Roundtable Discussion: Combination Therapies Available for Relapsed Patients With Triple-Refractory Multiple Myeloma
For patients who relapsed on their prior therapy and have triple-refractory multiple myeloma, selecting the best next-line of therapy is an important decision for their disease outcome. During a Targeted Oncology Case-Based Roundtable event, Peter Forsberg, MD, discussed this topic with a group.
Peter Forsberg, MD

For patients who relapsed and have triple-refractory multiple myeloma, selecting the best next-line of therapy is an important decision for their disease outcome. During a Targeted Oncology Case-Based Roundtable event, Peter Forsberg, MD, of the University of Colorado Health discussed this topic with a group.
FORSBERG: When you’re thinking about a new therapy in a patient, what things are important considerations in terms of your treatment? If you’re looking at second- or third-line therapy, what patient or disease or treatment considerations are at the core for you?
R. FAHED: [I would say] all the above, every patient progressing on the lenalidomide [Revlimid]-based treatment and daratumumab [Darzalex]-based treatment. I’ll take those [treatments] into consideration. I think the efficacy is a [major consideration] and then tolerance is secondary. For a patient [who previously received daratumumab plus lenalidomide], I would go with a bortezomib [Velcade]-based regimen. I think we have 2 FDA-approved options. We have the [bortezomib and daratumumab, which] I don’t like, or we have the selinexor [Xpovio], bortezomib, and dexamethasone as a reasonable second-line option now.
FORSBERG: This scenario of daratumumab and [lenalidomide] up front…I think is becoming a more common scenario. The question of what we’re thinking about doing in the second line in these older patients is a new consideration. I think a proteasome inhibitor is probably going to be a primary consideration for most patients.
FORSBERG: Do your patients force you to think more about convenience or cost, or are they amenable when you recommend something that you think is going to be the most active or best tolerated?
SRIVASTAVA: That would probably be the most important thing, also including efficacy—the drug performance, and usually at the time of second line, a lot of them are still open. If [the patient has] done well on the first-line regimen, I think they’re still fully encouraged to go on to second line. But as the lines keep increasing, I think the patience with treatment starts to decrease [as a consideration], [and] the convenience starts to become more important. Quality of life [is] important at any point.
Here in Colorado Springs [at UCHealth Cancer Care and Hematology Clinic Memorial Hospital North], we see a lot of patients who [come from farther away], so that is also something we must factor in. I think any oral medications, even though [they are] convenient, sometimes the co-pays can be high. I’ve run into that problem sometimes, but I think it just depends on the individual patient, what plan they have, and whatever assistance they can provide, so it’s the multitude of all those factors.
FORSBERG: I would guess that with providers from Wyoming, Eastern Colorado, Montana, and Nebraska you’re going to have a lot of [patients] traveling a long way to the infusion center and [facing] the challenges that come along with that. Do people end up trying to find all the oral combinations more often or trying to find regimens that reduce infusion center visits to accommodate your outlier patients?
E. FAHED: Twice-weekly carfilzomib [Kyprolis] is a problem for patients.
FORSBERG: I think twice-weekly carfilzomib is a problem for somebody who lives next door to the infusion center. I don’t think I have had a patient on twice-weekly [carfilzomib] for a little while now, just because we’ve got to think about quality-of-life considerations to some degree.
E. FAHED: [Regarding] using the oral regimens for somebody who’s far away, they’re not as effective. That’s my problem. If somebody is [coming from far away], I’ll probably go with a better, more efficacious regimen versus [a better] quality-of-life regimen. If somebody is older and frail, I would go with the doublet treatment and dexamethasone.
FORSBERG: Does anybody feel [insecure] at all about switching from lenalidomide? Are there patients you don’t like switching from lenalidomide to pomalidomide [Pomalyst] or switching the class, or does it depend on whether they’ve done well with it? Or is anybody a good candidate to go from lenalidomide to pomalidomide as part of their second-line combination?
R. FAHED: [For] deletion 17p [del(17p)]...I think we may have good success with proteasome inhibitors. After progression on a CD38 [antibody] and lenalidomide, I would think about the regimen including proteasome inhibitors.
E. FAHED: I would [use] both for patients with del(17p), and then pomalidomide, carfilzomib, and dexamethasone.
FORSBERG: Pomalidomide has some good data—nothing phenomenal. It’s one where, hopefully, there may be some things emerging that show [better data].
[For older patients], we’re probably not going to do\ a quadruplet, but I think sometimes these questions of backbone get oversimplified [when we think about a] triplet.
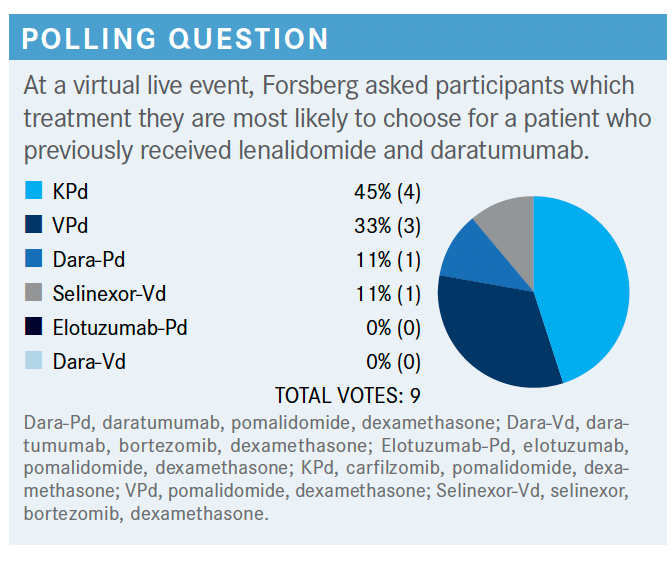
FORSBERG: What’s the most common secondor third-line regimen that you guys are using now in terms of daratumumab, carfilzomib, and pomalidomide? We mentioned briefly selinexor and inotuzumab [Besponsa]. Do you have any that you would consider a go-to in the second or third line for most patients?
THOMAS: I think you have to figure out what you’re going to use up front. Everybody’s a little bit different in what they use up front, [and you must decide] whether you’re going to use a CD38 antibody. Knowing that the patient is probably going to get fourth- or fifth-line therapy, [you have] to make sure that somebody is not eligible as they move forward with all the different classes of drugs. For me, daratumumab is a second-line therapy. I think carfilzomib’s always good, and so is pomalidomide. [That is also the problem when deciding: All these options are good.]
FORSBERG: That’s a good thought. I think sometimes we get the question “What’s your go-to fourth-line therapy?” and we can’t even agree on second line. I think we have some fairly crystallized thoughts about first-line treatment in different patient populations, but you’re right. I think that prior treatment exposures are a big factor.
SRIVASTAVA: If [you have] somebody high risk or if you used carfilzomib up front—so, KRd [carfilzomib, lenalidomide, dexamethasone]—then maybe that would be a secondline option in that scenario. But I have patients who went on VRd [bortezomib, lenalidomide, dexamethasone] who didn’t quite get complete responses, and I switched them to carfilzomib and got a deeper response. It just depends on what your first-line option was and then patient factors.
FORSBERG: I think daratumumab has been a solid backbone second- and third-line treatment for us. But as we move more [to] first line, we’re left with more second-line consideration of somebody who’s had a CD38 therapy and carfilzomib. I might be using less up-front carfilzomib now that we had the negative study of VRd versus KRd. For me, it has pushed carfilzomib more consistently into the second line, using carfilzomib and pomalidomide as backbone in the second line.
FORSBERG: Have you noticed any changes in your approach over the last 12 to 24 months? Anything that has shifted your early relapse pattern?
MUSHTAQ: It depends on what the first-line therapy was or comorbid conditions. What is the age? There are so many different [factors to consider]. I have patients who are old and frail, and they want to avoid coming to the infusion clinic. They just want everything as oral treatment. I try lenalidomide mixed with the dexamethasone. If they have aggressive disease and they have used both bortezomib and lenalidomide in the past, then carfilzomib would be an option. It depends on all the factors encountered, especially the comorbid condition and the performance status of the patient.
FORSBERG: It’s not a one-size-fits-all [treatment for patients with] multiple myeloma. I think we must consider all those things: prior treatment, how they respond and how they tolerate it, comorbidities, and what you need to accomplish with your therapy.
FORSBERG: Has anybody used selinexor, whether for patients with multiple myeloma or in patients with relapsed diffuse large B-cell lymphoma? How familiar are you all in terms of use of selinexor in the clinic?
E. FAHED: Patients on selinexor, bortezomib, and dexamethasone had excellent responses with disease. Outstanding response over remission....[There was a] patient who had triple-refractory multiple myeloma and had almost tried everything else already.
THOMAS: Did you use the weekly dosing?
E. FAHED: It was 100 mg [at first], now down to 60 mg.
FORSBERG: I’d say that’s a common scenario. I think dosing has been a moving target in a good way, for the most part, since that first approval came out with the twice-weekly dosing with just dexamethasone in the more heavily pretreated patients. That’s a dosing structure that I don’t know anybody could really handle, so I think getting folks on the weekly dosing and then finding dose flexibility to keep patients on it has been a real achievement.
THOMAS: [I had one patient on selinexor] and I feel like it’s something I think about in the salvage setting. I did it with lenalidomide, and that patient had a pretty good response. We started at 80 mg and I didn’t have too many cytopenias with it. The patient didn’t get as great a response as I’d like fast enough, but that’s what you get in sixth-line therapy.
FORSBERG: I think it’s certainly one of the new drugs. It’s a question of how we pull all these drugs together and how we sequence them [that] is the biggest emergent question in multiple myeloma these days.
FORSBERG: Is selinexor something you’re going to use in patients who are ineligible or not wanting to go to CAR [chimeric antigen receptor] T-cell therapy? Is it something you’re going to use in patients who want an oral [drug] for part of their combination? Is there anything specifically that you think helps it fit into the current treatment landscape?
THOMAS: I think the one thing that stood out to me was a subset analysis in the BOSTON trial [NCT03110562] for the elderly patients.1 That is something I didn’t know and would be interesting to put into a second- or earlier-line therapy for our triple-refractory patients up front.
FORSBERG: Of the subgroup analyses, I think that was the one that surprised me the most in terms of the consequences— we think that they did get that much benefit.
R. FAHED: It would be a second line for a patient who cannot tolerate [carfilzomib]-based treatment. Or if not, it would be the last on the list after exploring all options for patients with multiple myeloma who have triple refractories. [I would put it after belantamab mafodotin (Blenrep).]
FORSBERG: You’re putting it after? Below belantamab mafodotin and CAR T-cell therapy?
R. FAHED: At the bottom of the list. Either we use it in the second-line setting in combination with bortezomib or as a dual therapy with dexamethasone, but...it is the second or the last [on the list].
FORSBERG: If you start a patient on this combination, you have to watch them closely. You have to monitor counts routinely—even [though] they don’t have to be in infusion if you started selinexor with a lenalidomide-based combination or off-label. But whatever you may use, you do need to watch, especially during the first cycles. Getting people over the hump of the initial month or 2 on therapy is often the most challenging time. I often will send a patient to one of our dietitians prior to starting therapy to talk about it. We counsel them on some of the ways they can try to keep their sodium up, eating salty foods, trying to deal with volume issues. Then at least we start with 2 antiemetics straight away with a 5HT3 [receptor antagonist] and usually use olanzapine [Zyprexa].
I think they’re on the edge if they’ve had nausea with other regimens and they have some baseline issues. I’ll often add a neurokinin-1 [receptor] antagonist as well—[also] bringing people back in case they need intravenous hydration, as well as in case they need intravenous antiemetics.
REFERENCE
Grosicki S, Simonova M, Spicka I, et al. Once-per-week selinexor, bortezomib, and dexamethasone versus twice-per-week bortezomib and dexamethasone in patients with multiple myeloma (BOSTON): a randomised, open-label, phase 3 trial. Lancet. 2020;396(10262):1563-1573. doi:10.1016/S0140-6736(20)32292-3
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More











