TIGIT Emerging as Target in Clinical Research Across Cancer Settings
Immune checkpoint inhibitors blocking CTLA-4 or PD-1/PD-L1 often provide durable antitumor benefits to certain patients who respond to them; however, the percentage of responders is low, around 15% to 25%.
Vijay K. Kuchroo, DVM, PhD
Immune checkpoint inhibitors blocking CTLA-4 or PD-1/PD-L1 often provide durable antitumor benefits to certain patients who respond to them; however, the percentage of responders is low, around 15% to 25%.1 Investigators are hopeful that agents targeting other checkpoint molecules, along with combinations of immunotherapies, can fill that gap to provide broader therapeutic coverage. One of the more promising targets of checkpoint inhibitors currently in early trials is TIGIT (T-cell immunoreceptor with immunoglobulin and ITIM domains). Agents targeting this coinhibitory receptor are the subject of early clinical and preclinical studies.2
Research on TIGIT has explored its roles in cancer, autoimmunity, and viral immunity.3 It is part of the poliovirus receptor (PVR)/nectin family. The pathway formed by TIGIT, CD96 (TACTILE), and costimulatory receptor CD226 (DNAM-1) is analogous to the CD28/CTLA-4 pathway.4 TIGIT, along with LAG-3 and TIM-3, form a group of coinhibitory receptors considered to be the next generation of clinical cancer targets following the notable yet limited success of CTLA-4 and PD-1 inhibitors.5 Though TIGIT, LAG-3, and TIM-3 are members of the same receptor class as CTLA-4 and PD-1, they exert unique functions, making them nonredundant.
TIGIT’s Mechanism of Action
“TIGIT inhibits T-cell activation,” Vijay K. Kuchroo, DVM, PhD, the Samuel L. Wasserstrom Professor of Neurology at Harvard Medical School and a senior scientist in neurology at Brigham and Women’s Hospital in Boston, Massachusetts, who has studied TIGIT for the past 15 years, said in an interview with Targeted Therapies in Oncology. “Our data suggest that [inhibiting] it cooperates well with PD-1 blockade.” Tumors use the inhibitory TIGIT pathway to avoid attack by the immune system. Thus, therapeutic agents that inhibit TIGIT signaling by, for example, disrupting ligand binding promote the ability of T cells to proliferate and attack tumor cells.
TIGIT is expressed on multiple immune cell types, with potentially different functions on each.3 Expression of TIGIT on regulatory T cells (Tregs), particularly tumor-infiltrating Tregs, enhances their immunosuppressive function, with indirect effects that include inhibition of proinflammatory cytokine production. TIGIT also directly suppresses the antitumor effector function of CD8 T cells. Immune activation of TIGIT-expressing cytotoxic T cells and natural killer (NK) cells is suppressed when TIGIT interacts with 1 of its ligands, CD155 (PVR) or CD112 (PVRL2; Nectin 2), which are widely expressed on tumor cells.
After making a knockout mouse model of TIGIT, Kuchroo found that the receptor also promotes the regulatory activity of B cells. “If you make a deletion of TIGIT only on B cells, these mice spontaneously develop multiorgan autoimmunity,” he said. Furthermore, eliminating TIGIT on Tregs severely compromises those cells’ function, he said.
Anti-TIGIT Agents in Clinical Trials
Tiragolumab Data presented at the American Association for Cancer Research (AACR) 2020 Virtual Annual Meeting by Johanna Bendell, MD, director of the Gastrointestinal Cancer Research Program at Sarah Cannon in Nashville, Tennessee, from the phase 1a/1b GO30103 trial (NCT02794571) demonstrated efficacy of atezolizumab (Tecentriq) plus the anti-TIGIT antibody tiragolumab in patients with PD-L1–positive non–small cell lung cancer (NSCLC).6
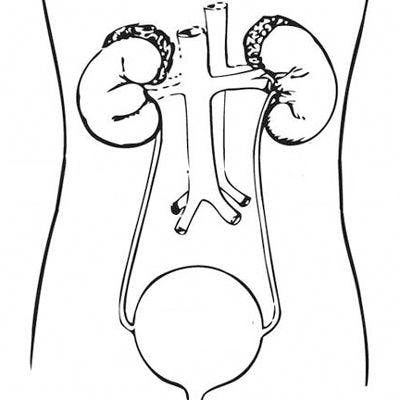
Patients treated as part of phase 1a were given single-agent tiragolumab; those treated in phase 1b received a combination of tiragolumab and atezolizumab. Patients with advanced solid tumors, including those in the colon, rectum, breast, lung, head and neck, and ovaries, were allowed onto the study.6 The CT302 investigators’ hypothesis was that blocking TIGIT along with PD-L1 would reinvigorate tumor- specific T effector cells, offering potentially better clinical responses (FIGURE).6
“Given the safety profile and clinical activity of anti–PD-1 and anti–PD-L1 [agents, investigators] are now using them as a therapeutic backbone to combine with other approaches, though the caveat is that it should not adversely [affect] health-related quality of life,” said invited discussant Michele Teng, PhD, associate professor and head of the Cancer Immunoregulation and Immunotherapy Laboratory at the QIMR Berghofer Medical Research Institute in Brisbane, Australia, following Bendell’s presentation of the trial results. The study enrolled 73 patients for whom standard treatment was unavailable or ineffective. Phase 1a included 24 patients, of whom 67% experienced treatment-related adverse effects (TRAEs). The phase 1b cohort included 49 patients, with 59% experiencing TRAEs; anemia, the most common, was reported in 31% of these patients. Investigators noted that the safety profile was acceptable across all dose levels in phase 1b. There were no objective responses in patients treated in phase 1a, with half of patients crossing over to the phase 1b group upon progression.
Three tumor responses were observed in patients treated in phase 1b. The responders, all of whom had PD-L1–positive tumors, included 2 patients with NSCLC, including 1 complete response (CR), and 1 patient with head and neck squamous cell carcinoma who experienced a partial response (PR).
Investigators created expansion cohorts of immunotherapy-naïve patients with PD-L1–positive tumors after noting that the combination of tiragolumab and atezolizumab produced preliminary antitumor activity in these patient subsets in phase 1b. The 14-patient metastatic NSCLC expansion cohort had a conf irmed objective response rate (ORR) of 46%, including 2 CRs and 4 PRs. The disease control rate (DCR) was 85%, and the safety profile was similar to that seen in the dose-escalation cohort. Patient enrollment in the expansion cohorts is ongoing.
Based on preliminary efficacy and safety observed in the phase 1a/1b trial described, the phase 2 CITYSCAPE (NCT03563716) trial was initiated to examine atezolizumab, alone or combined with tiragolumab, for firstline treatment of 135 patients with locally advanced or metastatic NSCLC with measurable disease. Participants in this randomized, double-blind trial had PD-L1–positive tumors with wild-type EGFR and ALK. Results were presented at the 2020 American Society of Clinical Oncology Virtual Scientific Program.7
Consistent with prior findings, CITYSCAPE results showed that tiragolumab plus atezolizumab was superior to atezolizumab monotherapy in terms of both ORR (31.3% vs 16.2%; odds ratio, 2.57; 95% CI, 1.076.14) and progression-free survival (PFS; 5.4 months vs 3.6 months; HR, 0.57; 95% CI, 0.37-0.90). The combination was well tolerated and associated with rates of grade 3 or higher all-cause AEs similar to those with atezolizumab alone (48% vs 44%).7 Investigators recently launched 2 phase 3 trials, SKYSCRAPER-01 (NCT04294810) in NSCLC and SKYSCRAPER-02 (NCT04256421) in extensive-stage small cell lung cancer, for further testing of the drug duo.8
Other Agents in Early-Phase Trials
An upcoming phase 1/2 study will focus on a combination of BMS-986207, nivolumab (Opdivo), and COM701 to study the blockade of the TIGIT, PD-1, and PVR immunoglobulin domain (CD112 receptor; CD112R) immune checkpoint pathways, respectively, in patients with advanced solid tumors, including those that may be refractory or nonresponsive to standard-of-care immune checkpoint inhibitors.9 BMS-986207 is an anti-TIGIT monoclonal antibody that binds to TIGIT expressed on several types of immune cells, including tumor-infiltrating T lymphocytes. This prevents TIGIT from interacting with its ligands, CD112 and CD155.1 It also enhances interactions of CD112 and CD155 with the costimulatory receptor CD226 expressed on immune cells like NK cells and CD8+ T cells. The resulting CD226-mediated signaling activates the immune system to execute a T-cell–mediated immune response against the tumor cells.10
COM701 is an investigational anti–poliovirus receptor–related immunoglobulin (PVRIG) antibody developed by Compugen. PVRIG and TIGIT are parallel inhibitory pathways counteracting stimulatory CD226 signaling. PRs have been achieved in previous trials of COM701, both as monotherapy and in combination with nivolumab, for patients with difficult-to-treat cancer types, including microsatellite-stable forms of platinum-resistant primary peritoneal cancer and colorectal cancer. These earlier clinical results support preclinical data showing that the PVRIG and PD-1 pathways are separate and that inhibiting both could clinically benefit patients. Compugen hypothesizes that the TIGIT pathway is also nonredundant with the PVRIG and PD-1 pathways; thus, inhibiting all 3 could expand the number of patients with tumors that respond to immunotherapy. The study’s investigational new drug application was approved by the FDA in June 2020. During a phase 1/2 trial dose-escalation trial of COM701 combined with fixed doses of BMS-986207 and nivolumab, investigators will aim to determine the agent’s safety, tolerability, and preliminary antitumor activity. Antitumor efficacy will be further assessed in expansion cohorts of patients with ovarian and endometrial cancer, and a biomarker-driven arm will assess tumor types with high CD112 expression.11
The MyCheckpoint (MMRC-089) open-label phase 1/2 clinical trial (NCT04150965) is examining the anti-TIGIT agent BMS-986207 in patients with multiple myeloma and started recruiting patients in June 2020. The estimated 104 participants with heavily pretreated relapsed/refractory disease will be randomized to 1 of 3 treatment arms. Patients in arm C will receive BMS-986207 monotherapy for the first 28-day cycle, then in combination with pomalidomide (Pomalyst) and dexamethasone from cycle 2 onward. The comparator arm A consists of the combination of elotuzumab (Empliciti), pomalidomide, and dexamethasone, with the experimental arm B examining the anti–LAG-3 agent BMS-986016 given in the same schedule as treatment on arm C.
In another phase 1/2 trial of BMS-986207 alone or combination with nivolumab (NCT02913313), patients with advanced solid tumors will be assessed for safety of the combination. This firstin-human trial of BMS-986207 began in 2016 with an estimated enrollment of 170 patients. The study is active but not currently recruiting patients, and no results are available.
In preclinical data presented at AACR 2020, the fully human anti-TIGIT antibody EOS884448 (EOS-448), dependent on Fcγ receptor engagement, showed strong in vitro competition with TIGIT natural ligands and prevented CD155-mediated inhibition of T cells from both healthy volunteers and patients with cancer. It also induced cytotoxicity preferentially against Tregs compared with CD4 and CD8 effector cells. In a mouse tumor model, single-agent EOS-448 strongly delayed tumor growth; combining it with an anti–PD-1 antibody produced an additional increase in antitumor activity, with CRs in 7 of 8 mice. EOS-448 demonstrated a safe profile in a primate toxicology study, and robust expression of several TIGIT pathway members in multiple tumor types led investigators to hypothesize that the agent may benefit a broad range of cancer indications. These findings, combined with additional translational medicine data, supported the initiation of a first-in-human study of EOS-448. In February 2020, the first of an estimated 30 patients with advanced cancers was enrolled in the dose- escalation portion of the phase 1/2a IO-002 trial (NCT04335253).12,13
Other trials are investigating the PD-1 inhibitor pembrolizumab (Keytruda) in combination with investigational anti-TIGIT agents. The phase 2 KEYNOTE-01A study (NCT04165070) is assessing the efficacy and safety of pembrolizumab in combination with the anti-TIGIT agent MK-7684, carboplatin, and either paclitaxel or pemetrexed in patients with treatment-naïve advanced squamous or nonsquamous NSCLC. The nonrandomized, open-label study, which began in December 2019, has an estimated recruitment of 90 patients. Investigators are evaluating ORR as a primary outcome measure and PFS and safety as secondary outcome measures. Another study is the randomized, open-label phase 1b trial of anti-TIGIT antibody ASP837414 as a single agent or combined with pembrolizumab (NCT03260322). The trial began in 2017 and expects to ultimately enroll 300 patients with locally advanced (unresectable) or metastatic solid tumors. Investigators plan to determine the recommended phase 2 dose and examine the tolerability and safety of ASP8374 as a single agent and combined with pembrolizumab. Additional outcome measures include ORR, duration of response, persistence of response after discontinuation, and DCR.
Moving Forward
Kuchroo noted that, outside of the approved agents with proven efficacy, choosing investigational immunotherapies for specific tumor types remains difficult. “There are a lot of clinical trials with anti-TIGIT [agents],” he said. “There is no immunological reason as to which tumors are going to be affected by which particular therapy. It’s all empirical right now.” Hierarchy will eventually emerge based on the results of clinical trials, Kuchroo said, adding that controversy persists regarding whether PD-L1 expression on tumors can be used as a biomarker of response to help select patients for treatment with anti-TIGIT agents.
“The time will come where we will have the agent, and it will match perfectly well with the tumor,” Kuchroo said. Until then, he added, there is no magic formula: “It’s a lot of guessing of who should get a combination and then which combination. These are all the questions that the scientific community has to grapple with.”
References:
1. Ventola CL. Cancer immunotherapy, part 3: challenges and future trends. P T. 2017;42(8):514-521.
2. Plieth J. Roche’s next immuno-oncology combo is a big bet on Tigit. Evaluate Vantage. Jan 31, 2020. Accessed August 19, 2020. bit.ly/329tz8m
3. Manieri NA, Chiang EY, Grogan JL. TIGIT: a key inhibitor of the cancer immunity cycle. Trends Immunol. 2017;38(1):20-28. doi:10.1016/j.it.2016.10.002
4. Dougall WC, Kurtulus S, Smyth MJ, Anderson AC. TIGIT and CD96: new checkpoint receptor targets for cancer immunotherapy. Immunol Rev. 2017;276(1):112-120. doi:10.1111/imr.12518
5. Anderson AC, Joller N, Kuchroo VK. Lag-3, Tim-3, and TIGIT: co-inhibitory receptors with specialized functions in immune regulation. Immunity. 2016; 44(5):989-1004. doi:10.1016/j.immuni.2016.05.001
6. Bendell JC, Bedard P, Bang YJ, et al. Phase Ia/Ib dose-escalation study of the anti-TIGIT antibody tiragolumab as a single agent and in combination with atezolizumab in patients with advanced solid tumors. Clin Cancer Res. 2020;80(suppl 16):CT302. doi: 10.1158/1538-7445.AM2020-CT302
7. Rodriguez-Abreu D, Johnson ML, Hussein MA, et al. Primary analysis of a randomized, double-blind, phase II study of the anti-TIGIT antibody tiragolumab (tira) plus atezolizumab (atezo) versus placebo plus atezo as f irst line (1L) treatment in patients with PD-L1-selected NCLC (CITYSCAPE). J Clin Oncol. 38;2020(suppl 15):9503. doi:10.1200/JCO.2020.38.15_suppl.9503
8. Roche to present first clinical data on novel anti-TIGIT cancer immunotherapy tiragolumab at ASCO. News release. Roche. May 14, 2020. Accessed August 19, 2020. bit.ly/2PBlN15
9. Compugen announces FDA clearance of IND application for phase 1/2 triple combination study of COM701 with Bristol Myers Squibb’s Opdivo (nivolumab) and TIGIT inhibitor. News release. Compugen Ltd. June 1, 2020. Accessed August 19, 2020. prn.to/3h8gTVA
10. Anti-TIGIT monoclonal antibody BMS-986207. National Cancer Institute Drug Dictionary. Accessed August 9, 2020. bit.ly/2DAXgXJ
11. Compugen announces phase 1/2 triple combination study to evaluate COM701 in combination with Bristol-Myers Squibb’s Opdivo (nivolumab) and TIGIT inhibitor. News release. Compugen Ltd. February 20, 2020. Accessed August 19, 2020. bit.ly/2EkEUdo
12. iTeos Therapeutics presents preclinical data for its anti-TIGIT antibody, EOS-448, at the AACR II Virtual Annual Meeting 2020. News release. iTeos Therapeutics. June 22, 2020. Accessed August 19, 2020. bit.ly/3iqovTD
13. Nguyen, TLA Cuende J, Preillon J, et all. Preparation of a clinical trial with a-TIGIT antagonist antibody EOS884448, which demonstrates potent preclinical activity and safe toxicology profile. Clin Cancer Res. 2020;80(suppl 16):3161. doi:10.1158/1538-7445.AM2020-3161
14. Harjunpää H, Guillerey C. TIGIT as an emerging immune checkpoint. Clin Exp Immunol. 2020;200(2):108-119. doi:10.1111/cei.13407

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More