Roundtable Discussion: Participants Consider Efficacy and Tolerability of Sacituzumab Govitecan for TNBC
During a Targeted Oncology™ Case-Based Roundtable™ event, Hope S. Rugo, MD, discussed with participants their experiences treating patients with triple-negative breast cancer.
Hope S. Rugo, MD (Moderator)
Professor of Medicine
Director, Breast Oncology and Clinical Trials Education
University of California, San Francisco Helen Diller Family Comprehensive Cancer Center
San Francisco, CA


CASE SUMMARY
A 48-year-old woman with T2N+ triple-negative breast cancer (TNBC) received neoadjuvant dose-dense doxorubicin and cyclophosphamide with paclitaxel, which she tolerated well. She underwent lumpectomy with axillary lymph node dissection. There was 1-cm residual disease in the breast and no residual disease in axillary lymph nodes. She received adjuvant capecitabine (Xeloda) for 6 cycles. Eight months after completion of adjuvant therapy, she reported worsening fatigue.
Laboratory results showed alanine transaminase was 1.5 times the upper limit of normal (ULN), and aspartate aminotransferase was 1.5 times the ULN. A CT scan showed 3 liver and 2 left lung lesions. A biopsy of the liver lesion confirmed recurrent metastatic TNBC. Brain MRI showed negative result for metastasis.
Genetic panel testing results were negative for detectable mutations. PD-L1 by immunohistochemistry (IHC) 22C3 pharmDx showed a composite positive score of 0. She had no significant comorbidities and was otherwise healthy, with an ECOG performance status of 0.
DISCUSSION QUESTIONS
- Please discuss your experiences with sacituzumab govitecan-hziy (Trodelvy) with respect to efficacy and tolerability. What is your approach to monitoring and managing adverse events (AEs)?
- How do you counsel your patients regarding sacituzumab with respect to mechanism of action (antibody-drug conjugate) and toxicity?
RUGO: Sacituzumab has not been more toxic than single-agent carboplatin in my experience, but it depends on the patient you are treating and your experience. So what has been your experience with efficacy and tolerability? How do you manage the AEs? And how do you talk to patients about this?
CHAUDHARY: In terms of AEs, [sacituzumab] is very well tolerated. As you mentioned, nausea was not a big [concern]. It was a young patient. I was not impressed with the efficacy; unfortunately, the patient progressed after the second cycle. I know this drug doesn’t cause interstitial lung disease [ILD], but there was no other explanation for her lung disease, and we thought this was all lymphangitic spread. But I did reach out to the company to see [whether] there is any incidence of ILD with the drug, and they said there is none. So we attributed it to lymphangitic spread.
RUGO: Yes. Some [patients] have disease that is resistant to everything. It is depressing. We were doing a phase 1b trial with fam-trastuzumab deruxtecan-nxki [Enhertu; T-DXd] and pembrolizumab [Keytruda], and we were on a roll because [all the patients were] responding, and then 3 patients in a row had no response. [Yet] you might want to fool yourself that a drug works for everybody. [But your patient] was probably being treated a little down the line, right?
KANG: You bring up a good point about using this drug earlier in the treatment course for a patient. Initially, when I started using sacituzumab, [I was using it] quite late in almost a Hail Mary situation, because it was before the ASCENT trial [NCT02574455] had come out. These patients were heavily pretreated, and maybe related to poor baseline performance status, tolerability was tough with me. I had patients complain about a lot of nausea, and the neutropenia was a huge issue. But now that you mention it, as I have started reaching for sacituzumab much earlier in the course of therapy, I had 1 patient who didn’t even tolerate single-agent capecitabine, probably because it wasn’t helping control her disease. We gave her 1 dose of sacituzumab and her nausea went away. Her strength and her appetite got better. The point is well made that this drug is effective, and if you are effective at controlling disease, you are going to keep your patient feeling better.
RUGO: What kind of antinausea drugs do you give when you first give the drug?
KANG: I don’t think I was doing the NK-1 [neurokinin-1] inhibition; I wasn’t using aprepitant [Emend]. Probably dexamethasone [and] ondansetron.
RUGO: Yes, I generally start with a 2-drug regimen with dexamethasone. With T-DXd, I have been giving a triple-drug regimen and backing off if patients have no nausea, because we have had so much nausea with T-DXd. But with sacituzumab, generally a 2-drug regimen works. But you can always add in your NK-1 [inhibitor]. We see patients who have such huge variations in their toxicity. I have only had 1 patient who had bad diarrhea, but I know physicians have seen this, so it’s an important thing to keep in mind. If a patient does have bad, continuous diarrhea that they can’t manage, dose reducing is a good way to manage it.
CHANDURI: I had an elderly patient last year when the drug was just released. I started her on this drug as a third-or fourth-line [therapy]. After the first course, she ended up in a nursing home that was not close to us, so I didn’t manage her. But she had neutropenia, infections, and diarrhea. She had bad toxicity. Lately I have a couple of younger patients who are doing very well, with no nausea. I usually use only 2 drugs, dexamethasone and ondansetron, and they are doing well.
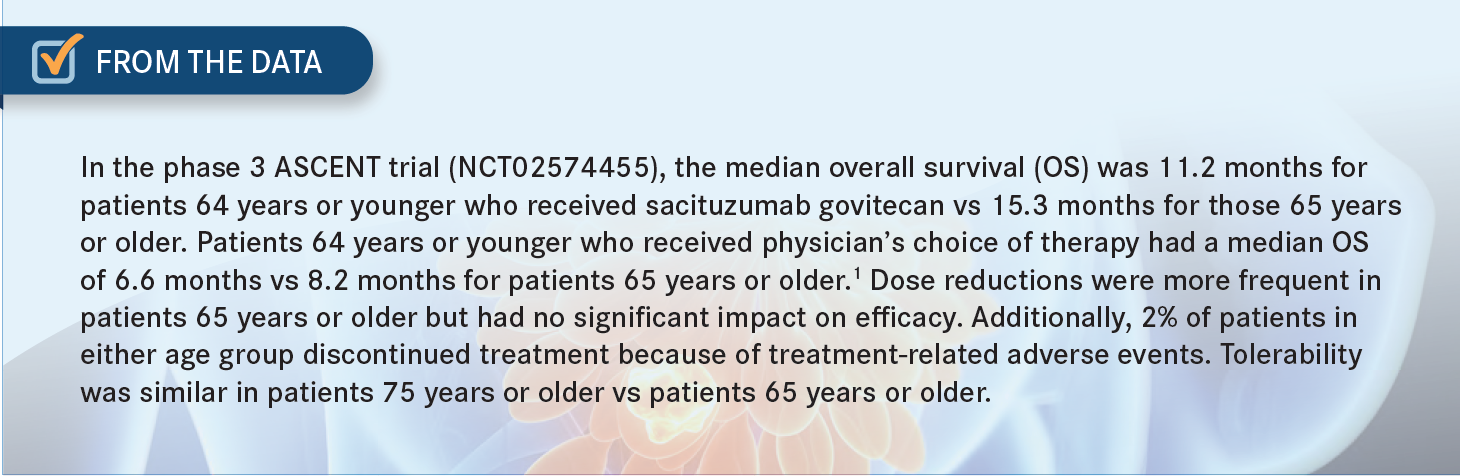
RUGO: If you look at all the FDA reports and other [reports] looking at older patients, [you see] the metabolism of drugs and the renal clearance drop off, and we do see more toxicity. Although if you can give the drug, the patient receives the same benefit. In ASCENT, we did an analysis looking at patients 65 years [or older] and others 70 [or older], though the numbers got much smaller. And it looked like the benefits in progression-free survival [PFS] and overall survival [OS] were at least similar, although the numbers were small.1
I treated a woman who had bone-only TNBC, and she ended up with liver metastases. She’s a [smaller] woman…and I gave her 1 dose of sacituzumab, and she did end up in the hospital for a cancer-related reason. Then I reduced the dose and gave it every other week, and she tolerated it incredibly well. Eventually I went up to the full dose every other week with growth factor support. She stayed on it for 8 months, and she [recently] went off. I was impressed. She went back to her normal activities. She cooked; she hung out with her family. This is a woman in her early 80s. It made a huge difference. So I got sold on the idea that if you have a fragile or [older] patient, maybe starting with a lower dose when you first give the drug would be better, using growth factors for frail or older patients up front and even treating every other week in patients you don’t think can tolerate 2 weeks on, 1 week off.
MOSALLAEI-BENJAMIN: I have 1 patient who had a hormone-positive tumor and had a recurrence after 15 years. She came in with pancytopenia and didn’t have any disease on the scan. But I did a bone marrow [biopsy], and her marrow was full of triple-negative [disease].
She had 6 months of docetaxel [Taxotere] and did well. Her counts came up, but then she had progressive disease. And I put her on sacituzumab, and she has been on that for about 38 cycles, and she has done well. She hasn’t had neutropenia, and I was worried about that because of the marrow involvement, but she has done incredibly well.
RUGO: If you look at intrinsic subtyping for those patients who [develop] triple-negative [disease] in the metastatic setting, we interrogate the sample as much as possible, because we are suspicious that they might still have estrogen receptor [ER]-positive disease. But if you had a marrow [aspiration], they should have been able to look for ER without decalcifying, right? So these tumors are still luminal; they are usually luminal B-like tumors, so they are more chemosensitive, which is better. But that’s amazing, 38 cycles.
MOSALLAEI-BENJAMIN: And it keeps going.
RUGO: I have a young patient who [experienced] relapse with brain metastases and lung tumor, and I think she was approximately 2 days off her adjuvant [capecitabine]. These are the kinds of patients who do poorly, but we treated her with sacituzumab up front. She needed 1 more treatment for brain metastases, and we radiated a bone lesion, but her lung disease went away, and it hasn’t come back again. I think she has been on [the regimen] for 7 months. That’s impressive. Some patients can get huge mileage out of the drug even though they seem like they would only stand treatment for 2 or 3 months.
DISCUSSION QUESTIONS
- What is your overall approach to molecular testing at metastatic relapse or progression? Have we learned anything about the value of potential biomarkers to guide the use of this agent (eg, TROP2 expression or germline BRCA1/2-mutation status)?
- What therapies were given to the patients who were randomly assigned to the comparator arm? How does that inform your use of sacituzumab vs other options?
RUGO: In terms of molecular testing, we did look at TROP2 expression in the ASCENT trial, and it didn’t seem that the TROP2 level correlated with the activity of sacituzumab,2 probably because of a bystander effect where the drug leaks out and kills neighboring cells. It was impactful to me that more than 50% of patients in ASCENT had eribulin [Halaven] in the treatment of physician’s choice [TPC] arm,3 because the last chemotherapeutic drug that got approved before sacituzumab was eribulin, based on results [from] the EMBRACE trial [NCT00388726].4
That was a heavily pretreated patient group [with] ER-positive, triple-negative, and HER2-positive [disease] at the time. It [afforded] a small but significant OS benefit [median OS, 13.1 months vs 10.6 months for eribulin vs TPC, respectively].5 So it’s even more impactful that sacituzumab was better than eribulin [median OS, 12.1 months vs 6.9 months for sacituzumab vs eribulin, respectively].6
The other thing we looked at was whether having a germline BRCA1 or BRCA2 mutation [influenced] the effectiveness of sacituzumab, and it doesn’t, as you would expect. But you don’t know until you look at it. The benefits in PFS and OS were very similar [in patients with and without BRCA1/2 mutations] and, if anything, were better in patients who had germline BRCA1/2 mutations, but the numbers were small [so] you can’t make a conclusion about [sacituzumab] being better. [But] at least you know it’s positive. And 80% of patients had medium to high TROP2 expression, and their benefit was the same [as that of the overall primary efficacy population].2
There [were so few] patients with low TROP2 expression that it’s hard to know exactly how to interpret those [results], and there wasn’t a validated test for TROP2. Although now there is more validation of this test for TROP2, so that’s helpful [in deciding] whether we should be checking for TROP2.
DISCUSSION QUESTIONS
- What are you using most often as next-line therapy for progression on or after sacituzumab?
- If you aren’t using sacituzumab in the second line, what are you using and why?
RUGO: If patients progress on sacituzumab, what are you giving them next?
SWEET: Whatever is left.
RUGO: Is there a preference of sequencing? What if a patient had an IHC score of 1+?
ZIARI: For a score of IHC 1+, I would do T-DXd.
RUGO: When in the sequence would you give the T-DXd?
ZIARI: I would do it for the second line.
RUGO: Instead of giving sacituzumab?
ZIARI: I would if the IHC score is 1+.
RUGO: You would give T-DXd instead of sacituzumab for triple-negative disease that’s HER2 1+?
ZIARI: For IHC 1+, which is HER2-low [disease], I would.
RUGO: That’s interesting. [What] does everybody else think about that?
MOSALLAEI-BENJAMIN: I would give sacituzumab first and then do the T-DXd subsequently.
KANG: Yes. With sacituzumab, you have a large, randomized trial in the triple-negative population, whereas in the DESTINY-Breast04 trial [NCT03734029] of T-DXd, [the triple-negative population] was a subset in the study of HER2-low breast cancer, and it was a relatively small subset.
MOSALLAEI-BENJAMIN: Sacituzumab also doesn’t have the approximately 6% to 10% rate of ILD that T-DXd can have.7,8
RUGO: Yes. The ILD rate is somewhere between 12% to 13% overall,7 and the mortality rate in patients with HER2-positive disease was 0% in DESTINY-Breast03 [NCT03529110],9 but there were deaths in DESTINY-Breast04.10 You have to monitor it carefully and check the CT scans. But it is a very effective drug. The primary end point was in the hormone receptor–positive, HER2-low population; this is what we were talking about [regarding] sequencing. I still want to use the phase 3 data with more than 500 patients9 vs the [data from the] 58 patients who were in DESTINY-Breast04,10 but I think the sequencing is an interesting question. And if a patient refused sacituzumab, then you have another option, but generally [patients] haven’t [refused].
[In the ASCENT trial,] there was similar efficacy [between] age groups. But [regarding] the frailty of older patients, there could be more hematologic toxicity. So in that situation, one might want to start low and then go up on the dose if patients tolerate it, [because] it is very hard for us to predict. The AEs were similar [for patients 75 years or older vs patients 65 years or older]. But when we get into the real-world population, we always see differences. But you are still getting an improvement in OS in the older patients, so it is worth it [From the Data1].
DISCUSSION QUESTIONS
- What are the goals of therapy?
- Which efficacy end points are most meaningful (OS, PFS, clinical benefit rate, objective response rate, time to response, or duration of response)?
- Which factors influence your decision-making?
RUGO: Does OS generally drive your decisions about treatment? Or are PFS and toxicity more important?
MOSALLAEI-BENJAMIN: PFS and toxicity are more important, especially toxicity.
RUGO: And how well it can be managed for your patients.
SWEET: I agree.
RUGO: So PFS and toxicity more than OS, but OS is a good icing on the cake.
CHEN: If you give [a] treatment relatively early in the [sequence], you may want to look at OS advantage. After 2 or 3 lines, the PFS and toxicity will be very important. Because at that point, preserving some quality of life might be very important to the patient.
CHANDURI: I had a patient who presented with metastases in bone, liver, and lung, and then we found out that she had a mass in her breast. And for this patient, PFS [and] toxicity [are] more important…. She is doing well. She has triple-negative disease. I was able to give her chemoimmunotherapy.
She has been on sacituzumab for almost 6 cycles and is doing extremely well, [though she] was in bed for more than 6 months. Now it has been almost 3 years, but she asks me, “Am I going to be curable? I know I’m not, but I want this drug as long as I can tolerate it.” I don’t know. Her breast mass has completely disappeared and the PET scans look good, but she started progressing on sacituzumab. She is doing well now.
RUGO: Yes, it’s interesting [to consider] those patients who have long responses and try to understand. The comments about OS vs PFS in the late-line setting are interesting because in ASCENT the median [number of prior] lines of therapy in the metastatic setting was 3. OS was almost doubled [12.1 months (95% CI, 10.7-14.0) vs 6.7 months (95% CI, 5.8-7.7) for sacituzumab vs TPC, respectively].3 If you can control the AEs and the toxicity, that’s an important end point for a lot of our patients, who are afraid that death is around the corner. That does have a big impact for those patients.
REFERENCES
1. Kalinsky K, Oliveira M, Traina TA, et al. Outcomes in patients (pts) aged ≥65 years in the phase 3 ASCENT study of sacituzumab govitecan (SG) in metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1011. doi:10.1200/JCO.2021.39.15_suppl.1011
2. Bardia A, Tolaney SM, Punie K, et al. Biomarker analyses in the phase III ASCENT study of sacituzumab govitecan versus chemotherapy in patients with metastatic triple-negative breast cancer. Ann Oncol. 2021;32(9):1148-1156. doi:10.1016/j. annonc.2021.06.002
3. Bardia A, Hurvitz SA, Tolaney SM, et al; ASCENT Trial Investigators. Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med. 2021;384(16):1529-1541. doi:10.1056/NEJMoa2028485
4. U.S. FDA approves Eisai’s Halaven (eribulin mesylate) injection for treatment of metastatic breast cancer. News release. Eisai Global. November 16, 2010. Accessed February 10, 2023. https://bit.ly/3I5I2XR
5. Cortes J, O’Shaughnessy J, Loesch D, et al; EMBRACE Investigators. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377(9769):914-923. doi:10.1016/S0140-6736(11)60070-6
6. O’Shaughnessy J, Punie K, Oliveira M, et al. Assessment of sacituzumab govitecan (SG) versus treatment of physician’s choice (TPC) cohort by agent in the phase 3 ASCENT study of patients (pts) with metastatic triple-negative breast cancer (mTNBC). J Clin Oncol. 2021;39(suppl 15):1077. doi:10.1200/ JCO.2021.39.15_suppl.1077
7. Enhertu. Prescribing information. Daiichi Sankyo; 2022. Accessed February 10, 2023. https://bit.ly/3jZzYjE
8. Trodelvy. Prescribing information. Gilead Sciences; 2023. Accessed February 10, 2023. https://bit.ly/3YDxlCX
9. Hurvitz SA, Hegg R, Chung WP, et al. Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomised, open-label, phase 3 trial. Lancet. 2023;401(10371):105-117. doi:10.1016/S0140-6736(22)02420-5
10. Modi S, Jacot W, Yamashita T, et al; DESTINY-Breast04 Trial Investigators. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387(1):9-20. doi:10.1056/NEJMoa2203690