Roundtable Roundup: Prostate Cancer
In separate, live virtual events, Neeraj Agarwal, MD, and Alicia Morgans, MD, MPH, discussed options for a patient with metastatic castration-resistant prostate cancer after multiple lines of therapy.
Neeraj Agarwal, MD
Professor of Medicine
Presidential Endowed Chair of Cancer Research
Director, Genitourinary Oncology Program, Center of Investigational Therapeutics
Huntsman Cancer Institute
University of Utah
Salt Lake City, UT

Alicia Morgans, MD, MPH
Genitourinary Medical Oncologist
Medical Director, Survivorship Program
Member of the Faculty of Medicine, Harvard Medical School
Dana-Farber Cancer Institute
Boston, MA

CASE SUMMARY
- A man aged 75 years presented with intermittent right hip pain.
- The physical examination was unremarkable except for a prostate nodule on the rectal exam.
Clinical work-up:
- Prostate-specific antigen (PSA): 16.2 ng/mL
- Bone scan and abdominal/pelvic CT scan: negative
- Transrectal ultrasonography biopsy; Gleason 5 + 4, grade group 5
- Negative bone scan and abdominal/pelvic CT scan
- Stage T2N0M0
- ECOG performance status: 1
Treatment and follow-up:
- External beam radiation therapy plus androgen deprivation therapy (ADT) was initiated, planned for 24 months. Undetectable PSA level at 6-month follow-up; asymptomatic
- The patient did not return for regularly scheduled PSA follow-up after completion of 24 months of therapy.
Thirty-six months later:
- The patient developed new hip pain and urinary frequency.
- PSA: 29.4 ng/mL
- Testosterone: 300 ng/dL
- Bone scan showed evidence of 2 lesions in left hip (0.8 cm and 1.1 cm)
- Abdominal/pelvic CT showed 2.1-cm left pelvic lymphadenopathy and blastic lesions corresponding to uptake on bone scan.
- Germline and somatic testing are negative for pathogenic alterations.
- The patient started treatment on ADT plus enzalutamide (Xtandi) 160 mg daily. PSA decreased to nadir of 3.9 ng/mL 4 months after starting enzalutamide.
- Bone pain resolved.
- After 8 months on enzalutamide, the patient had a PSA level of 12.6 ng/mL.
- The patient had a vacation planned and declined intense PSA follow-up.
- Four months later, he returned to the office with a PSA level of 48.1 ng/mL. Abdominal/pelvic CT showed enlargement of known pelvic lymph nodes.
- Bone scan showed progressive disease, new lesions.
- New back pain and progressive disease.
- He is now considered metastatic and castration resistant.
- The patient was started on docetaxel 75 mg/m2 intravenously every 3 weeks and prednisone 10 mg daily. Clinically responded with resolution of pain and improved energy, with declining PSA
- Four cycles completed; patient developed worsening bilateral digital neuropathy throughout therapy, so therapy stopped during cycle 5
- Three months later, rising PSA, new back pain, and shortness of breath on exertion
- Abdominal/pelvic CT shows enlargement of known pelvic lymph nodes and 1 new liver lesion (< 2 cm).
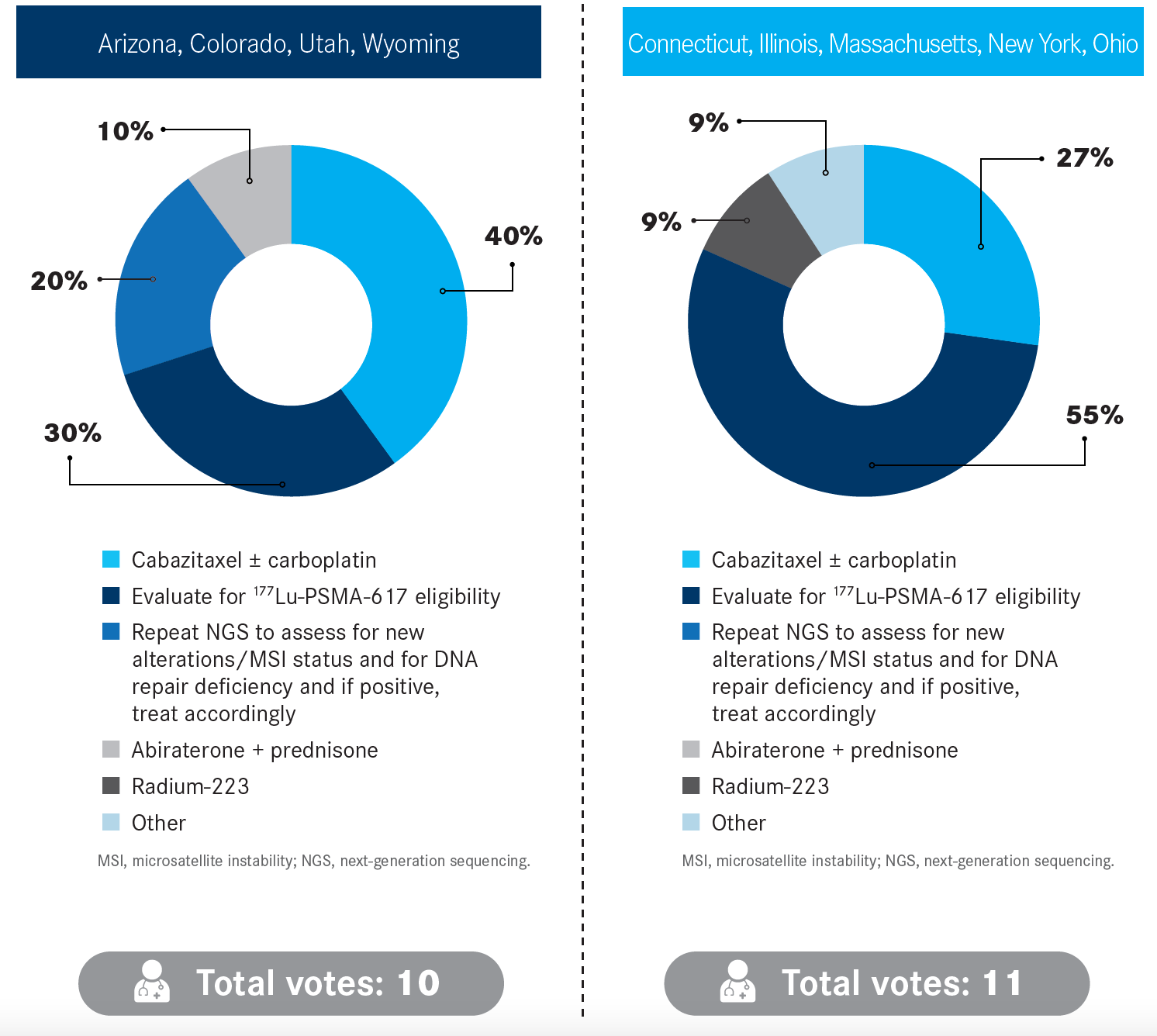
“What are you most likely to recommend now that the patient’s disease is progressing, with new liver involvement?”
REFERENCE
1. NCCN. Clinical Practice Guidelines in Oncology. Prostate cancer; version 1.2023. Accessed March 3, 2023. https://bit.ly/41DXvHT