HITTING THE TARGET: Approvals for Companion Tests Rise in Step With Targeted Agents
Expanded indications in the treatment of cancers with novel therapy biomarkers were a notable result of drug approvals in the past year. In order to facilitate the identification of these molecular markers, more targeted agents are being approved with associated companion diagnostics, made evident by 3 such tests approved in 2019.
John Simmons, PhD

Expanded indications in the treatment of cancers with novel therapy biomarkers were a notable result of drug approvals in the past year. In order to facilitate the identification of these molecular markers, more targeted agents are being approved with associated companion diagnostics, made evident by 3 such tests approved in 2019.
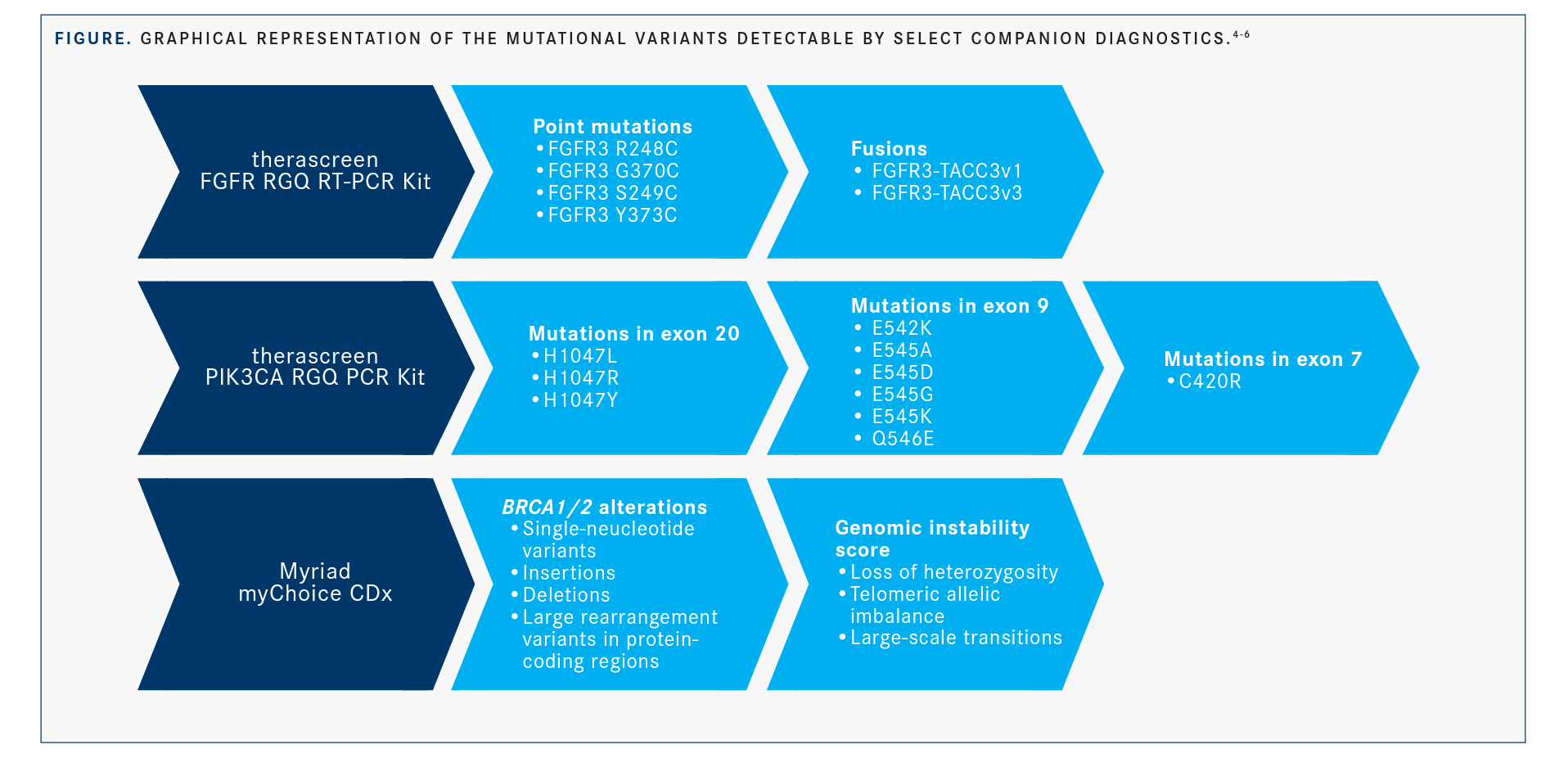
The multikinase inhibitor erdafitinib (Balversa) and the PI3K inhibitor alpelisib (Piqray) both received initial approval for biomarker-specific indications in the first half of 2019.1,2 Niraparib (Zejula), a PARP inhibitor previously approved for maintenance treatment of patients with ovarian cancer, received an expanded indication for the treatment of patients with homologous recombination deficiency (HRD)positive ovarian tumors after prior therapy.3 All 3 decisions were accompanied by approvals for associated companion diagnostic tests (FIGURE).4-6
“The biomarker landscape has fundamentally changed in the past 3 years,” John Simmons, PhD, vice president of translational medicine at Personal Genome Diagnostics, a biotechnology company in Baltimore, Maryland, said in an interview with Targeted Therapies in Oncology. “Previously, we were only really seeing a focus in discussing precision oncology in the lung cancer space. Now we are seeing the [use of] actionable alterations and associated therapies shift from 1 or 2 tumor types to many others.”
According to Simmons, the ability to understand the tumor on the genomic level is becoming increasingly more vital to the successful treatment of patients. He added that in certain cases, as with the tumor types described herein, use of a single-gene assay is beneficial during treatment selection.
FGFR2/3-Mutant Urothelial Cancer
In April 2019, the FDA approved erdafitinib for the treatment of locally advanced or metastatic urothelial carcinoma with susceptible FGFR3 or FGFR2 genetic alterations after progression on or following platinum-containing chemotherapy.1 On the same day, Qiagen announced the launch of its novel therascreen FGFR RGQ RT-PCR Kit (therascreen FGFR Kit) as a companion diagnostic intended to guide patient selection for this agent.7
The approval was based on data from 87 previously treated patients with certain FGFR3 mutations or FGFR2/3 fusions enrolled in the BLC2001 study (NCT02365597), in which the objective response rate (ORR) was 32.2% (95% CI, 22.4%-42.0%) in patients whose alterations were detected by an investigational clinical trial assay (CTA).1,5 Patients with responses to erdafitinib included those who had previously not responded to anti–PD-1/PD-L1 therapy.1
The therascreen FGFR Kit is a 2-step, reverse-transcription, real-time polymerase chain reaction assay clinically validated for the detection of 6 alterations: point mutations in exon 7 of FGFR3 producing the amino acid variants R248C and S249C and in FGFR3 exon 10 producing variants G370C and Y373C, as well as the fusions FGFR3-TACC3v1 and FGFR3-TACC3v3. Each kit contains reagents for up to 24 patient specimens derived from formalin-fixed, paraffin-embedded urothelial tumor tissue as well as additional controls.4
To test the validity of the kit compared with an analytically validated high-throughput orthogonal method, investigators conducted a study with specimens from the pivotal BCL2001 trial (n = 271) and the same intended-use population (n = 36).4
The positive percentage agreement (PPA) between the kit and the comparator method was 99.04% (95% CI, 94.76%-99.98%), and the negative percentage agreement (NPA) was 97.52% (95% CI, 94.32%-99.19%) in the same group. The overall percentage agreement (OPA) for the 306 patients tested was 98.04% (95% CI, 95.78%-99.28%). The 6 patient sam-ples with discordant results included 1 spec-imen with a negative result by the kit and a positive result by the comparator method; the other 5 specimens had the opposite result.4
After examining the concordance between the kit and the comparator method for each alteration, investigators observed a PPA of 100% for the S249C, G370C, and Y373C point mutations and the FGFR3-TACC3v1, FGFR3-TAC-C3v3, and FGFR3-BAIAP2L1 fusions.4
ORR in patients positive for FGFR alterations by both the CTA and the therascreen FGFR Kit was 33.3% (95% CI, 23.4%-45.1%). Alterations, as detected by the kit, with the highest ORRs included FGFR3 Y373C (50%; 95% CI, 23.7%-76.3%) and FGFR3 S249C (35.1%; 95% CI, 21.8%-51.2%), with the lowest ORRs recorded for the fusions FGFR3-BAIAP2L1 and FGFR3-TACC3v3, at 0% each. Although the therascreen FGFR Kit was designed to evaluate 5 fusions, sufficient clinical sample materials were available for the clinical validation of FGFR3-TACC3v1 and FGFR3-TACC3v3 only. Results of an ongoing phase III trial will determine whether the kit’s approval can be extended to the FGFR2-BICC1, FGFR2-CASP7, and FGFR3-BAIAP2L1 fusions.4
Breast Cancer With PIK3CA Mutations
The FDA approved alpelisib in May 2019 for the treatment of postmenopausal women and men with hormone receptor–positive, HER2-negative advanced or metastatic breast cancer with PIK3CA mutations, as detected by an FDA-approved test, following disease progression on or after endocrine-based ther-apy.2 The randomized phase III SOLAR-1 trial (NCT02437318) served as the basis for the approval. In this study, the PI3K inhibitor plus fulvestrant improved median progression-free survival (PFS) versus placebo/fulvestrant at 11.0 months and 5.7 months, respectively (HR, 0.65; 95% CI, 0.50-0.85; P = .001).2
Qiagen, the manufacturer of the therascreen FGFR Kit, released its therascreen PIK3CA RGQ PCR Kit (therascreen PIK3CA Kit) on the same day that the FDA approved alpelisib. This kit is the first FDA-approved assay for guiding breast cancer treatment decisions using either circulating tumor DNA or paraffin-embedded tumor tissue.8
The kit contains reagents for the detection of 11 individual mutations in exons 7, 9, and 20 of the PIK3CA gene, as well as an unmu-tated region of PIK3CA exon 15 used as a control. The kit can detect the following point mutations in PIK3CA: E542K, E545K, E545D, E545G, E545A, H1047Y, H1047L, H1047R, Q546R, Q546E, and C420R.5
Validation of the kit was achieved through analysis of tissue obtained from the SOLAR-1 clinical trial as well as contrived samples, which are laboratory-created samples designed to mimic clinical samples. The rationale for using contrived samples centered on the rarity of some of the mutations being tested for. Valida-tion involved a comparator analysis between the kit and a previously validated next-generation sequencing (NGS)–based reference method.5
The comparison of the therascreen PIK3CA Kit and NGS produced a PPA and an NPA of 97.39% (95% CI, 93.44%-99.28%) and 91.26% (95% CI, 88.00%-93.87%), respectively. The OPA was 92.99% (95% CI, 90.50%-94.99%).5
Of the 542 total samples tested, 38 produced discordant results, including 4 samples that were positive for a mutation by NGS and neg-ative by therascreen PIK3CA Kit using plasma samples and 34 with the opposite outcome. For 29 of the discordant samples, the kit produced positive results for both tissue and plasma samples; for the other 5, kit results were negative for tissue but positive for plasma.5
PFS analysis in 185 patients with plasma samples positive for PIK3CA mutations indicated that alpelisib plus fulvestrant resulted in a 46% reduction in the risk of disease progression or death compared with placebo plus fulvestrant (HR, 0.54; 95% CI, 0.33-0.88).5
Of note, comparing tissue and plasma samples using the therascreen PIK3CA Kit yielded some discordant results. Of 549 samples, 149 had mutation-positive results by tumor tissue and negative results by plasma, resulting in a PPA of 54.6% (95% CI, 49.0%-60.1%) for the 2 sample types. The NPA in the same analysis was 97.2% (95% CI, 94.0%-99.0%), and the OPA was 71.5% (95% CI, 67.5%-75.2%). Because approximately 46% of mutations detected in tissue were missed in the plasma test, reflex tissue testing using tissue specimens will be required in the event that plasma testing is negative.5
Simmons detailed how these tests, despite discordant outcomes, can serve an unmet need in oncology practice. “In some cases, there may not be enough [tissue] material to input into a test,” he said. “Maybe they’ve had other targeted therapies or there has been evolution [of the tumor following those] therapies. In that case, you may need to know the biomarker status of that tumor the day that you are making that treatment decision. This paradigm of having a test with a reflex claim is actually quite useful. If the mutation is detected, it’s actionable.”
Furthermore, Simmons said, positive results from these companion diagnostic tests are reliable. “We are not seeing issues with specificity. If you can do the blood test and identify an actionable variant, then you may not need to do another biopsy, and that may be a great benefit to the patient as well as a cost savings to the health system,” he said.
Simmons said finding these mutations in plasma samples is like finding a needle in a haystack. “We are always working to develop test sensitivity, [and] we are working at the outer limits of the technology,” he noted.
Ovarian Tumors With HRD
Clinical evidence has long pointed to the efficacy of PARP inhibitors in the treatment of patients with HRD-positive tumors.9 In October 2019, the FDA expanded the indication for niraparib in the treatment of patients with ovarian, fallopian tube, or primary peritoneal cancer to include patients treated with 3 or more prior chemotherapy regimens whose cancer is associated with HRD, defined as either deleterious or suspected deleterious BRCA mutations or genomic instability in patients with disease progression >6 months after response to the last platinum-based chemotherapy.3
The agency based the approval on data from the phase II QUADRA trial (NCT02354586), in which the ORR was 24% and the duration of response was 8.3 months in the heavily pretreated patient population.3
The myChoice CDx companion diagnostic assay from Myriad Genetics, Inc, was approved for use with niraparib. According to the manufacturer, this is the first tumor test capable of detecting BRCA1/2 alterations as well as genomic instability.10
Similar to the validation process for the therascreen FGFR Kit, investigators compared the myChoice assay and an NGS-based reference assay to analyze genetic alterations in patient tumor samples. They examined a range of representative tumor BRCA1/2 sequence variants and large genomic rearrangements, as well as the genomic instability score (GIS), an algorithmic measurement of loss of heterozygosity, telomeric allelic imbalance, and large-scale state transitions.6
All 1733 samples that tested positive for BRCA1/2 sequence variants with ≥10% allele frequencies by the reference NGS were also positive by the myChoice assay, for a PPA of 100%. For variants with <10% allele frequency, the PPA was 99.94%. For nonvariant base calls, the NPA was 100%. The OPA for 402 BRCA1/2 large rearrangement calls was 100%.6
Investigators examined results of the accuracy study for 3 patient outcomes: tumor BRCA1/2 status based on BRCA1 and BRCA2 sequence and large rearrangement analyses, GIS status, and Myriad HRD status (a combination of the first 2 items).10 Tumor BRCA1/2 status yielded 100% concordance between myChoice CDx and the NGS comparator assay, with only 7 samples producing invalid results by the companion diagnostic.10 For GIS status, the concordance between myChoice CDx and the comparator assay yielded a PPA of 98.5% (95% CI, 94.6%-99.8%) and an NPA of 97.4% (95% CI, 90.8%-99.7%), for an OPA of 98.1% (95% CI, 95.1%-99.5%).10 When HRD status was analyzed for concordance between myChoice CDx and the comparator assay, the OPA was 98.5% (95% CI, 95.8%-99.7%). The PPA and NPA were 98.5% (95% CI, 94.8%-99.8%) and 98.6% (95% CI, 92.4%-100.0%), respectively.6
Future of Clinical Assays
Simmons advocated for biomarker testing of singular mutations as well as at the comprehensive genomic level. “I strongly advocate that patients who have a tumor type that has an approved therapy based on a biomarker be tested for that biomarker. Precision oncology is not precise without the diagnostics,” he said.
Moving forward, Simmons said, being able to test for multiple genes at a time will be increasingly important. “With pan-cancer biomarkers and a number of different drugs being approved for particularly actionable targets, that will further drive the field’s ability to have [an] impact on patient care for those with advanced disease,” he concluded.
References
1. FDA grants accelerated approval to erdafitinib for metastatic urothelial carcinoma. FDA website. bit.ly/39Nyhvn. Published April 12, 2019. Accessed March 9, 2020.
2. FDA approves alpelisib for metastatic breast cancer. FDA website. bit.ly/2vPPuoU. Updated May 28, 2019. Accessed March 9, 2020.
3. FDA approves niraparib for HRD-positive advanced ovarian cancer. FDA website. bit.ly/2TPga1b. Published October 23, 2019. Accessed March 9, 2020.
4. Summary of safety and effectiveness data (SSED): therascreen FGFR RGQ RT-PCR Kit. FDA website. bit.ly/3cK20qH. Published April 12, 2019. Accessed March 9, 2020.
5. Summary of safety and effectiveness data (SSED): therascreen PIK3CA RGQ PCR Kit. FDA website. bit.ly/3cCYgXY. Published May 24, 2019. Accessed March 9, 2020.
6. Summary of safety and effectiveness data (SSED): Myriad myChoice CDx. FDA website. bit.ly/3a1LyAj. Published October 23, 2019. Accessed March 9, 2020.
7. Qiagen launches first FDA-approved companion diagnostic using FGFR alterations to help guide the treatment of metastatic urothelial cancer [news release]. Germantown, MD, and Hilden, Germany: Qiagen NV; April 12, 2019. bwnews.pr/2Q0dVHc. Accessed March 9, 2020.
8. Qiagen launches first FDA-approved companion diagnostic PIK3CA biomarkers to enhance precision medicine in breast cancer [news release]. Germantown, MD, and Hilden, Germany: Qiagen NV; May 24, 2019. bwnews.pr/2Qr03Gd. Accessed March 9, 2020.
9. Yi T, Feng Y, Sundaram R, et al. Antitumor efficacy of PARP inhibitors in homologous recombination deficient carcinomas. Int J Cancer. 2019;145(5):12091220. doi: 10.1002/ijc.32143.
10. FDA approves Myriad’s myChoice CDx test to help identify women eligible for treatment with Zejula in late-line ovarian cancer [news release]. Salt Lake City, UT: Myriad Genetics Inc; October 23, 2019. bit.ly/39Gq3oH. Accessed March 10, 2020.

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More