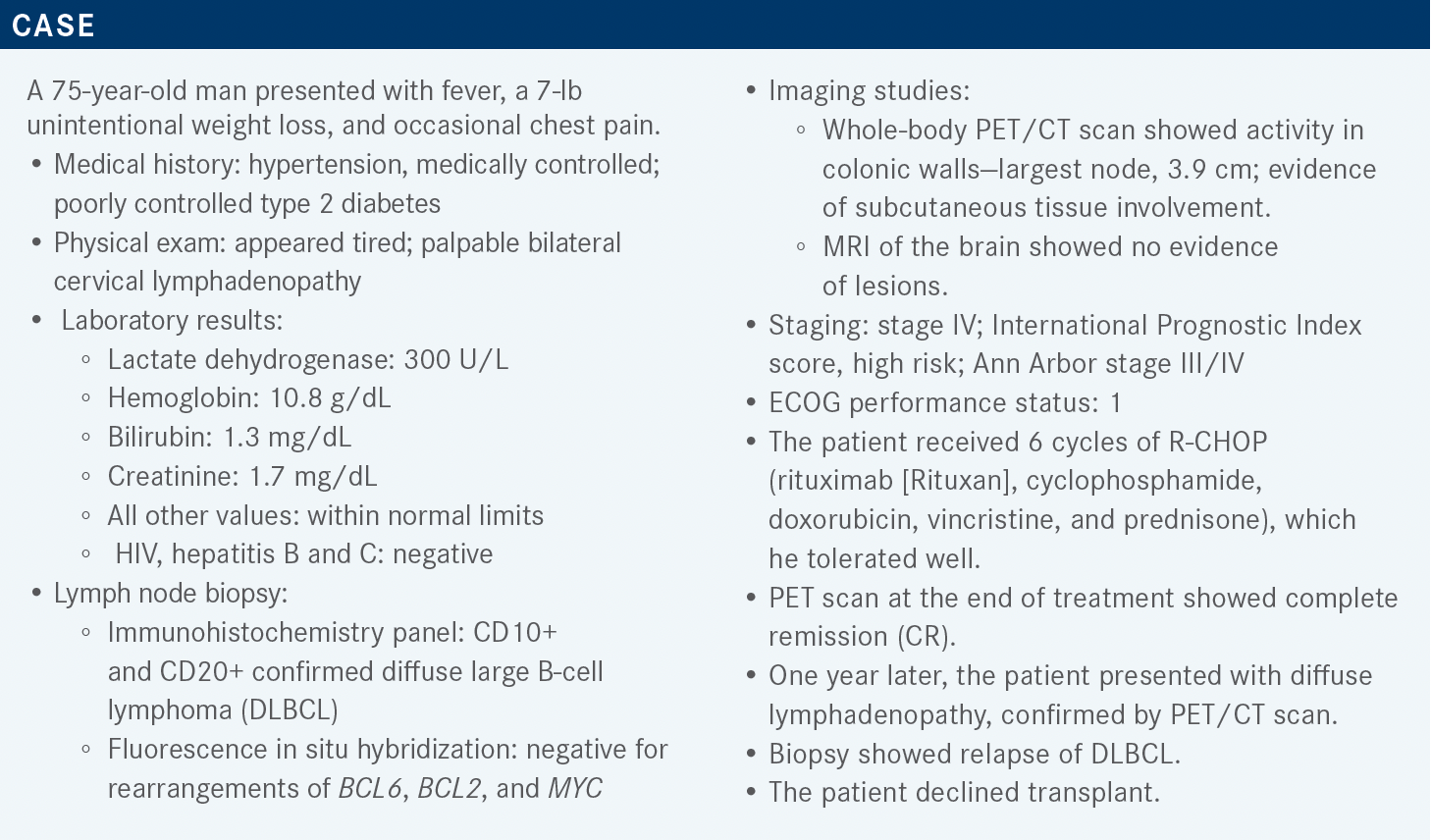
Deciding on Treatment for a Patient With CD10+, CD20+ DLBCL
During a Targeted Oncology case-based roundtable event, John M. Pagel, MD, PhD, discusses the case of a patient with diffuse large B-cell lymphoma who is not eligible for transplant.
John M. Pagel, MD, PhD
Chief of Hematologic Malignancies
Center for Blood Disorders and Stem Cell Transplantation
Swedish Cancer Institute
Seattle, WA

Targeted OncologyTM: What are some options for the second and subsequent lines of therapy in this patient?
PAGEL: The NCCN [National Comprehensive Cancer Network] guidelines break down [therapy for DLBCL] into those for transplant candidates or nontransplant candidates. Our patient in this case is not a transplant candidate. For the second and subsequent lines of therapy, there are some interesting chemotherapy-based regimens that we have a long history with.1
Polatuzumab vedotin [Polivy] plus or minus rituximab and bendamustine [Treanda] is approved by the FDA for patients who have failed 2 or more prior lines of treatment.1 Polatuzumab is an antibody-drug conjugate that targets CD79b on the surface of the B lymphocytes, and delivers a payload, which is the MMAE [monomethyl auristatin E] chemotherapeutic agent, internally to the cell like a smart bomb.
Tafasitamab [Monjuvi], an anti-CD19 antibody plus lenalidomide is also approved by the FDA.2 I think it’s been an exciting regimen, as well, but we understand that it’s only approved for people who are not eligible for transplant for any reason.3 It’s important to remember patient preference can be a reason not to be eligible for transplant. The patient in our case refused the transplant, so it made that part easy.
Other options include lenalidomide [Revlimid] plus rituximab, bendamustine plus rituximab, brentuximab [vedotin; Adcetris] for rare cases of CD30+ DLBCL, and ibrutinib [Imbruvica] for very rare cases of non–germinal center B-cell-like [non-GCB] DLBCL.1
After following up [with] these patients and reassessing for response or progression…the choices are around alternative second-line treatments. [These include] allogeneic transplants or novel therapies such as loncastuximab tesirine [Zynlonta], another antibody-drug conjugate, [and] selinexor [Xpovio], which is approved for people who have failed at least 2 lines of therapy or have progressed on CAR [chimeric antigen receptor] T-cell therapy, which is in fact very much another option too.1
I think it’s important to recognize that we don’t know if targeting CD19 with tafasitamab or loncastuximab, which both of these agents target, has a negative impact on anti-CD19 CAR T-cell treatment. We’re waiting for more data. The early data suggest that maybe it’s not a problem but just something to keep in mind.
What is the mechanism of action for tafasitamab and lenalidomide?
I think [tafasitamab plus lenalidomide] is an interesting regimen. Lenalidomide is not a new drug to anyone and, frankly, you probably know tafasitamab indirectly because it’s an anti-CD19 antibody that just targets a different antigen than rituximab.
There are data that suggest that the combination of these 2 agents works better than if you were to use either of them alone. In other words, they have a synergistic effect. The antibody is, of course, going to work just like rituximab works. You have antibody-dependent cellular cytotoxicity, and phagocytosis. You can have direct apoptosis, as well.
If you understand the management of rituximab, you can understand the management of tafasitamab. One of the nice things about targeting CD19 simply is that it’s not CD20. We give a ton of anti-CD20 antibodies and eventually, it doesn’t work as well for one reason or another. So having a different target is very reasonable. Most know lenalidomide from using it in multiple myeloma. It certainly has immunomodulatory capabilities, such as direct cell death, and activation of those host effector cells that may work well with the antibody. The activity of these agents is potentiated when given together, which has been shown in preclinical models, in vivo and in vitro.
Which data was the approval of combined tafasitamab and lenalidomide based on?
[The combination] was approved based on [findings from] the phase 2 L-MIND trial [NCT02399085].4 We’re looking forward to the confirmatory data, but it was a simple study that used relapsed or refractory patients who had failed 1 to 3 prior therapies. They were not eligible for a transplant. Patients who were refractory to primary therapy were not eligible for the study, but you can imagine that treating them with something different might be very appealing if they’re not going to go for a transplant.
Tafasitamab is an infusion done at 12 mg/kg. You give it weekly for the first 3 cycles. In the first cycle, there’s an additional loading dose on day 4. After cycle 3 up to indefinitely, you deliver the antibody every 2 weeks.3,4 It is combined with lenalidomide for 21 of 28 days at the approved dose of 25 mg daily. The objective response rate [ORR] was the primary end point in this trial. There are longer-term follow-up data of this study, as well, and the data are quite encouraging.4
Many of these patients will require a dose reduction [of lenalidomide] from 25 mg, for reasons I don’t really understand well. Patients with lymphoma tend to not tolerate lenalidomide quite as well as those with multiple myeloma, it seems, so dose reductions happen in about half of patients. It’s not uncommon…to go down to 15 mg and, [although] rarer, down to 10 mg or 5 mg, but it is not particularly common to have to stop therapy due to toxicity.5
In the L-MIND trial, the median age of the patients was 72 and the oldest patient was 76. This is an ideal regimen for older patients. The median number of prior therapies was 2. About 20% are refractory to primary therapy, 44% refractory to their last therapy, [and] 11% failed a prior transplant. Most of these patients didn’t have a known cell of origin, and about [one-fourth] of them had non-GCB DLBCL.5
What was the efficacy in the L–MIND trial?
The data after a follow-up of almost 3 years show the CR rate was outstanding. At 35 months, 32 of the 80 patients were in CR, so 40% of patients [were] having a CR. The ORR in this very difficult high-risk population who cannot get a transplant is also encouraging, at about 46%. Even more encouraging than that is the extended, outstanding median duration of response, with people at well over 43.9 months maintaining their remission and doing very well.5,6
The median progression-free survival [PFS] is about [1 year]. I think that’s extremely encouraging, again, when they’re not transplant candidates. They’ll stay on that every- 2-week antibody infusion for long periods of time. Some of these people are out 2 years or more, doing very well, with a relatively plateaued PFS curve. Maybe some of the people on the overall survival [OS] curve will do well for a long time. The regimen of course is unique but has an outstanding chance to get a CR that might be very durable.
Patients who get CRs do best. A partial remission is certainly better than not having any remission but is certainly very limited. The median duration of remission was about 44 months, …very encouraging in many ways. But how we will use it in the algorithm is something I think we’re still trying to figure out.
Probably, and not surprisingly, [using this regimen] earlier is better than later. So if you only had 1 prior therapy, you have almost a 50% chance of having a CR. If you’ve had 2 or more therapies, it’s about a 1 out of 3 chance of having that kind of remission. Getting a CR is important. Those are the people that have the longest durations of remission. The patients with the longest durations of remissions are the ones that get treated earlier, after 1 prior therapy. Not surprisingly, the median PFS, the earlier [the regimen] was used, was about 2 years, which is outstanding in this patient population, and median OS in these patients is almost 4 years or so.
This is very encouraging for a non–chemotherapy-based regimen in patients who are not transplant candidates because they had comorbidities, or their age or performance status wasn’t adequate, or maybe they didn’t respond to their salvage chemotherapy.
Which toxicities are associated with tafasitamab/ lenalidomide therapy?
You’re going to get some cytopenia due to the lenalidomide. They’re not at all due to the tafasitamab. You manage these just like in multiple myeloma and figure out if you need to go from 25 mg to 20 mg a day, or from 20 mg to 15 mg, because there is a 27% chance of having grade 3 neutropenia. The important point, in my opinion, is that the cytopenia is due to the lenalidomide. So if you’re going to dose reduce, or change anything, you change the lenalidomide. The tafasitamab is never dose reduced because it’s not causing these problems.5
The nonhematologic adverse events [AEs] comprise a long list, but I think one of the things that’s impressive here…is a very low rate of grade 3 or 4 AEs. We saw a little bit of diarrhea, about 30%, and things that go along with lenalidomide such as edema, and perhaps other gastrointestinal issues like constipation as well.
About half of these patients will have to go down to 20 mg. But if you’re at 20 mg, about three-[fourths] of patients will complete the entire 1 year of therapy with lenalidomide.5 So you’re going to do very well with it. Most of these people are going to do, hopefully, very well for a longer time.
Discontinuations to the regimen are about 12%. Most regimens in this patient population and setting have discontinuation rates of around 25% due to AEs.5 So it’s a well-tolerated regimen. The infusion reactions were about 6% to 7%, [which is] not high. If it happens early, it’s managed just like a rituximab reaction.
Tafasitamab plus lenalidomide is given for 1 year with lenalidomide, and then you stop the lenalidomide and continue the tafasitamab every 2 weeks indefinitely. There’s a big difference [between the AES in the first year of therapy and those on the tafasitamab monotherapy thereafter]. To reiterate, the AEs outside of the infusion reactions are due to the lenalidomide.5
How does tafasitamab plus lenalidomide vs lenalidomide alone compare?
The RE-MIND study [NCT04150328] evaluated the combination of the tafasitamab and lenalidomide vs lenalidomide monotherapy. A large [cohort of patients got lenalidomide monotherapy] and 81 patients got tafasitamab plus lenalidomide, but there was no tafasitamab alone cohort. I wish there was and in a perfect world we’d have that, but we don’t. The CR rate in the cohort that [received] tafasitamab plus lenalidomide was about 40%, and it was only about 13% if they received lenalidomide alone.7 We use the [rituximab plus lenalidomide] regimen a lot in indolent lymphomas and this is our equivalent of adding an antibody to lenalidomide in DLBCL. It is a non–chemotherapy-based regimen that clearly has a better ORR, better CRs, and probably even a better OS rate when you look at the combination of tafasitamab and lenalidomide, given its synergistic effects, for people that are not transplant candidates.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 5.2021. Accessed January 25, 2022. https://bit.ly/3geoS5N
2. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed January 25, 2022. https://bit.ly/3bodb9v
3. Monjuvi. Prescribing information. MorphoSys US Inc; 2020. Accessed January 31, 2022. https://bit.ly/2S38ZW7
4. Salles G, Duell J, González Barca E, et al. Primary analysis results of the single-arm phase II study of MOR208 plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma (L-MIND). Hematol Oncol. 2019;37(suppl 2):173-174. doi:10.1002/hon.130_2629
5. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
6. Duell J, Maddocks KJ, González Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/haematol.2020.275958
7. Nowakowski GS,Rodgers TD, Marino D, et al. RE-MIND study: a propensity score-based 1:1 matched comparison of tafasitamab + lenalidomide (L-MIND) versus lenalidomide monotherapy (real-world data) in transplant-ineligible patients with relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL). J Clin Oncol. 2020;38(suppl 15):8020. doi:10.1200/JCO.2020.38.15_suppl.8020