Oncologists Scramble to Shift Resources, Develop New Protocols in Response to Novel Coronavirus
From reprioritizing office visits to rescheduling surgical procedures and even delaying clinical trials, coronavirus disease 2019 has affected every facet of life on a global scale. Oncologists who are already challenged to keep their patients healthy from more run-off-the-mill infections must now contend with a new pathogen.

From reprioritizing office visits to rescheduling surgical procedures and even delaying clinical trials, coronavirus disease 2019 (COVID-19) has affected every facet of life on a global scale. Oncologists who are already challenged to keep their patients healthy from more run-off-the-mill infections must now contend with a new pathogen
In the face of this pandemic, community oncologists, advanced practice nurses, and a host of health care providers on the frontlines of patient care remain resolved to deliver the best care possible. As a result, day-to-day practices have been altered, but patients with cancer still need to receive necessary care, and clinical trials are ongoing.
“Cancer is not waiting or stopping because of this virus; it is still there, and it is still an issue,” Andrew M. Evens, DO, MSc, director of the lymphoma program and associate director of clinical services at Rutgers Cancer Institute of New Jersey in New Brunswick, said in an interview with Targeted Therapies in Oncology(TTO).
“We have patients still being diagnosed with influenza, so COVID-19 is an extra infection that we have to be cognizant and mindful of.”
Impact on Oncology
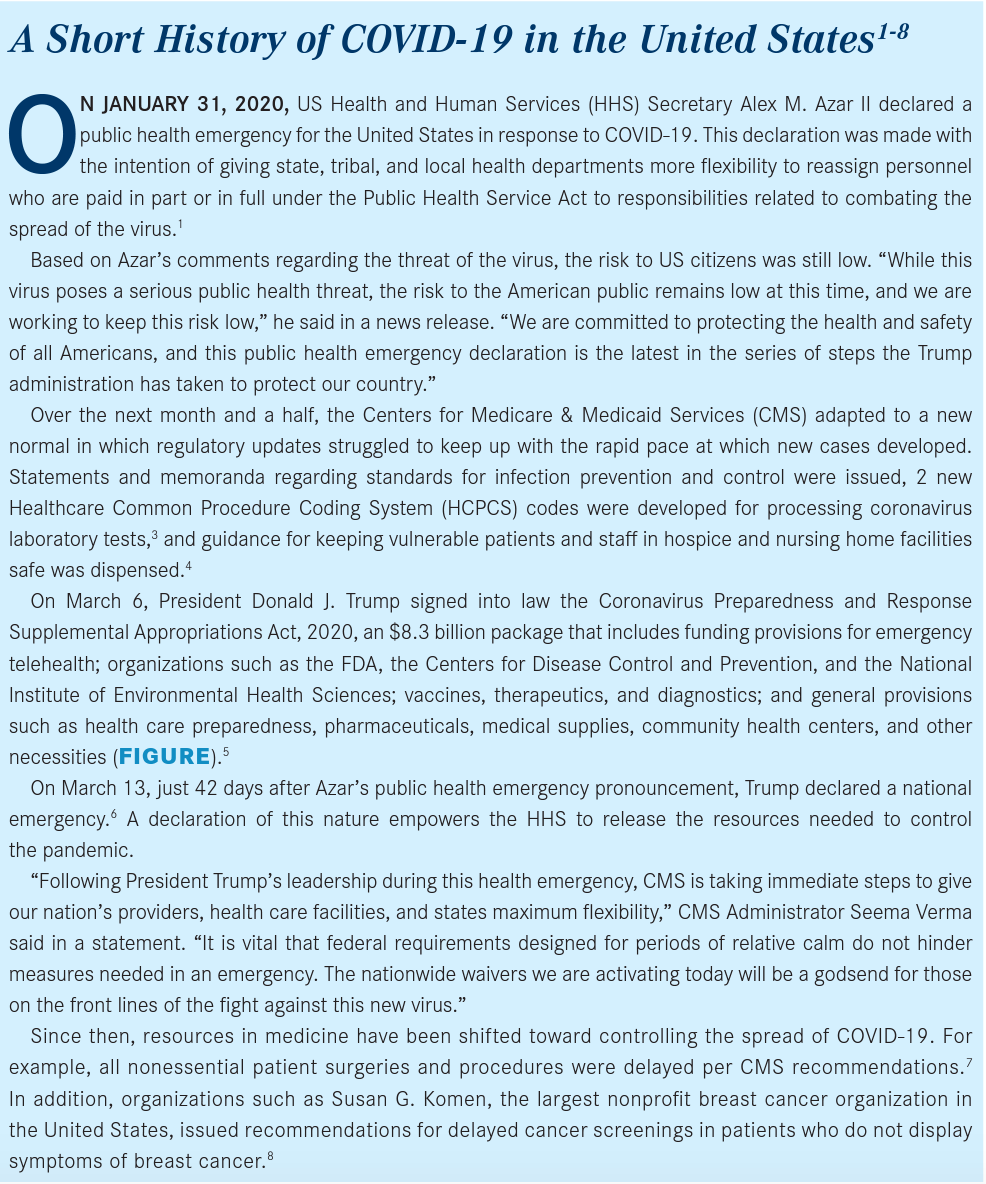
By late March 2020, every US state had confirmed patient cases of COVID-19, but testing and treatment strategiesespecially for patients with malignancies— are still emerging. The sidebar, “A Short History of COVID-19 in the United States,” reviews in more detail the emergence of the virus in our country.1-8
The growing concern regarding the spread of COVID-19 has had heavy effects on the oncology community. In large part, this is due to the outsize number of patients who are immune compromised such as the elderly and those who are actively receiving chemotherapy and/or immunotherapy that affects the ability to fight infections.
Although patients are receiving treatment as necessary and clinical trials continue, precautions have been taken and will continued to evolve, with the safety of patients, providers, and the general public as the top priority.
Real-Life Experience Treating COVID-19
Limited peer-reviewed research is available to describe the effects of the virus on patients with cancer, due in large part to the rapidity at which the novel virus has spread.9
In an analysis of 2007 cases of COVID-19 throughout China, investigators aimed to determine the effect of the virus, specifically on patients with a history of cancer. Of 1590 patients analyzed, 18 had a history of cancer (1%; 95% CI, 0.61%-1.65%). Lung cancer was the most frequent malignancy, accounting for 5 cases (28%). Twenty-five percent of patients with known treatment status had received chemotherapy or surgery within the past month, and the rest were cancer survivors in routine follow-up after primary resection.10
Compared with patients without cancer, patients in this group were older, were more likely to have a history of smoking or polypnea, and had more severe baseline computed tomography manifestations. Patients with cancer were at higher risk of severe events (39%) compared with those without cancer (8%; Fisher exact testP= .0008).
Based on these results, the investigators concluded that patients with cancer may be at higher risk of contracting COVID-19 than other individuals. Major strategies proposed for this group include postponing adjuvant chemotherapy or elective surgery in patients with stable disease who are currently in endemic areas; stronger personal protection provisions; and more intensive surveillance and treatment, especially in older patients and those with comorbidities.
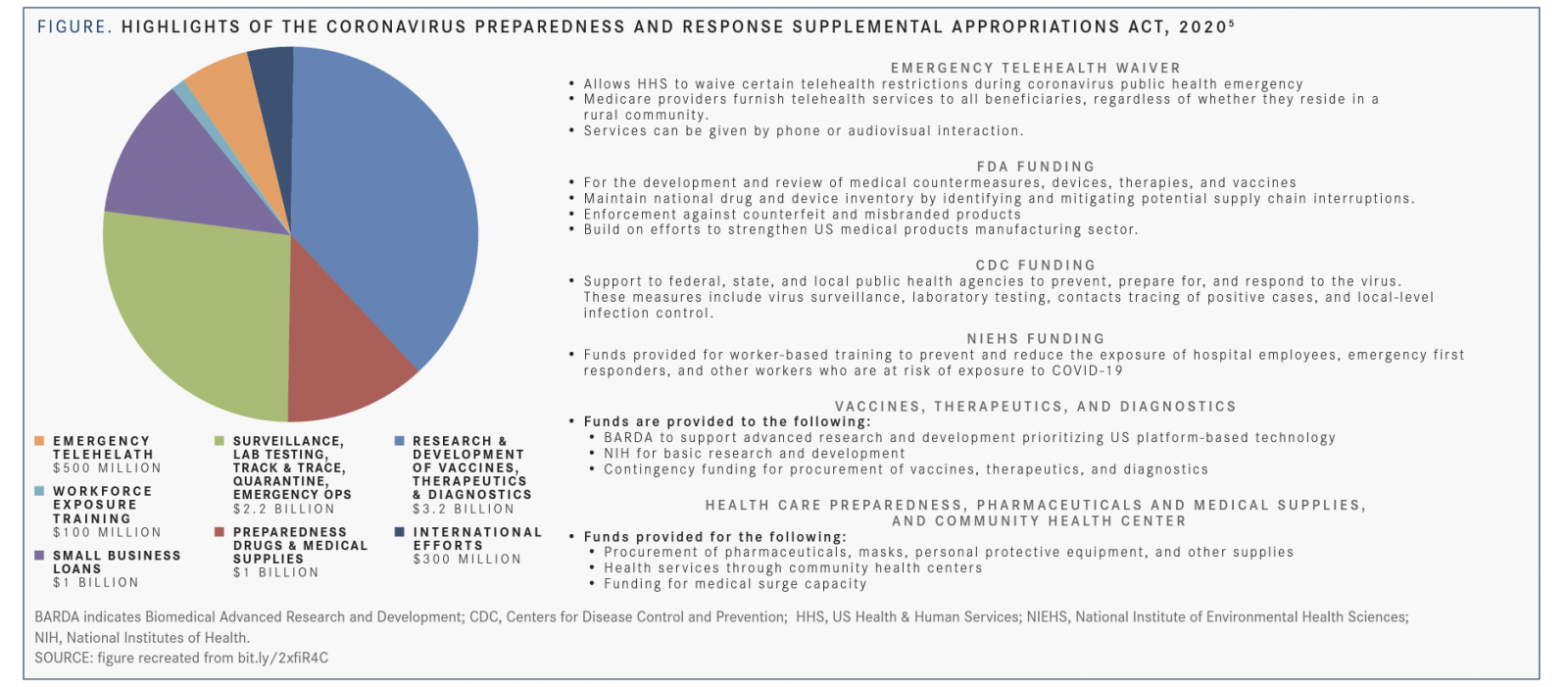
One report published in theJournal of Thoracic Oncologydetailed the clinical presentation of 2 patients who underwent lung lobectomies for adenocarcinoma and were retrospectively found to test positive for COVID-19 at the time of procedure. Both patients exhibited edema, proteinaceous exudate, focal reactive hyperplasia of pneumocytes with patchy cellular infiltration, and multinucleated giant cells (TABLE).9
“This is the first study to describe the pathology of disease caused by COVID-19 pneumonia since no autopsies or biopsies had been performed thus far,” Shu-Yuan Xiao, MD, of the department of pathology at Zhongnan Hospital of Wuhan University in China and a coauthor of the study, commented when discussing the findings.11
Logistics for Practicing Oncologists
Evens discussed how the new precautions are changing the way he treats patients in the clinic. “Even before COVID-19, we have always had significant concern about the risk of patients with cancer contracting an infectionin particular, those patients on active treatment, and especially if they are receiving strong chemotherapies where their immune system could be compromised,” Evens said. “With COVID-19, we are not sure if there is a higher risk of contracting an infection, but if your immune system is compromised and you happen to contract an infection, it can be more severe.”
For general patient care recommendations, the American Society of Clinical Oncology (ASCO) encouraged oncologists to follow CDC guidance where possible regarding general health care facilities. Additionally, the organization said that patients should be informed about symptoms of COVID-19, be trained on proper handwashing and hygiene, and minimize exposure to sick contacts and large crowds. Comprehensive evaluation of any patient with a fever or other symptoms should be performed as per usual medical practice.12
“The focus should be on education [concerning] what is going on with the virus but also regarding the needed precautions,” Evens said. “Social distancing and other standing ramifications [are important considerations about] not only contracting but potentially spreading this virus, as well as other infections.”
At this time, there is no guidance for delaying or discontinuing potentially immunosuppressive therapy; however, certain patients in remission who have the option to stop maintenance therapy or those capable of switching to oral chemotherapeutics may choose to do so. ASCO pointed out that oral chemotherapeutics have the advantage of reducing clinic visits but require greater vigilance by the administering health care team to ensure that patients are taking their medications correctly. Other recommendations include dose delay if local transmission affects a particular cancer center or arranging for patients to receive care at another facility.12
“We do not want people to overreact, especially if they have a treatable and curable,” Evens said. “We do not want somebody with a potentially treatable and curable cancer to forgo therapy out of fear of this situation.”
For patients at high risk of contracting COVID-19, ASCO does recommend delaying planned allogeneic stem cell transplantation, particularly in those with malignancies that are well controlled with conventional treatment.
“There is not an overarching or one-size-fits-all treatment policy. It depends on the individual patient, what type of cancer they have, the type of treatment they are receiving, and if it’s a cancer [for which treatment] could potentially be delayed,” Evens said. “If it is a cancer that is life-threatening [but also] treatable and curable, we need to stay on schedule. At the end of the day, it becomes individualized.”
Clinical Trial Participation and Enrollment On March 18, the FDA issued guidance regarding conducting clinical trials during the COVID-19 pandemic because of the added obstacles that may affect trial protocols.13Interim guidance for amending protocols and practices to investigational and noninvestigational new drug trials was also released by the National Cancer Institute (NCI) Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).14
“The clinical trials process, by its nature, builds in an abundance of caution,” Randall A. Oyer, MD, medical director of the Ann B. Barshinger Cancer Institute of Penn Medicine Lancaster General Health in Pennsylvania and current president of the Association of Community Cancer Centers (ACCC), said in an interview with TTO. “We have had communications from the NCI and NCORP, from the cooperative groups, from our industry trial sponsors, and from in-house investigator-led trials…to continue [to treat] patients on essential clinical trials, especially those who have the clear prospect of directly benefiting from the trial.”
Based on FDA guidance, trial sponsors are encouraged to consider the safety of each individual patient when making a determination regarding recruitment, continued participation, and drug administration. Changes to trials may vary based on factors such as the disease being studied, the drug being administered, disruptions or changes to the agent’s supply chain, and the region in which the trial is being conducted.13
Protocol changes, if undertaken, must be documented and explain how the change affects furnishing of patients’ safety needs. Sponsors are urged to consult institutional review boards and independent ethics committees regarding changes to a clinical trial, especially those related to efficacy end points. Lifesaving measures can be implemented without prior approval but should be documented and reported.13
“At my organization, we are going to suspend opening new clinical trials, and we are not going to enroll new participants in existing clinical trials unless there’s someone with an acute cancer for which one of our clinical trials is likely to make them better,” Oyer said. “We’re going to focus our efforts right now on treatment trials rather than our prevention and registry trials.”
Shift in Focus for Biopharma
As businesses slowed down in most sectors worldwide because of the spread of the virus, the biopharmaceutical industry doubled its efforts to develop lifesaving vaccines and diagnostic tools for clinicians across medical specialties.
Testing
On March 13, Thermo Fisher Scientific Inc, a Massachusetts-based company responsible for developing both research and clinical cancer assays, announced that the FDA issued emergency use authorization (EUA) to its diagnostic test, TaqPath COVID-19 Combo Kit,15for detection of severe acute respiratory syndrome coronavirus (SARS-CoV-2) only and no other viruses or pathogens.16
“The authorization of our diagnostic test for COVID-19 will help to protect patients and enable medical staff to respond swiftly to treat those who are ill and prevent the spread of infection,” Marc N. Casper, chairman, president, and chief executive officer (CEO) of Thermo Fisher Scientific, said in a statement.
The test has not yet received FDA clearance or approval, but the designation allows use of the products in diagnosing, treating, or preventing a disease or conditionas in the case of COVID-19—after declaration of a public health emergency by the secretary of the US Department of Health & Human Services.16
Two additional actions by the FDA occurred simultaneously on March 16, when the agency issued an EUA to Hologic for its Panther Fusion SARS-CoV-2 Assay and to LabCorp for its COVID-19 Real-Time RT-PCR test.17
“Staff at FDA have been working nonstop to expedite the review and authorization of diagnostics during this public health emergency,” FDA Commissioner Stephen M. Hahn, MD, said in a statement. “Our device center has been in continual contact with the medical device communityin particular, diagnostic developers—since January [by] providing technical assistance to test developers to help facilitate the availability and distribution of tests so that health care professionals can accurately detect the COVID-19 virus. Since the beginning of this outbreak, more than 90 test developers have sought FDA guidance with the development and validation of tests they plan to bring through the EUA process.”
Emphasis on rapid results has taken hold for testing manufacturers and this led to the approval of the first point-of-care diagnostic test on March 21. The Cepheid Xpert Xpress SARS-CoV-2 test allows clinicians to know a patient’s diagnosis within hours rather than the few days it takes to get results by other testing measures.18
On April 1, the FDA issued an EUA for the use of a serology test from the manufacturer Cellex for the detection of the virus by antibodies in the blood. The advantages of this test are the quick turnaround time, about 15 minutes, and that it can be used in patients who may not be able to leave their homes.19
Oncologic Agents Under Investigation for COVID-19 Management
A randomized, double-blind, placebo-controlled phase III trial is exploring tocilizumab (Actemra) as a possible option for adult patients hospitalized with severe COVID-19 pneumonia. The immunosuppressive drug is FDA approved for the treatment of rheumatoid arthritis, giant cell arteritis, polyarticular juvenile idiopathic arthritis, and systemic juvenile idiopathic arthritis; it has also been a critical component in the development of chimeric antigen receptor T-cell therapies, for which it is used to manage cytokine release syndrome.20
“In these unprecedented times, today’s announcement is an important example of how industry and regulators can collaborate quickly to address the COVID-19 pandemic,” said Levi Garraway, MD, PhD, chief medical officer and head of global product development for Genentech, a member of the Roche Group.
Enrollment is expected to start in April 2020 with a target accrual of 330 patients internationally. Key trial end points include clinical status, mortality, mechanical ventilation, and intensive care unit variables.
Incyte, the company responsible for manufacturing the JAK inhibitor ruxolitinib (Jakafi), announced in April that it would be initiating a phase III trial of its agent as treatment for patients with COVID-19related cytokine storm. Ruxolitinib may be beneficial in treating patients with this condition as many features of patients with severe respiratory disease from the virus have features that appear consistent with increased activation of the JAK-STAT pathway.21And, a new phase II trial involving the oncologic agent leronlimab in treating patients with COVID-19 was cleared by the FDA (see page 75).
Vaccination Clinical Trial
A phase I clinical trial evaluating a COVID-19 vaccine was initiated on March 16 at the Kaiser Permanente Washington Health Research Institute in Seattle, with the first patient out of 45 healthy volunteers receiving the investigational agent on day 1.22
The open-label, dose-ranging clinical trial is assessing the safety of the vaccine, mRNA-1273, and its ability to induce an immune response. The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, is responsible for developing the vaccine and is also funding the trial.
“Finding a safe and effective vaccine to prevent infection with SARS-CoV-2 is an urgent public health priority,” Anthony S. Fauci, MD, director of NIAID, said in a statement. “This phase I study, launched in record speed, is an important first step toward achieving that goal.”
Dissemination of Information on Hold
Starting in late February, organizations hosting oncology meetings and conferences began releasing statements postponing their spring events, or in some cases, cancelling them. Academic facilities and cancer centers also issued bans prohibiting their faculty from nonessential travel.
The first wave of notable oncology meetings to be canceled or postponed included the National Comprehensive Cancer Network Annual Conference, originally planned for March 19 to 22 in Orlando, Florida23; the Society of Gynecologic Oncology Annual Meeting on Women’s Cancer, scheduled for March 28 to 31 in Toronto, Ontario, Canada24; and the American Association for Cancer Research Annual Meeting, scheduled for April 24 to 29 in San Diego, California.25
ASCO, which hosts one of the most important oncology meetings worldwide, announced on March 24 that it would deliver the latest abstracts virtually May 29 through June 2, when the annual meeting originally was to be held in Chicago, Illinois.26
In a related press release, leaders within the organization had this message: “We still intend to deliver the latest cancer science to the global community during the annual meeting time frame, using a virtual format that respects the contributions of the authors and the work of the Scientific Program Committee. In addition, abstracts will be published online and in the Journal of Clinical Oncology on our usual schedule.”
Moving Forward
The future impact of the pandemic on the medicine is unknown, but the effects will undoubtedly resonate for some time to come.
“Our primary concern is our patients, but of course we do not want the health care providers to become ill and need to be quarantined,” Evens said. “We are being cognizant of that and are trying to work together as a team to help [prevent] this.”
Oyer noted similar changes to the way in which he communicates with his patients. “We had adopted a process of doing nonessential visits on the telephone,” he said. “It’s a learning [curve] for all of us.” As understanding of COVID-19 develops daily, it is essential that clinicians in medicine stay up-to-date on the latest recommendations from public health entities.
“Become a member of the ACCC, ASCO, or another trusted organization so that you can learn from the experience of others. [Check in with] your local department of health; don’t go it alone,” Oyer concluded.
References
- Secretary Azar declares public health emergency for United States for 2019 novel coronavirus [news release]. Washington, DC: US Health & Human Services Press Office; January 31, 2020. bit.ly/2wocfkm. Accessed March 23, 2020.
- CMS prepares nation’s healthcare facilities for coronavirus threat [news release]. Washington, DC: Centers for Medicare & Medicaid Services; February 6, 2020. go.cms.gov/2xlddO8. Accessed March 23, 2020.
- Public health news alert: CMS develops new code for coronavirus lab test [news release]. Washington, DC: Centers for Medicare & Medicaid Services; February 13, 2020. go.cms.gov/33HcmmY. Accessed March 23, 2020.
- CMS issues clear, actionable guidance to providers about COVID-19 virus [news release]. Washington, DC: Centers for Medicare & Medicaid Services; March 9, 2020. go.cms.gov/3dnT5vC. Accessed March 23, 2020.
- Congress passes funding bill to respond to Coronavirus: summary of provisions of importance to the healthcare community. American Society of Clinical Oncology website. bit.ly/2xfiR4C. Published March 9, 2020. Accessed March 23, 2020.
- CMS takes action nationwide to aggressively respond to coronavirus national emergency [news release]. Washington, DC: Centers for Medicare & Medicaid Services; March 13, 2020. go.cms.gov/3afrbQb. Accessed March 23, 2020.
- CMS releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response [news release]. Washington, DC: Centers for Medicare & Medicaid Services; March 18, 2020. go.cms.gov/2y2V7Ry. Accessed March 23, 2020.
- Susan G. Komen suggests non-symptomatic women delay routine breast cancer screening this spring [news release]. Dallas, TX: Susan G. Komen; March 18, 2020. sgk.mn/3dm4ZpD. Accessed March 23, 2020.
- Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer [published online February 28, 2020]. J Thorac Oncol. doi: 10.1016/j.jtho.2020.02.010.
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335337. doi: 10.1016/S1470-2045(20)30096-6.
- Pasini L, Nash A. Pulmonary pathology of the novel Coronavirus in two patients with lung cancer. The ASCO Post website. bit.ly/2xeHBK9. Accessed March 23, 2020
- COVID-19 patient care information. American Society of Clinical Oncology website. bit.ly/2QG0JYq. Accessed March 23, 2020
- FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic. FDA website. bit.ly/3b1sORI. Published March 2020. Accessed March 19, 2020
- Interim guidance for patients on clinical trial supported by the NCI Cancer Therapy Evaluation Program and the NCI Community Oncology Research Program (NCORP). Cancer Therapy Evaluation Program website. bit.ly/2wvIwG4. Published March 13, 2020. Accessed March 19, 2020.
- TaqPath COVID-19 multiplex diagnostic solution. Thermo Fisher Scientific website. bit.ly/2UcUUT3. Accessed March 16, 2020.
- FDA issues emergency authorization to Thermo Fisher Scientific for diagnostic test used to detect COVID-19 [news release]. Waltham, MA: Thermo Fisher Scientific Inc; March 13, 2020. bit.ly/38Xo1z6. Accessed March 16, 2020.
- Coronavirus (COVID-19) update: FDA issues diagnostic emergency use authorization to Hologic and LabCorp [news release]. Silver Springs, MD: FDA; March 16, 2020. bit.ly/2WyGShD. Accessed March 23, 2020.
- Coronavirus (COVID-19) Update: FDA Issues first Emergency Use Authorization for Point of Care Diagnostic. FDA website. bit. ly/2UTC5WL. Published March 21, 2020. Accessed April 9, 2020.
- Mandavilli A. F.D.A. approves first coronavirus antibody test in U.S. NY Times website. nyti.ms/3e87hZM. Published April 2, 2020. Accessed April 9, 2020.
- Genentech initiates phase III clinical trial of Actemra in hospitalized patients with severe COVID-19 pneumonia [news release]. South San Francisco, CA: Genentech; March 18, 2020. bit.ly/2UvCnBK. Accessed March 19, 2020.
- Incyte Announces Plans to Initiate a Phase 3 Clinical Trial of Ruxolitinib (Jakafi) as a Treatment for Patients with COVID-19 Associated Cytokine Storm [news release] Wilmington, DE: Incyte; April 2, 2020. bwnews.pr/2ypBaEA. Accessed April 3, 2020.
- NIH clinical trial of investigational vaccine for COVID-19 begins. National Institutes of Health website. bit.ly/2ITwXew. Published March 16, 2020. Accessed March 16, 2020.
- National Comprehensive Cancer Network postpones 2020 annual conference, citing precautions against potential patient exposure to COVID-19 [news release]. Plymouth Meeting, MA: National Comprehensive Cancer Network; March 5, 2020. bit.ly/2WAu9uC. Accessed March 6, 2020.
- 2020 annual meeting coronavirus update. Society of Gynecologic Oncology website. bit.ly/2UtDWjI. Accessed March 23, 2020.
- AACR Annual Meeting 2020: update on rescheduled meeting in August and announcement of virtual annual meeting preview. American Association for Cancer Research website. bit.ly/3aeNe9Q. Published March 20, 2020. Accessed March 23, 2020.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.