doing a couple of 3-month scans. As soon as I see [the tumor is not changing], maybe then I can use the calcium doubling time and say, “We haven’t bumped [up] and it’s been 6 months.” Then I’ll say, “OK, the next scan can be at 4 or 6 months,” and give them a bit more room. But I don’t trust [the disease], and I have to prove that the tumor is not going to misbehave before I would [watch and wait].
What testing do you order for patients with thyroid cancer?
Both papillary [thyroid cancer] and MTC have RET alterations. The difference is that papillary thyroid cancer acts [more] like lung cancer and tends to have translocations, whereas medullary disease has point mutations. That’s important because when you’re ordering genetic testing, you have to ensure that if your patient has papillary thyroid cancer, you’re getting a good gene fusion panel, whichever modality, wherever you’re sending it. Just check your list of identifiable abnormalities for whatever testing you’re ordering. Germline RET mutations happen in kids; it’s important that if you have a germline mutation, send the patient for genetic counseling so they can get the kids screened because you can save some lives by doing a good screening. So do not ignore that. But it is true that if you have a patient who is sick in front of you, you send the tissue first so that you get all the mutations, not just half of them.
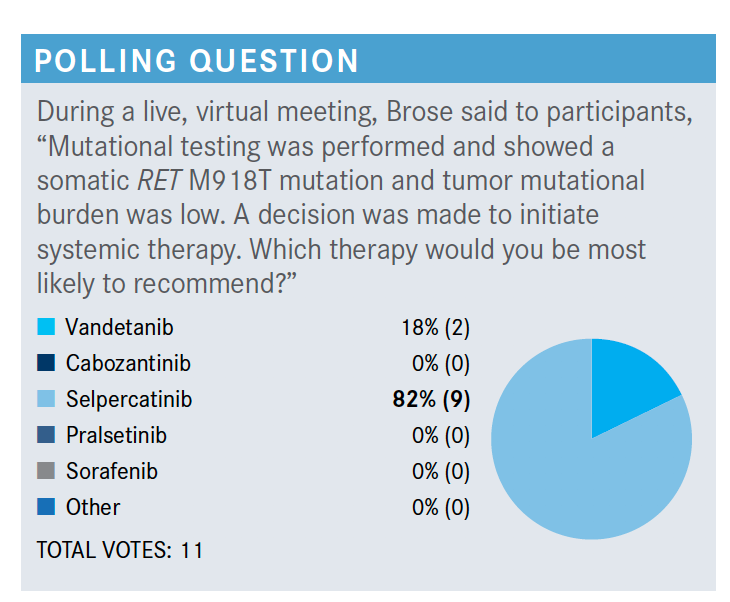
Do you agree with these poll results?
These [poll results] bring up a couple of things I want to point out. There were overall survival [OS] data from the cabozantinib [Cabometyx] trial [EXAM; NCT00704730] that showed patients with a RET M918T mutation had extended OS with cabozantinib [RET M918T positive HR, 0.60; negative HR, 1.12].1 Now would I use that over selpercatinib [Retevmo] given the difference in the toxicity profiles? Not on your life.
Vandetanib [Caprelsa] and cabozantinib are the 2 multikinase inhibitors approved for MTC. Selpercatinib and pralsetinib [Gavreto], I’ll talk about [later with] the ARROW [NCT03037385] and the LIBRETTO-001 [NCT03157128] trials. Sorafenib [Nexavar] has some nice data in MTC, in the phase 2 setting, [but it is] definitely much lower down on my list.
Most people picked selpercatinib [in the poll]. Vandetanib and cabozantinib were both FDA approved, so you would never be wrong with that choice, and it would probably work quite well. We have 4 right answers here: vandetanib, cabozantinib, selpercatinib, and pralsetinib. I think any of these 4 are completely correct. When you know a drug well, you’re going to be managing the adverse effects [AEs] much more effectively, and sometimes that might be more important than which one has a slightly different profile.
What are the National Comprehensive Cancer Network guidelines recommendations in this setting?
Similar to lung cancer, [guidelines recommend] vandetanib and cabozantinib, which are both FDA approved.2 Phase 3 trials led to the FDA approvals. Selpercatinib [is in the guidelines]. Pralsetinib…[is] right under selpercatinib.
Can you discuss the study of vandetanib?
The ZETA trial [NCT00410761] had patients who were not actively progressing, so in the placebo arm, patients were [19.3] months out for their progression-free survival [(PFS), and PFS was not reached for the vandetanib arm].3 It’s hard to compare these data with anything else, but there was an improved hazard ratio of 0.46 with vandetanib, so it was approved based on that [95% CI, 0.31-0.69; P <.001]. The objective response rate [ORR] was 45%, so this was clearly an active agent.
It was active in patients that were RET-mutation positive. Vandetanib has good RET activity, and it was the entire reason that it was initially approved for MTC—that is part of the rationale that was used. Interestingly, this patient had the RET M918T mutation. I don’t [know] OS data in this setting as it wasn’t in this trial, but the RET M918T population did quite well with vandetanib.
[Any grade] of diarrhea was quite common [in 56% of patients given vandetanib]. Many times, this was doselimiting. Rash was common [in 45%]. [Much] like an EGFR [inhibitor], it has EGFR inhibitor activity, and [the AE of] acneiform rash can be quite bothersome, especially with teenagers who are on [this drug]. There was some nausea [33%], hypertension [32%], fatigue [24%], and headache [26%]. All of these were prevalent in the vandetanib arm. There was not an insignificant number of patients who had grade 3 diarrhea [11%] and hypertension [9%].
We have to watch the corrected QT [QTc interval] prolongation. There is a risk evaluation and mitigation strategy [REMS] program for risk remediation. In order to prescribe vandetanib, you have to go through a minitraining, and to order it, you have to provide your REMS number. That’s one of the obstacles for vandetanib. But once you’ve done it, it’s easy. You need to monitor electrolytes as well for the QTc prolongation. Dose decreases are fairly common when we use this in the clinic. Not many patients stay at 300 mg. Quite a few of them end up at 200 mg or 100 mg. But I have a patient 7 years out on vandetanib at 100 mg; she is doing great, doesn’t notice it, and her disease has stopped growing. So I’ll take 7 years, no problem.
What was the efficacy of the cabozantinib trial you mentioned previously?
The EXAM study also had a very good hazard ratio [for PFS] [HR, 0.28; 95% CI, 0.19-0.40].1 In the placebo arm, patients progressed at [4] months, but on the drug, median PFS was 11 months. These patients were actively progressing, so it was a much more aggressive cohort of patients. It was a very significant hazard ratio and was approved on that basis.
A lot of people, because the patients were more aggressive, chose [cabozantinib] initially. There was an analysis that showed the RET M918T-[positive population] did quite well in the OS data.
Again, there was diarrhea [all grade with cabozantinib, 70.1%] and weight decrease [57.9%]. Weight decrease and diarrhea can be combined; in other words, if you don’t
control the diarrhea, they lose more weight, so controlling the diarrhea can be extremely important. This is not the same as the diarrhea caused by calcitonin, which initially gets better when you treat patients. This is a diarrhea that comes on over several months and worsens, and patients lose a lot of weight and muscle mass.
Patients can also get hand-foot syndrome with this drug [52.8%], which is a little different from vandetanib. Decreased appetite [49.1%], nausea [46.7%], and fatigue [42.5%] are also things that we deal with commonly.
There were quite a few grade 3 toxicities for patients on cabozantinib. Knowing the toxicity profile and how to manage it is important. If you dose reduce, patients can be quite well treated, similarly to vandetanib. I think when you get used to these drugs, you can treat patients. I’ve had patients for years on cabozantinib. It just takes a bit of finesse and knowledge of what to look for and how to [counsel] patients to help themselves; make sure that they know how to take loperamide [Imodium] for diarrhea. Any of us who have [prescribed] various gastrointestinal oncology drugs know that we have to give people all the loperamide in the world if they need it. We can use that for these patients, and I teach people to give themselves loperamide, not [only] after the diarrhea, but prophylactically on standing doses of 2, 4, or 6 mg; whatever they need to prevent the diarrhea.
There were 22% of patients who discontinued because of an AE or serious AE. As with other tyrosine kinase inhibitors, these numbers tended to be higher in the initial trials and were lower as people got better at using these drugs and managing the AEs. But there was significant toxicity with both cabozantinib and vandetanib.
How did patients with MTC do when given selpercatinib? How was the trial for this designed?
LIBRETTO-001 had 2 arms; 1 was for RET fusion-positive papillary thyroid cancer, and then RET point mutation MTC.4 A large number, 306 patients, were in the MTC cohort.
They were broken down into people that were cabozantinib or vandetanib na.ve versus people who were not. There were RET M918T mutations in over half the patients [57% of 143 patients with MTC]. This is well known to be the most common mutation that we would see. A smaller number of patients were pretreated versus naive, and almost 90 patients were na.ve [versus 55 patients previously treated].
The age range was the same [15 to 84 years old]. The average systemic therapy in the patients who were pretreated…was 2 lines of therapy in many cases, either cabozantinib, vandetanib, or sometimes something else. This affected the ECOG status. There were quite a few more patients that had a performance status of 1 or 2. The investigators didn’t allow higher ECOG status, so they’re getting the healthier patients who were pretreated. Many patients who are pretreated will have ECOG status of 2 or greater [in the clinic].
There was an ORR in the previously treated group of 69%, but the na.ve group was 73%. That was for the patient with mutated MTC. These numbers are robust, and 73% compared well with both vandetanib and cabozantinib. It was a higher ORR than with either of those drugs.
Interestingly, duration of response was not reached or was 22 months [in the previously treated and treatment-naive groups, respectively]. These data are remarkable. We’re talking about 11 to 15 months or 16 to 18 months with vandetanib and cabozantinib, and now we’re out to 22 months [or more].
For PFS, 23.6 months [for treatment naive] or not reached [for previously treated] was the median. These patients were doing well for a really long time.
These patients tolerated the selpercatinib much better [compared with the other drugs I’ve discussed]. Even though it does have some hypertension [any grade, 30%] and liver function test abnormalities [increased aspartate aminotransferase level, 28%], it is nothing compared with what we’ve been fighting with [the use of] both vandetanib and cabozantinib.
What data from the ARROW trial are relevant in this space?
The ARROW trial had patients with RET-mutant papillary thyroid cancer or MTC, and they were either cabozantinibor vandetanib-naive or previously treated with cabozantinib or vandetanib.5
Age was pretty similar [in both arms for MTC], and ECOG performance status was almost all 0 or 1. These were healthy patients overall. A few patients with central nervous system metastases were treated. Prior [treatments with cabozantinib or vandetanib] were 0 to 2 [in the previously treated arm]. A couple of the patients who were cabozantinib or vandetanib na.ve were treated with immunotherapy… but it was not something that I think we’re regularly doing in thyroid cancer because there are no good data right now for immunotherapy in thyroid cancer, as it turns out.
In ARROW, for RET-mutant MTC after [treatment with] cabozantinib or vandetanib, the ORR was 60%, and in the patients who were naive, it was about 66%. There was a small number of complete responders [1.8% and 10%, respectively], as there was with selpercatinib, and median duration of response was not reached. But 79% and 84% of patients, at least at 6 months, were still responding.
There was some significant hypertension [any grade with pralsetinib, 40%]. It did seem like it was slightly more prevalent in ARROW with pralsetinib. But there were also some other grade 1 through 4 toxicities. Interestingly, some patients had problems with anemia and blood count, probably because of some interaction with the JAK pathway. There were a bit more frequent problems with gastrointestinal tract issues, some fatigue [38%], edema [29%], and people sometimes got fevers [22%], which I thought was curious because some patients just had [fever] in the beginning and then it went away. This was fairly well tolerated overall, just maybe not quite as low as what we saw with selpercatinib [in terms of AEs].
References:
1. Schlumberger M, Elisei R, Müller S, et al. Overall survival analysis of EXAM, a phase III trial of cabozantinib in patients with radiographically progressive medullary thyroid carcinoma. Ann Oncol. 2017;28(11):2813-2819. doi:10.1093/annonc/mdx479
2. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 3.2020. Accessed March 22, 2021. https://bit.ly/3uzMTZL
3. Wells SA Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134-141. doi:10.1200/JCO.2011.35.5040
4. Wirth LJ, Sherman E, Robinson B, et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med. 2020;383(9):825-835. doi:10.1056/NEJMoa2005651
5. Hu M, Subbiah V, Wirth LJ, et al. Results from the registrational phase I/II ARROW trial of pralsetinib (BLU-667) in patients (pts) with advanced RET mutationpositive medullary thyroid cancer (RET+ MTC). Ann Oncol. 2020;31(suppl 4):S1084.doi:10.1016/j.annonc.2020.08.1401

Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More