Roundtable Discussion: Atlas Considers Sequencing for a Patient With Basal Cell Carcinoma
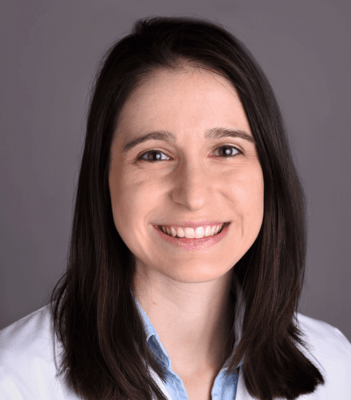
During a Targeted Oncology case-based roundtable event, Jennifer L. Atlas, MD, discussed the case of a patient with infiltrative basal cell carcinoma with participants.


Jennifer L. Atlas, MD (Moderator)
Medical Oncology and Hematology
Levine Cancer Institute Morehead
Atrium Health
Charlotte, NC

ATLAS: Based on the NCCN [National Comprehensive Cancer Network] guidelines on BCC, it’s important to think about it from a risk group stratification standpoint, which is low-risk vs high-risk lesions.1
Low-risk lesions are typically present on the trunk and extremities; less than 2 cm in size; well-defined, primary lesions; not in immunosuppressed patients; no previous radiation to the site; nodular or superficial; and without perineural invasion.
High-risk lesions on the trunk and extremities are usually greater than 2 cm in size, so these are locally advanced lesions and in difficult places to treat such as cheeks, forehead, scalp, neck, and pretibial area. Anything that’s greater than 1 cm in these sites, I would call a high-risk lesion. The mask areas such as across the central face, the eyelids, eyebrows, periorbital, nose, and lips are high-risk areas, as well as the postauricular area, temple, and ear. They are poorly defined, recurrent lesions in patients who are immunosuppressed and occur in a site of previous radiation. They have perineural invasion and an aggressive growth pattern.
Based on the NCCN guidelines for locally advanced BCC [laBCC], which is what this patient has, and metastatic BCC [mBCC], systemic therapy may be considered. It is used where topical therapy, surgery, or radiation are not likely to be curative. Locally advanced disease is defined as primary or recurrent local disease not amenable to surgery or radiation. Multidisciplinary consultation is key in the treatment of these patients.1
Systemic therapy options include hedgehog pathway inhibitors [HPIs]. [Because of] the frequency…of intolerable adverse events [AEs] associated with these inhibitors, drug holidays or even alternative dosing regimens need to be used to allow for improved adherence to therapy. This approach has been used for patients who have certain hereditary syndromes such as Gorlin syndrome. Current FDA-approved HPIs include vismodegib [Erivedge] and sonidegib [Odomzo].
There’s also an emerging role, and now an FDA approval, for immunotherapy in this setting with cemiplimab [Libtayo] for patients with laBCC or mBCC previously treated with an HPI or in those for whom an HPI would not be appropriate. This also includes patients who had stable disease or lack of response after several months of therapy.1,2

ABHISHEK: Cemiplimab has a history in skin cancer; it is well tolerated and can offer a decent response as well as durable response. So why not?
KHAN: We have much more experience and comfort levels with prescribing immunotherapies, so…our thresholds to use these drugs are lower compared with a new drug like an HPI. Familiarity with immunotherapy makes us pull the trigger quick.
HAGAN: I would love to use it, and…the major concern would be my understanding of the FDA approval is that it is approved for use after an HPI or in those for whom an HPI was not thought to be appropriate. A lot…would depend on how strict the insurance companies were about using it. I think most oncologists are seriously in love with immunotherapy and molecularly targeted therapy. The fact that we have 2 drugs in this situation that we could use is awesome. But whatever I could get for the patient, I’d try to get.
YUAN: I have very little experience using both HPIs as well as cemiplimab. From my very limited experience, I will choose the immunotherapy because of HPI AEs, such as the [debilitating] fatigue for my patient. That’s all I’m thinking, maybe just to choose immunotherapy [because] it’s a little bit better tolerated.
ATLAS: What I’m hearing is that we in the oncology world, whether you predominantly treat skin cancers or general oncology, have a lot more familiarity with using immunotherapy and are well versed in its AEs. I [would not use cemiplimab]. The indication truly is for patients who have either a contraindication to an HPI, have failed an HPI, or had intolerance to therapy. These indications were listed on the trial [NCT03132636] that led to the approval of cemiplimab.3 In my practice, if he did not have a contraindication, I would at least attempt therapy with an HPI first.

ABHISHEK: If the patient had a good response, at least from the local standpoint, I think a drug holiday would be appropriate. Is the patient at a point that they could have more surgery? That would be a consideration at this point, as well.
ATLAS: A drug holiday was an option, and that’s a great choice. [Another option is an] amenable surgical plan. Often in my team, this includes multiple [surgeries]. He’s had nice closure over the nose. I usually do repeat biopsies around the original periphery to see whether we have active disease.
We could think about treatment discontinuation if we had negative biopsies and could move on to observation. I think one other thing to consider if we still have active disease—because it’s not an aesthetic location or a location amenable to local regional management—is moving to an intermittent dosing pattern. One trial that specifically looked at this….is the MIKIE trial [NCT01815840], which was a phase 2 trial that looked at 2 different intermittent dosing regimens. One was using vismodegib for 3 months on, followed by an 8-week drug holiday.
That is something I incorporate into my strategy for treating these patients often. They also had an alternative regimen doing a 6-month lead-in of vismodegib followed by a 2-month-on, 2-month-off treatment pattern to allow for drug intolerance.4 Then there is the immunotherapy option that we could move to for a patient who had intolerance to HPIs. Those would be some of the options I would see at this point for this patient.
KHAN: Why is dose reduction not an option?
ATLAS: They did not look at dose reduction in any of these clinical trials of the 150-mg tablet, which is the tablet size for vismodegib. So there’s not really a drug reduction option, and we typically don’t ask that patients divide these tablets from an administration standpoint. I’ve seen dermatologists sometimes go to every-other-day dosing. I find…that the time frame for people to recover from the toxicities takes longer than that.
I don’t usually find that it makes a huge difference going to every-other-day or every-third-day dosing patterns, and that’s why I typically take these longer breaks off if tolerated.
KHAN: Why does the company not try them? They had studies with the 2-month-on, 2-month-off regimen, so why not come with a lower dose [because] that may pan out and make it more tolerable?
They could have some of it in smaller-dose tablets as well, if they know that it [decreases] problems.
ATLAS: They would have to do pharmacokinetic studies and prove benefit, which haven’t been done. But it’s a good question.
YUAN: In case you give a drug holiday and the cancer has recurred….do you rechallenge with an HPI or just switch to the immunotherapy?
ATLAS: Previously, when we did not have the FDA-approved immunotherapy option, you could rechallenge. People can still have excellent responses with rechallenge. The bigger aspect is, can they have tolerance to the drug?
That’s what I’ve noted in my clinical practice. If I rechallenge and someone is intolerant to the drug, then I immediately would shift to immunotherapy. Also based on the grade and number of toxicities, I will often think about shifting to immunotherapy in that setting.

ATLAS: In my...practice, moving from one of the HPIs to the other has not, traditionally, overcome resistance if someone’s progressing, or having intolerance, because they share many of the same AEs. But it is a strategy that could be considered.
HPI eligibility should be determined by a medical oncologist. There are dermatologists who prescribe, in many areas, and so a clinical evaluation [is needed to assess] whether somebody has a surgical option, a radiation option, or whether systemic therapy is the ideal option….Do they have a low-risk or a high-risk lesion? Do they have some sort of comorbidity that excludes them or [that] we think is going to have a high rate of toxicity? These would be the patients I might think about not starting with an HPI and moving toward immunotherapy.
For patients who’ve received anti–PD-1 therapy prior to a HPI, we don’t have any clear data on that. In my…clinical practice, which revolves around treating cutaneous malignancies, I have many patients who’ve had multifocal tumors, whether it is BCC, cutaneous squamous cell carcinoma, or they have more than 1 diagnosis like melanoma plus another disease.
I do have some experience in giving PD-1 therapy before someone gets an HPI and it can be very successful as a frontline approach….It’s reasonable to use for the right patient in the frontline setting, although the current FDA approval would be for use after an HPI unless the patient’s not a candidate.
KHAN: I think it is also [an option] for somebody who is not [adherent] on oral drugs.
ATLAS: That’s a really good answer, and that’s a problem we have in oncology. I think part of the problem with laBCC sometimes is, it was a neglected lesion. If we can’t rely on the patient to consistently take the drug, should we be starting with an intravenous medication?
HANNA: I have not [given frontline PD-1 therapy], but my understanding is [most] patients with BCC have a high tumor mutational burden [TMB] and typically patients with a high TMB have a higher chance of responding to immunotherapy. To me it makes sense to use it up front. It’s a good idea, but we need to have a clinical trial behind that.
KHAN: I think the other rationale is that the duration of response from the immunotherapy, even as a second-line agent, seems to be decent. You would hope that you can use an up-front immunotherapy that can provide durable control, like you’ve seen in other malignancies that use immunotherapy, rather than a short-lived [response].

KHAN: A very important goal in locally advanced disease is providing good long-term disease control by surgical resection after a good response.
The rational designer drug approach would be where you say, “This patient is going to benefit from PD-L1 [agents] and this one is going to benefit from an HPI.” Have a target, so that I can be more educated in this age where I’m trying to use rational approaches rather than throwing drugs at [individuals].
HAGAN: You’ve already touched on trying to know the ideal sequencing. We got burned in lung cancer, when our EGFR-mutated cancers turned out to be strongly PD-L1 positive, but when we used the PD-L1 agent first, there was no response rate and then toxicity was worse when we went to osimertinib [Tagrisso], a drug that would have worked better if we had just waited for the EGFR [test] to come back.
I also think having 1 target is probably suboptimal. It would be nice if we could find some other targets; like with colon cancer, for example, we can target angiogenesis and we can target EGFR. Hopefully someday, we’ll be able to target KRAS. Finding other targets, so we could have nontoxic therapies, would be great. It seems like already a lot of these patients are somewhat older, their skin is in terrible shape, and they have more than 1 cancer.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Basal cell skin cancer, version 1.2022. Accessed January 17, 2022. https://bit.ly/37fg4Hn
2. FDA approves cemiplimab-rwlc for locally advanced and metastatic basal cell carcinoma. FDA. February 9, 2021. Accessed January 17, 2021. https://bit. ly/2VjB5y8
3. Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):848-857. doi:10.1016/S1470-2045(21)00126-1
4. Dréno B, Kunstfeld R, Hauschild A, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18(3):404- 412. doi:10.1016/S1470-2045(17)30072-4
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More