Patients With Thyroid Carcinoma Respond to Multikinase Inhibitors After Disease Progression
The DECISION and SELECT studies provide evidence of response to multikinase inhibitors after disease progression in patients with thyroid carcinoma.
Misagh Karimi, MD

During a Targeted Oncology Case-Based Roundtable event, Misagh Karimi, MD, an assistant clinical professor in the Department of Medical Oncology & Therapeutics Research at City of Hope, discussed the studies praround the use of multikinase inhibitors after disease progression in patients with thyroid carcinoma.
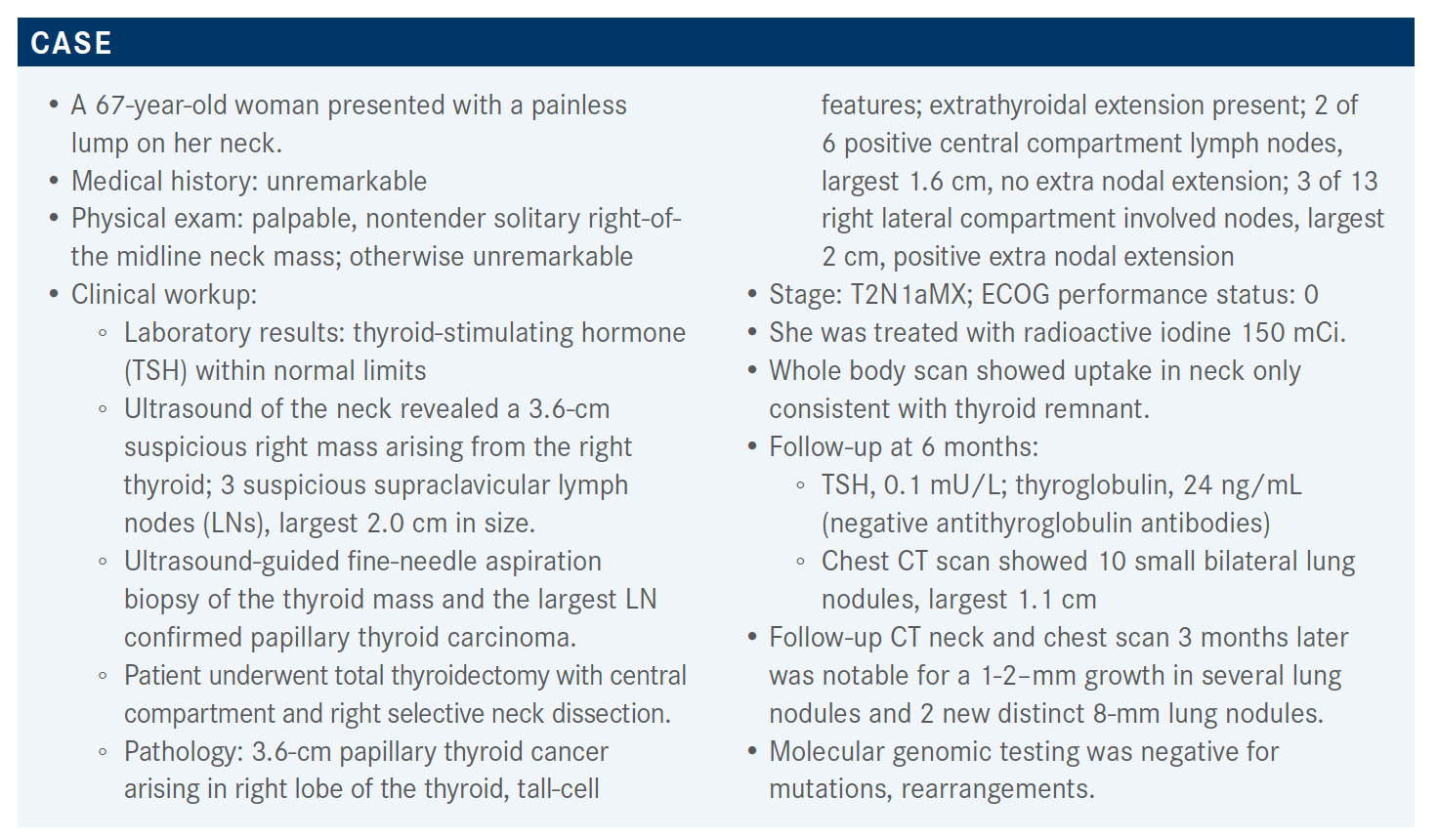
Targeted OncologyTM: What are the guidelines for treatment with a patient like this?
KARIMI: Looking at metastatic disease, the National Comprehensive Cancer Network [NCCN] guidelines suggest lenvatinib [Lenvima] as preferred [treatment] as it is more efficacious, but sorafenib [Nexavar] is another option.1 When we talk about the NGS [next generation sequencing], if patients have NTRK [gene fusion], then they would qualify for the targeted treatment. If they have a [tumor with a] RET fusion, other drugs that have recently been approved include selpercatinib [Retevmo].
Immunotherapy [is used] for patients who have a high TMB [tumor mutation burden], so that’s also something that has been shown to be effective. For patients who have resectable disease, that’s definitely an option. The radiotherapy may be reserved for patients who have symptomatic sites, and that could be used if they’re not responding to systemic therapy.
Please provide an overview of the DECISION (NCT00984282) study.
[This study] looks at sorafenib versus placebo in patients who have locally advanced or metastatic disease, are radioiodine refractory, who have recently progressed, and had no prior chemotherapy or targeted therapy. Sorafenib was given 400 mg twice a day, [and patients were] randomized 1:1 in each arm. The primary end point was progression-free survival [PFS].2
The difference [in PFS between the treatment arm and placebo arm] had a hazard ratio of 0.59 [95% CI, 0.45- 0.76, P < .0001]. In the objective response rates [ORRs], the difference was 12% versus 0.5% on placebo. That was highly statistically significant, but overall survival [OS] was not reached. So, there’s no difference at this point that we’re aware of.
Of course, the other side of the coin is the toxicity, and with sorafenib there was significant dose interruption [in 66.2%] and dose reductions [in 64.3%], and then withdrawal was about 19%. There was some treatment-emergent death, but probably the biggest issue here is the hand-foot syndrome, [which was] the most common reason for sorafenib dose interruption, reduction, and withdrawals. Hand-foot syndrome is the most common [with 76.3% of patients experiencing it at any grade] and then diarrhea. Grade 3 adverse events [AEs] was what patients would suffer from and the reported hand-foot syndrome was 42% for grade 3.
What were the design and efficacy outcomes of the SELECT (NCT01321554) trial?
This was a double-blind study randomized 1:1 to lenvatinib versus placebo and they did allow crossover for patients who had placebo then had [disease] progression.3 Patients [included on the trial] had evidence of progression, were refractory to iodine, measurable disease, and they allowed up to 1 prior TKI [tyrosine kinase inhibitor] for this trial. The lenvatinib dose was 24 mg daily and the primary end point was PFS, then secondary end points included ORR, OS, and safety.
Median PFS was 19.4 months versus 3.7 months, significant statistically with a hazard ratio of 0.24 [99% CI, 0.17-0.35, P < .0001]. It’s difficult that we don’t have the head-to-head trials, but there was a significant difference here that seems to be more pronounced, and that’s the reason that NCCN has lenvatinib as the preferred agent.
What was the safety profile of lenvatinib in this patient population?
Six fatalities reported were thought to be related to the lenvatinib arm including pulmonary embolism, hemorrhagic stroke, general deterioration, and 3 cases were reported as death or sudden death. We have to keep that in mind when we’re recommending treatment for these patients.
I think most of oncologists have used lenvatinib [and expect] hypertension, [which was] pretty high on the list [at 67.8% at all grades]. Diarrhea, fatigue, decreased appetite, decreased weight, and nausea [were also high on the list of common AEs]. Those were the main ones, and the hand-foot syndrome in this case was not [most common]. The grade 3 [cases of it] was 3.4% and that’s probably the biggest differentiating factor for patients who get hand-foot syndrome. I think a lot of [patients] experienced it when sorafenib and sunitinib [Sutent] came out; we saw the difference in hand-foot syndrome.
How does the patient’s age impact their PFS?
Both [patients older and younger than 65 years old] benefitted from lenvatinib. For PFS, there was a significant difference in hazard ratio in both age groups, 0.19 [95% CI, 0.13-0.27, P < .001] and 0.27 [95% CI, 0.17-0.43, P < .001], respectively.4 That’s why it is recommended. We see more toxicity in the older patients, but we still see benefit even when we have to dose reduce.
What’s interesting here is the OS. There’s speculation as to why the OS is different for the older patients. It’s in favor [of the older population], the agent compared with placebo, but in the younger patient it isn’t. The speculation was that maybe it’s a smaller number of patients than the younger patients. Or maybe older patients just don’t have enough reserve and they tend to succumb to issues that come up from the cancer faster compared with younger patients who tend to live longer and are able to compensate for the issues that come up. That’s a pretty interesting discussion. We saw the significance in PFS, there was no question there.
Does the size of the tumor affect outcome, or does it affect your decisions regarding starting treatment?
Looking at OS and PFS by lung metastases, they are [both] better for metastases less than 1 cm, and favoring lenvatinib in the study regardless of size.5 The survival was a little bit different. For patients who have metastases above 2 cm, that’s expected. The median survival was a bit lower compared with the patients who have smaller size on the study. That also, looking at PFS, similar issue. With the PFS, there was much more benefit in general.
What dose do you believe patients like this should start on?
The SELECT study started with 24 mg of lenvatinib.6 This is a phase 2 trial trying to figure out what dose would be good in radioiodine-refractory disease, and they tried 18 mg versus 24 mg; 152 patients were randomized to receive those 2 doses. The primary end points were overall response rate at 24 weeks and improved safety.
The results—we would have liked to see that 18 mg would be as good, but noninferiority was not demonstrated. So, you couldn’t really say 18 mg was as good as 24 mg, and that’s the reason that 24 mg is the recommended dose for treatment. Interestingly, they reported similar incidences of grade 3 and 4 AEs between the 2 doses which is pretty interesting.
References:
1. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 2.2020. Accessed April 9, 2021. https://bit.ly/2TCNGIq
2. Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet. 2014;384(9940):319-328. doi:10.1016/ S0140-6736(14)60421-9
3. Schlumberger M, Tahara M, Wirth LJ, et al. Lenvatinib versus placebo in radioiodine-refractory thyroid cancer. N Engl J Med. 2015;372(7):621-630. doi:10.1056/ NEJMoa1406470
4. Brose MS, Worden FP, Newbold KL, Guo M, Hurria A. Effect of age on the efficacy and safety of lenvatinib in radioiodine-refractory differentiated thyroid cancer in the phase III SELECT trial. J Clin Oncol. 2017;35(23):2692-2699. doi:10.1200/ JCO.2016.71.6472
5. Tahara M, Kiyota N, Hoff AO, et al. Impact of lung metastasis on overall survival (OS) in the phase 3 SELECT study with lenvatinib (LEN) in patients (pts) with radioiodine refractory differentiated thyroid cancer (RR-DTC). Ann Oncol. 2019;30(suppl 5):v756-v759. doi:10.1093/annonc/mdz267
6. Eisai announces topline results from Study 211 supporting 24 mg as the appropriate starting dose for Lenvima (lenvatinib) in patients with differentiated thyroid cancer. News release. Eisai, Inc; August 11, 2020. Accessed April 9, 2021. https://bit.ly/3ixG6Jn

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen