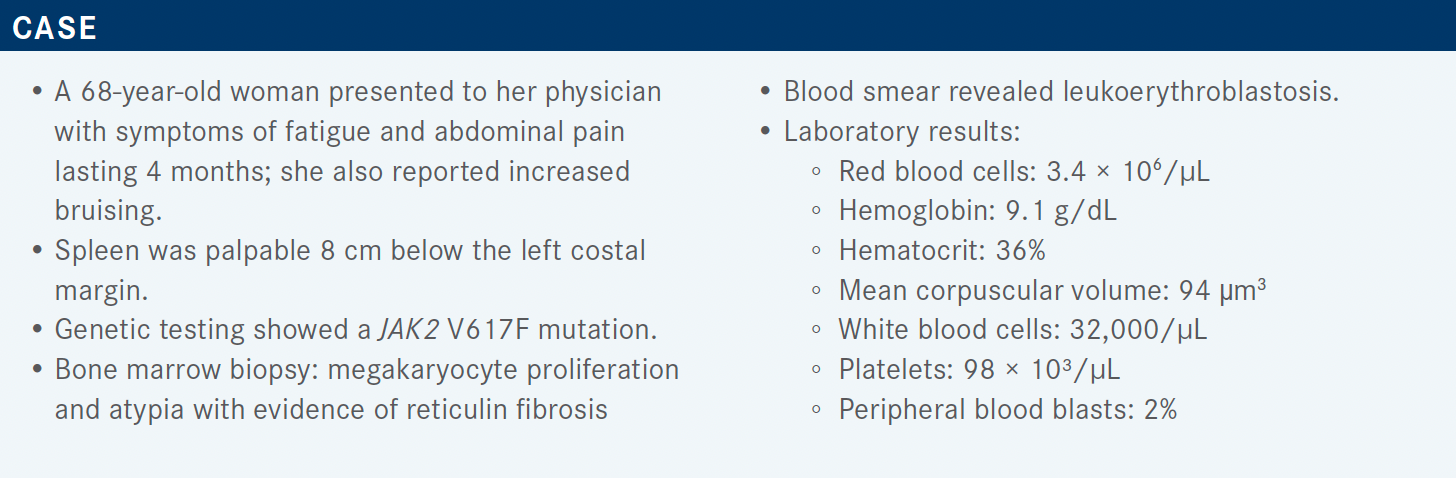
Mesa Considers JAK Inhibition in Myelofibrosis
During a Targeted Oncology case-based roundtable event, Ruben Mesa, MD, discussed risk assessment and management of myeloproliferative neoplasms.
Director
Mays Cancer Center at The University of Texas Health San Antonio
MD Anderson Cancer Center
San Antonio, TX
Targeted OncologyTM: Can you discuss using risk assessment tools in scoring myeloproliferative neoplasms (MPNs)?
MESA: What I tell our fellows is that there’s a prognostic score for every disease [and sometimes] more than one. Clinicians are busy; you’re trying to keep track of many different diseases. It’s impractical to memorize all these things. I think knowing where to find the scores is helpful, but more importantly, in what situation is it the most helpful?
From my end, I always think that it’s interesting to look at what ends up being predictive and what that tells us about the biology of the disease. Because I see a lot of patients with MPNs, but I might also see CML [chronic myeloid leukemia], MDS [myelodysplastic syndrome], AML [acute myeloid leukemia]; and to some degree, a lot of the prognostic features overlap in these diseases. They’re cousins of one another. With worsening cytopenias, moving more toward AML and higher-risk molecular features, it’s only natural that patients have a worse prognostic score.
What about prognostic scoring in myelofibrosis [MF]?
For MF you have the IPSS [International Prognostic Scoring System] and the DIPSS [dynamic IPSS].1-3 The IPSS is at diagnosis; the DIPSS can be used at any time. Practically around the world, the DIPSS and the DIPSS-Plus are used by far the most commonly.3,4 Because with peripheral blood counts and asking [about] symptoms and age you have a rough idea regarding survival, and that can be helpful for separating out the high-risk patients, or likely, the low-risk patients.
The additional molecular mutations are relevant. It doesn’t take away those clinical features, but it’s clearly relevant. These other variables are as follows: 1, if there’s significant fibrosis, and 2, the absence of CALR type 1.5,6 It’s a little awkward way of saying it, but basically being CALR type 1 mutated is more favorable; if they have CALR type 2, they do worse. If you have JAK2 or MPL or if you are lacking any of those driver mutations, you are triple negative. Or if you have a higher-risk molecular feature: ASXL1 is a bad actor, and it’s a bad actor also in MDS; again, it’s telling us something about the biology of the disease. [Additionally, if you have] EZH2, IDH1/2, or SRSF2, or if you have more than 1 of these, [it is a high-risk feature].
The MIPSS70 [mutation-enhanced IPSS 70] can help to separate those patients who have a pretty long survival from the other side, [patients who] might have a very poor survival.5,6
If I’m on the fence about someone—they’re aged 58, they have some mild anemia—this is exactly the sort of patient I’m going to do that extended panel on to try to get a sense of whether we should be thinking about stem cell transplantation. If an individual is aged 79, it’s probably not going to make a big impact one way or the other. There is a second model [MIPSS70-Plus version 2.0].6,7 This is, to some degree, splitting hairs. I think it’s the transplanter who drilled down a bit more into this, to refine that prognosis to the best degree that you can, as they’re trying to factor in who the donor is and what the comorbidities are for the patients. Really, [they are] trying to weigh the risk and benefit of transplant vs no transplant.
Now, the MF secondary to polycythemia vera [PV] and essential thrombocythemia [ET] prognostic model—again, it may seem too much in terms of too many scores—this one is a bit complementary. Patients who had evolved from PV or ET are similar, but not exactly the same, as [those with] primary MF.8 The biggest functional difference is that the blood counts tend to be more preserved in these patients. So, if they had PV before, they tend to become anemic at a lower rate, because there’s still more residual erythrocytosis left in the bone marrow. I’ve had patients who have died of AML, from post-PV MF, who still never became anemic, or still had a hemoglobin of 12 g/dL. It can confound that value.
Likewise, if they have ET, becoming thrombocytopenic sometimes doesn’t occur. There are individuals who have died of MF, with post ET MF, who still had a platelet count of 200,000/μL. Again, they’re not always predictive. So this is helpful, but it’s primarily a refinement for the stem cell transplanter. For physicians, knowing more than the DIPSS and the MIPSS probably doesn’t help your practice to a significant degree.
Is the CALR mutation protective against clots, protective against transformation, or both?
In ET, it is less associated with thrombosis. Now, is it the CALR mutation itself that’s more protective, or is the biology a little different? I don’t think that we know. In MF, it has a longer survival, but it’s not necessarily associated with the issue of thrombosis. So it is helpful for both of those conditions but for slightly different reasons. We may end up finding, in the end, that CALR-mutated disease is similar but is different enough that it should be considered separate. For the time being, we still largely treat them the same but factor in a prognostic score.
What about the National Comprehensive Cancer Network (NCCN) guidelines for MF?
For the NCCN guidelines, I was the initial panel chair. It’s now fallen to my colleague Aaron Gerds, MD, MS. But they decided, and I think wisely so, that with all these scores, functionally, it probably doesn’t have implications for therapy beyond stratifying patients into lower risk or higher risk [groups].9
In higher risk, which fits this patient, we assess symptoms but we stratify the treatment in part on platelets. So first we determine, are they a transplant candidate or not a transplant candidate? If they’re a transplant candidate, we certainly consider moving toward a transplant.
Now usually [this is] in concert with starting them on medical therapy. Initially, we have questions such as is it safe to use a JAK inhibitor before transplant? Largely, we have found that is the case. We also have found that the outcome with transplant is probably best if they have the transplant while they’re optimally responding to a JAK inhibitor. If we wait until they’re on a JAK inhibitor and progress, if they’ve failed it, particularly if they’ve moved to acute leukemia, the outcomes are worse. I try to share with my patients, “The optimal time for transplant is probably a bit before you feel that you need one.” Because if we’re using it as a salvage therapy, the outcomes are probably a bit poorer.
All of that said, probably less than 10% of patients with MF in the United States [receive] a transplant. That’s due to age, choice, a range of factors. The majority in the United States receive ruxolitinib [Jakafi]. Fedratinib [Inrebic] is now approved in the frontline setting.10 Not many have used it in that setting, but it is approved and there are circumstances when to consider it. It probably is more commonly used in the second-line setting, and that is approved as well.
Can you give more detail about ruxolitinib?
Now ruxolitinib, it’s almost a decade that it has been around, [as seen in the] New England Journal of Medicine studies that were published long ago: ruxolitinib vs placebo, or ruxolitinib vs best alternative therapy.11,12 It was shown to be very helpful for improvement in the spleen and the control of symptoms.
We have used it over this period of time. Sometimes, the effect can be quite dramatic. I’d say because of the availability of this we tend to see [fewer] patients now with these extreme presentations, because they usually have already been treated. But there was—I think pre-2007, pre–JAK inhibitor—a time when we had patients with gargantuan spleens and cachectic patients. That still occurs, but fortunately that occurs in fewer patients.
There clearly can be improvement in symptoms. Patients with MF can be quite symptomatic….Symptoms include fatigue, night sweats, weight loss.11 There can be some symptoms related to the spleen, some that are hypercatabolic and some that are associated with progressive disease.
With other patient-reported outcome metrics, ruxolitinib showed improvement in quality of life, as well as global health status.12
Now over time, I think we have been able to answer the question, “Is there an impact on survival?” The studies were not survival studies because of many reasons, starting with the impractical nature of keeping [participants] on a control arm indefinitely with a drug that made a difference. But there are now many real-world analysis data, as well as long-term follow-up from the trials accounting for crossover, as well as other pieces, suggesting that there is an improvement in survival.13 It’s not a cure; the survival curves do not plateau.
Why do you think patients live longer when receiving ruxolitinib?
I think it’s a range of things. There may be less inflammation in the bone marrow, less drive toward progression, toward acute leukemia.2,13 I think there is less debilitation. All of these things play a factor. But in caring for hundreds to thousands of patients with MF, without question [I’ve seen that] these patients are living longer. I have some patients who are still alive from 2007 who [previously might have died] in 2 to 3 years, so there are some extremely long-lived patients. The average is less; I think the impact is real, but it is finite.
What we have learned over time is that—and it’s probably not a surprise—survival is associated with the quality of their response and the degree of improvement in the spleen correlates with survival.14-16 I don’t think that it’s a mechanical thing, meaning that it’s because the spleen shrank that they lived longer. I think whatever is associated with JAK inhibitor–treated patients living longer corresponds to the improvement in the size of the spleen.
Is that cytokine driven? Is that improvement in the inflammatory microenvironment in the bone marrow? Whatever that is, I think there’s a correlation but I don’t think that it’s just about the spleen.
How is ruxolitinib dosed for patients? What is the safety profile?
One thing we have learned over time is that we probably have grown a bit too conservative in terms of the dosing. Doses below 10 mg twice daily probably don’t have a significant impact on the splenomegaly, and probably don’t have a huge impact on survival. There is probably some value to trying to get patients to 15 mg twice daily or, in certain circumstances, even 20 mg twice daily.17 If they’re anemic, I tend to be patient. If they need a transfusion or 2, I warn them that that is a possibility up front.
I think over time we’ve done a variety of analyses, and it probably is worthwhile to hold the dose steady and support them during that time. In terms of toxicities, in JAK inhibition—the creation of red cells and platelets both go through the JAK/STAT pathway. So it was predictable from the beginning, that lowering red cells and platelets would be, not even a toxicity, just a predicted effect based on the mechanism of action. The DLT [dose-limiting toxicity] was clearly platelet-[related].11,12 Neutropenia is quite uncommon.
There have been studies looking at, for patients with lower platelets, what is the best approach.18,19 There are increasing data suggesting it’s OK to start them low but push the dose. If a patient has 60,000 platelets, it’s OK to start them on 5 mg twice a day. But they’re not stuck at that dose.
The likelihood of, once they’re on a JAK inhibitor, having a big drop in their platelets as a secondary effect is probably less. So they were able to take [patients] who started with platelets of 50,000 to 74,000, or 75,000 to 100,000, and get them to 15 mg twice a day. Not at first, but they walked the dose up, and that probably is a bit more effective dosing for these patients.
Now with these patients, they started with thrombocytopenia. Interestingly, for the patients with platelets of 50,000 to 74,000, further decreases from baseline really weren’t very high.19 It’s been my experience that the lower the platelet count, probably the less the delta. I have started patients on 5 mg twice a day who have a platelet count of 40,000, but it’s not like they dropped to 5000. They’ll drop to 32,000. Whereas, if you start somebody at 300,000, yes, they may drop to 150,000. What we don’t tend to see is JAK inhibitors causing platelet counts of under 10,000 or having patients hemorrhage. So there can be thrombocytopenia, but it’s a little different from a straight myelosuppressive effect.
What are the data for fedratinib in this setting?
Fedratinib…is a JAK2 and FLT3 inhibitor. It was approved in September 2019, so just a little bit before the COVID-19 pandemic started.10 [The approval was] based on the randomized phase 3 JAKARTA study [NCT01437787], which was fedratinib vs placebo. It very much was a contemporary of ruxolitinib.20,21 It was not compared against ruxolitinib because it was tested somewhat in parallel, perhaps just a little bit further behind, but this study started before ruxolitinib was approved.
Very much like ruxolitinib, there was good improvement in splenomegaly and symptoms.20-22 There was efficacy both for individuals with a platelet count above 100,000, as well as from 50,000 to 100,000. In terms of toxicity, the potential for cytopenias is relatively similar to that of ruxolitinib.21 It can cause gastrointestinal adverse events. Having used it in a range of patients [throughout Texas], I tend to start prophylactic medication; many patients are able to come off of these. The medicine has a black box warning for Wernicke encephalopathy, which is very rare—in the clinical trials, which had led to a hold—less than a 1% rate. It may interfere a bit with thiamine metabolism. Subsequent to that hold, now, with the black box warning, we screen for thiamine and we replace thiamine.
Thiamine is easy to give, it’s [inexpensive]; I pretty much put all my patients on it who go on the medicine; they are screened for this. We’ve not seen that it’s been an issue after its approval, with monitoring for thiamine. So it’s something to be aware of, but functionally not a big deal.
A jug of 100 thiamine [tablets], when I went down to the pharmacy, was less than 10 dollars. About Wernicke encephalopathy: There is less than a 1% absolute risk, and [it is] something that shouldn’t be viewed as an excessive barrier.23 Give them some thiamine, measure the level, track it, but it’s not too big a factor.
What do you think about using fedratinib for patients with MPNs?
Fedratinib is a good drug….It’s a drug a lot of people aren’t super familiar with. In part, with COVID-19 and everything else, we’ve not been at the American Society of Hematology annual meeting and…have heard about it less. There was a delay between its phase 3 studies and its approval. So a lot of the things that usually build momentum in terms of usage weren’t there.
We can see some nice responses in the second-line setting. I think for most who are pretty comfortable with ruxolitinib, the second-line setting is the most natural. I’d say I had [approximately] 10 to 15 patients during COVID-19 [for whom] I would have normally considered a clinical trial, [but] putting them on a clinical trial was impractical. They didn’t want to come down from Dallas or somewhere else if they needed a second-line therapy. So we used fedratinib and got some good responses. Patients can tolerate it. It’s a good thing to consider in the second-line setting, particularly if traveling for a clinical trial is not attractive.
Just going back to the NCCN treatment algorithm, no response or loss of response to that initial JAK inhibitor therapy is where an alternative JAK inhibitor may be considered. [And that], at this point, is fedratinib.9 [For patients with] platelets of less than 50,000, “not a transplant candidate” equals “consider clinical trial.” It is possible that soon we may see a third JAK inhibitor, pacritinib, approved. That has been tested in individuals with a platelet count less than 50,000 and was helpful. So there may be a new option for those individuals in the frontline or second-line setting who have marked thrombocytopenia.
REFERENCES
1. Bose P, Verstovsek S. The evolution and clinical relevance of prognostic classification systems in myelofi brosis. Cancer. 2016;122(5):681-692. doi:10.1002/cncr.29842
2. Cervantes F, Dupriez B, Pereira A, et al. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood. 2009;113(13):2895-901. doi:10.1182/blood-2008-07-170449
3. Passamonti F, Cervantes F, Vannucchi AM, et al. A dynamic prognostic model to predict survival in primary myelofibrosis: a study by the IWG-MRT (International Working Group for Myeloproliferative Neoplasms Research and Treatment). Blood. 2010;115(9):1703-1708. doi:10.1182/blood-2009-09-245837
4. Gangat N, Caramazza D, Vaidya R, et al. DIPSS plus: a refined Dynamic International Prognostic Scoring System for primary myelofibrosis that incorporates prognostic information from karyotype, platelet count, and transfusion status. J Clin Oncol. 2011;29(4):392-397. doi:10.1200/JCO.2010.32.2446
5. Guglielmelli P, Lasho TL, Rotunno G, et al. MIPSS70: Mutation-Enhanced International Prognostic Score System for transplantation-age patients with primary myelofibrosis. J Clin Oncol. 2018;36(4):310-318. doi:10.1200/JCO.2017.76.4886
6. Tefferi A, Nicolosi M, Mudireddy M, et al. Revised cytogenetic risk stratification in primary myelofibrosis: analysis based on 1002 informative patients. Leukemia. 2018;32(5):1189-1199. doi:10.1038/s41375-018-0018-z
7. Tefferi A, Guglielmelli P, Lasho TL, et al. MIPSS70+ version 2.0: Mutation and Karyotype-Enhanced International Prognostic Scoring System for primary myelofibrosis. J Clin Oncol. 2018;36(17):1769-1770. doi:10.1200/JCO.2018.78.9867
8. Passamonti F, Giorgino T, Mora B, et al. A clinical-molecular prognostic model to predict survival in patients with post polycythemia vera and post essential thrombocythemia myelofibrosis. Leukemia. 2017;31(12):2726-2731. doi:10.1038/leu.2017.169
9. NCCN. Clinical Practice Guidelines in Oncology. Myeloproliferative neoplasms, version 2.2021. Accessed January 31, 2022. https://bit.ly/3geJd9T
10. FDA approves fedratinib for myelofibrosis. FDA. Updated August 16, 2019. Accessed January 31, 2022. https://bit.ly/3dErcBr
11. Verstovsek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366(9):799-807. doi:10.1056/NEJMoa1110557
12. Harrison C, Kiladjian JJ, Al-Ali HK, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366(9):787-798. doi:10.1056/NEJMoa1110556
13. Verstovsek S, Gotlib J, Mesa RA, et al. Long-term survival in patients treated with ruxolitinib for myelofibrosis: COMFORT-I and -II pooled analyses. J Hematol Oncol. 2017;10(1):156. doi:10.1186/s13045-017-0527-7
14. Palandri F, Palumbo GA, Bonifacio M, et al. Durability of spleen response affects the outcome of ruxolitinib-treated patients with myelofibrosis: results from a multicentre study on 284 patients. Leuk Res. 2018;74:86-88. doi:10.1016/j.leukres.2018.10.001
15. Palandri F, Palumbo GA, Bonifacio M, et al. Baseline factors associated with response to ruxolitinib: an independent study on 408 patients with myelofibrosis. Oncotarget. 2017;8(45):79073-79086. doi:10.18632/oncotarget.18674
16. Menghrajani K, Boonstra PS, Mercer JA, et al. Predictive models for splenic response to JAK-inhibitor therapy in patients with myelofibrosis. Leuk Lymphoma. 2019;60(4):1036-1042. doi:10.1080/10428194.2018.1509315
17. Verstovsek S, Gotlib J, Gupta V, et al. Management of cytopenias in patients with myelofibrosis treated with ruxolitinib and effect of dose modifications on efficacy outcomes. Onco Targets Ther. 2013;7:13-21. doi:10.2147/OTT.S53348
18. Vannucchi AM, Te Boekhorst PAW, Harrison CN, et al. EXPAND, a dose-finding study of ruxolitinib in patients with myelofibrosis and low platelet counts: 48-week follow-up analysis. Haematologica. 2019;104(5):947-954. doi:10.3324/haematol.2018.204602
19. Guglielmelli P, Kiladjian J, Vannucchi AM, et al. The final analysis of EXPAND: a phase 1b, open-label, dose-finding study of ruxolitinib (RUX) in patients (pts) with myelofibrosis (MF) and low platelet (plt) count (50 × 109/L to < 100 × 109/L) at baseline. Blood. 2020;136(suppl 1):4-5. doi:10.1182/blood-2020-137742
20. Pardanani A, Harrison C, Cortes JE, et al. Safety and efficacy of fedratinib in patients with primary or secondary myelofibrosis: a randomized clinical trial. JAMA Oncol. 2015;1(5):643-651. doi:10.1001/jamaoncol.2015.1590
21. Pardanani A, Tefferi A, Masszi T, et al. Updated results of the placebo-controlled, phase III JAKARTA trial of fedratinib in patients with intermediate-2 or high-risk myelofibrosis. Br J Haematol. 2021;195(2):244-248. doi:10.1111/bjh.17727
22. Harrison C, Schaap N, Vannucchi AM, et al. Fedratinib induces spleen responses and reduces symptom burden in patients with myeloproliferative neoplasm (MPN)-associated myelofibrosis (MF) and low platelet counts, who were either ruxolitinib-naïve or were previously treated with ruxolitinib. Blood. 2019;134(suppl 1):668. doi:10.1182/blood-2019-129288
23. Inrebic. Prescribing information. Bristol Myers Squibb; 2019. Accessed January 31, 2022. https://bit.ly/3Ha4CwO