More Analysis Is Needed of COVID-19, Cancer Interactions
As COVID-19 alters current approaches to caring for patients with cancer, early emerging research data reinforce what practicing oncologists have been observing in their patients are at increased risk of mortality.
Leora Horn, MD, MSc

As the coronavirus disease 2019 (COVID-19) alters current approaches to caring for patients with cancer, early emerging research data reinforce what practicing oncologists have been observing in their patients—that is those with cancer, particularly lung malignancies, are at increased risk of mortality. However, because data have not been fully analyzed, the impact remains clouded.
“There are conflicting data about which comorbidities impact survival, but the presence of any comorbidity is a factor,” Leora Horn, MD, MSc, the Ingram Associate Professor of Cancer Research, associate professor of medicine (hematology and oncology), and clinical director of the Thoracic Oncology Program of the Vanderbilt-Ingram Cancer Center in Nashville, Tennessee, said during a virtual presentation at the American Association for Cancer Research Virtual Meeting: COVID-19 and Cancer. “Further, it is unclear which cancer therapy is associated with worsening survival, but data suggest that chemotherapy and immunotherapy may have an effect.”
Horn highlighted findings from the TERAVOLT (Thoracic cancERs international coVid-19 cOLlaboraTion) registry-based cohort study.1,2 This registry is a multicenter observational study composed of cross-sectional and longitudinal cohort components. Eligible patients were enrolled if they had any thoracic malignancy and a COVID-19 diagnosis that was confirmed by reverse transcriptase–polymerase chain reaction, suspected contact or symptoms, or radiologic confirmation based on features consistent with COVID-19 pneumonia and symptoms.
In the study, 200 patients from 8 countries were registered. At baseline, the median age was 68 years, the majority of patients had an ECOG performance status of 0 or 1, 76% had a diagnosis of non–small cell lung cancer, and 74% were on therapy at the time of COVID-19 diagnosis. Of those patients, 57% were being treated in the first line.
The published article reported that patients were divided into hospitalized, nonhospitalized, and all patients. During Horn’s presentation, she assessed patients in 3 groups: those who recovered from COVID-19 infection, those who died, and those with ongoing infection. Patients who died were slightly older than patients in the 2 other cohorts, were more likely to be men, and had an ECOG performance status of 1 or higher. These patients were also slightly more likely to be current or former smokers.
Among hospitalized patients with cancer, the most common treatment was chemotherapy alone (33%) followed by immune checkpoint inhibitors (ICIs) alone (25%). These findings were similar in nonhospitalized patients (chemotherapy alone, 32%; ICIs alone, 20%). The majority of patients were on first-line treatment, with therapy administered a median of 7 days before COVID-19 diagnosis.
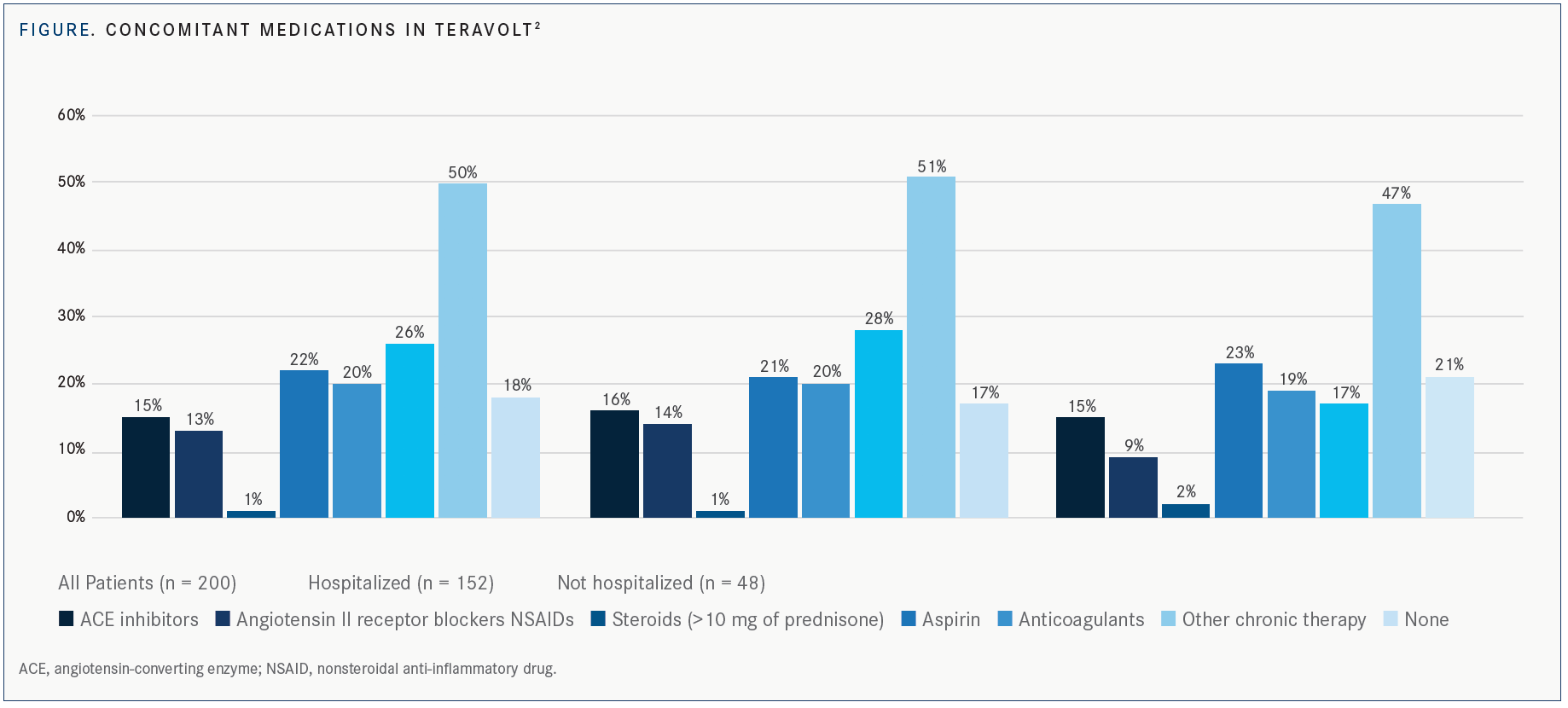
Among patients who died, Horn noted that they had had higher use of angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, anticoagulants, and steroids (FIGURE). One or more comorbidities were present among this group of patients, including chronic obstructive pulmonary disease, diabetes, vascular disease, renal insufficiency, and hypertension.
In the study, Marina Chiara Garassino, MD, and colleagues reported that 76% of patients were hospitalized and 33% had died. Of 134 patients who met the criteria for admission to the intensive care unit (ICU), 10% were subsequently admitted; the remaining 121 were hospitalized but not admitted to the ICU.
“Among patients with cancer treated in the past 3 months, many of the patients either had not been treated or were on first-line therapy,” Horn said. “Anywhere from 25% of patients who had recovered to 35% of patients who were in hospital were treated with immune checkpoint inhibitors within the last 3 months.”
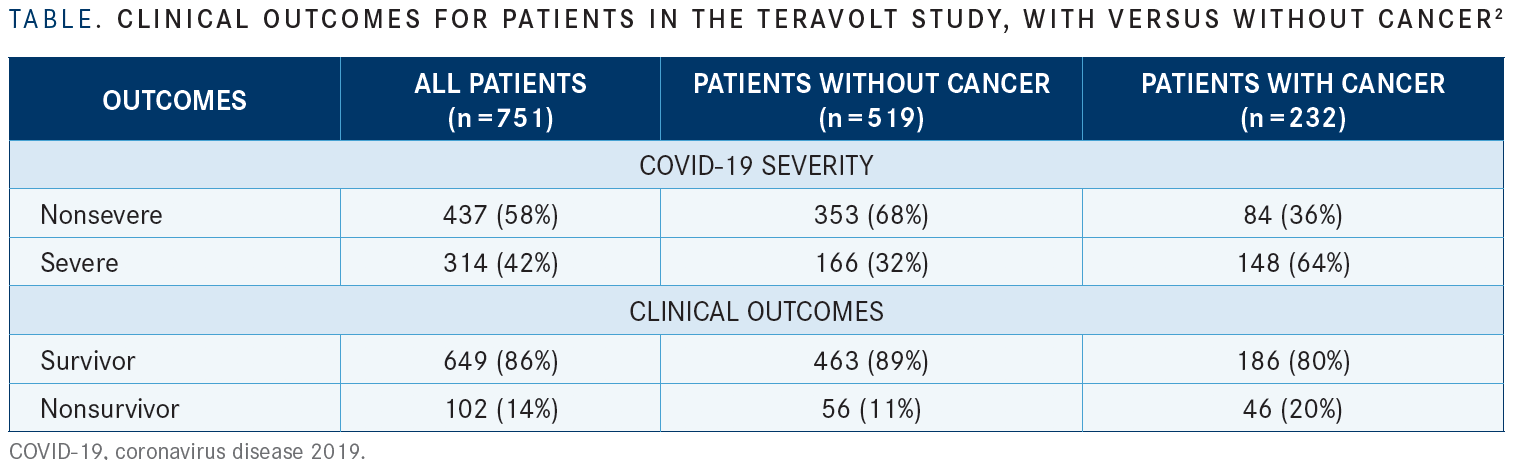
Factors affecting survival were age over 65, presence of a comorbidity, ECOG performance status greater than 1, steroid use greater than 10 mg, anticoagulation therapy at the time of COVID-19 diagnosis, and cancer therapy including chemotherapy with or without an ICI or tyrosine kinase inhibitor. “Patients with cancer were more likely to have a more severe form of COVID-19,” Horn said. “There was a higher mortality in patients with cancer—20% compared with 11% in patients without cancer [TABLE2].”
Older age, higher ECOG performance status scores, and more advanced stage of cancer were among the factors leading to a higher severity of COVID-19. “Patients were more likely to have received chemotherapy, radiotherapy, targeted therapy, or immunotherapy, but not surgery,” Horn added. In addition, patients who received their last chemotherapy treatment within 2 weeks and those whose cancer diagnosis occurred within the last year, compared with between 1 and 5 years or more than 5 years, were associated with COVID-19 severity.
Data From a Large Hospital System
Next, Horn highlighted results from a preliminary study evaluating 946 patients with cancer and resulting hospitalizations, ICU admissions, and deaths due to COVID-19 illness.3
“The rate of hospitalization was about 40%. ICU admission was less than 10%, and death rate was less than 10%,” Horn said. “When the investigators looked at severe respiratory illness, they reported that being over 65 years of age and ICI use were associated with a more severe respiratory illness.”
Horn emphasized that patients who were treated with ICIs represented a small percentage of the data set. Nonetheless, when evaluating patients with lung cancer, “the rate of hospitalization was 83% and severe respiratory illness was 58%,” she said. “This is numerically higher than those patients who have other solid tumors, in which the rate of hospitalization was 47% and severe respiratory illness was 26%.”
Another study showed that risk of death was significantly associated with advanced patient age (odds ratio [OR], 9.42; 95% CI, 6.56-10.02; P <.0001); being male (OR, 1.67; 95% CI, 1.19-2.34; P = .003); and the presence of other comorbidities, such as hypertension (OR, 1.95; 95% CI, 1.36-2.80; P < .0003) and cardiovascular disease (OR, 2.32 95% CI, 1.47-3.64; P = .0003).4
Horn said that after adjusting for age, gender, and comorbidities, chemotherapy in the past 4 weeks had no significant effect on mortality from COVID-19 disease.
“It is also important to recognize that 22% of patients were reported by sites as having their anticancer therapy interrupted because of the COVID-19 pandemic,” Horn said.
Limitations of Data
A number of limitations are associated with the data presented, Horn said, especially in regard to conflicting results on the impact of the use of ICIs. She noted that the data evaluated different end points, including death, hospitalizations, and oxygen requirements. There are no data to indicate if timing of ICI initiation is a factor and whether its use contributes to mortality, she said. In addition, there are no clear data about what therapies were administered to treat COVID-19 and the impact on outcomes.
“Compared with the general population, patients with cancer are at increased risk for mortality from COVID-19, and patients with lung cancer appear to be at particular risk,” Horn said. “Patients with cancer appear to be less likely to be offered ICU level care.” She concluded by stating there is no evidence regarding medications for COVID-19 managements and their effects on patients with cancer.
References
1. Horn L. COVID-19 and cancer: a new perspective on cancer care in the era of immunotherapy. Presented at: American Association for Cancer Research Virtual Meeting: COVID-19 and Cancer; July 20-22, 2020.
2. Garassino MC, Whisenant JG, Huang LC, et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol. 2020;21(7):914-922. doi:10.1016/S1470-2045(20)30314-4
3. Robilotti EV, Babady NE, Mead PA, et al. Determinants of severity in cancer patients with COVID-19 illness. medRxiv. Preprint published online May 8, 2020. doi: 10.1101/2020.05.04.20086322
4. Lee LYW, Cazier JB, Starkey T, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919-1926. doi:10.1016/S0140-6736(20)31173-9
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More