Patients With Pretreated Sarcoma May Derive Benefit From Various Immunotherapy Combinations
Combination therapy strategies involving immune checkpoint inhibitors and a secondary agent have shown promise across sarcoma subtypes, according to analysis of clinical trial data that were presented at the European Society for Medical Oncology Sarcoma & GIST Symposium 2020, held in Milan, Italy.
Combination therapy strategies involving immune checkpoint inhibitors and a secondary agent have shown promise across sarcoma subtypes, according to analysis of clinical trial data that were presented at the European Society for Medical Oncology Sarcoma & GIST Symposium 2020, held in Milan, Italy.1
“Combining strategies seems to be more effective than antiPD-1 alone in sarcomas,” Javier Martin-Broto, MD, PhD, a medical oncologist at the University Hospital Virgen del Rocio in Seville, Spain, wrote in his presentation of the data. Martin-Broto compared sarcomas within the immune context of melanoma, a cancer which has experienced significant benefit with the integration of PD-1/PD-L1 inhibitors into treatment paradigms. In general, sarcomas have a much lower mutational burden than melanoma tumors and are less likely to be positive for PD-L1 expression.
Tumor mutational burden by subtype for angiosarcomas, undifferentiated pleomorphic sarcomas, and leiomyosarcomas is typically in the range of 2 to 3 mutations/ megabase versus <2 mutations/megabase that is observed with myxofibrosarcomas, liposarcoma, and synovial sarcoma. Even within certain subtypes, mutational burdens can range in value as demonstrated by the 13% of angiosarcomas with >20 mutations/megabase.
Martin-Broto began by exploring data related to the use of the PD-1/CTLA-4 inhibitor combination of nivolumab (Opdivo) plus ipilimumab (Yervoy) or nivolumab monotherapy in patients with advanced or unresectable sarcoma who had received at least 1 prior line of therapy. This patient cohort was heavily pretreated, with more than half of patients (61%) having received at least 3 prior lines of therapy.
Complete responses were observed in 5% of patients undergoing the combination therapy. Partial responses were observed in 5 patients (13%) treated with the combination and in 3 patients (8%) who received monotherapy. The corresponding confirmed objective response rates were 5% and 16% with clinical benefit rates of 18% and 29%, respectively.2
The investigators concluded that the combination cohort met the trial’s primary end point, with responses observed in leiomyosarcomas, myxofibrosarcoma, undifferentiated pleomorphic sarcomas, and angiosarcoma, and the survival rate at 1 year for the combination cohort exceeded expectations for these patients. However, high rates of grade 3/4 adverse events were observed with the combination (14% vs 7%).2
“Targeting 2 checkpoints offers higher ORRs [objective response rates] and PFS [progression-free survival] and could be improved if treatment can be prolonged for both,” Martin-Broto wrote.
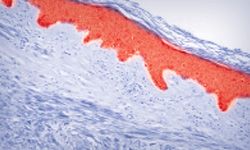
Another potentially viable strategy being explored is the combination of PD-1 inhibitors with an antiangiogenic agent, which are thought to enhance the efficacy of immunebased cancer therapies. Angiogenic factors, such as vascular endothelial growth factor A, may have suppressive effects on the immune response and may induce expression of inhibitory molecules such as PD-1 (FIGURE).3
According to Martin-Broto, “Antiangiogenic and antiPD-1 seems to offer better disease control in selected sarcoma subtypes than monotherapy.”
In a phase II trial, pembrolizumab (Keytruda) was combined with axitinib (Inlyta) for use in patients with previously treated advanced sarcoma, including those with alveolar soft-part sarcoma who accounted for 36% of the population. Thirty-six percent of patients had 2 or more prior lines of therapy, 51% had received prior tyrosine kinase inhibitors, and 61% had an ECOG performance status score of 0.4
Out of 32 total patients, 8 (25%) experienced a partial response and 9 (28%) had stable disease, for a clinical benefit rate of 53.1%. These results coupled with a manageable toxicity profile led investigators to conclude that this combination has activity in patients with advanced sarcomas, especially alveolar softpart sarcoma, and should be studied further.
In a phase II trial, patients with advanced soft tissue sarcoma were treated with the combination of sunitinib (Sutent) and nivolumab. The trial met its primary end point, with a 6-month PFS rate of 50% at 6 months. The overall survival rate at 6 months was 77%.5
Another phase I/II trial examined chemoimmunotherapy in patients with advanced sarcoma using doxorubicin with pembrolizumab. After the recommended dose for doxorubicin was determined in phase I, a 24-week PFS rate of 73% was observed in phase II. This compared favorably with the 30% PFS rate that was gleaned from data out of a retrospective cohort. The response rate was 22%.6
Other strategies that warrant further investigation include combining PD-1 inhibition with anti-LAG3 agents, radiotherapy, and IDO1 inhibitors, among other treatment strategies, Martin-Broto concluded.
References
- Martin Broto J. Combination immunotherapy attempts. Presented at: European Society for Medical Oncology Sarcoma & GIST Symposium 2020; February 3-5, 2020; Milan, Italy. bit.ly/3dzJ0LQ.
- D’Angelo SP, Mahoney MR, Van Tine BA, et al. A multi-center phase II study of nivolumab +/- ipilimumab for patients with metastatic sarcoma (Alliance A091401).J Clin Oncol. 2017;35(suppl 15; abstr 11007). doi: 10.1200/JCO.2017.35.15_suppl.11007
- Motz GT, Coukos G. The parallel lives of angiogenesis and immunosuppression: cancer and other tales.Nat Rev Immunol. 2011;11(10):702-711. doi:10.1038/nri3064
- Wilky BA, Trucco MM, Subhawong TK, et al. Axitinib plus pembrolizumab in patients with advanced sarcomas including alveolar soft-part sarcoma: a single-centre, single-arm, phase 2 trial.Lancet Oncol. 2019;20(6):837-848. doi: 10.1016/S1470-2045(19)30153-6
- Martin Broto J, Hindi N, Grignani GE, et al. IMMUNOSARC: a collaborative Spanish (GEIS) and Italian (ISG) sarcoma groups phase I/II trial of sunitinib plus nivolumab in advanced soft tissue and bone sarcomas: results of the phase II- soft-tissue sarcoma cohort.Ann Oncol. 2019;30(suppl 5; abstr 1669O). doi: 10.1093/annonc/mdz283.002
- Pollack S, Redman MW, Wagner M, et al. A phase I/II study of pembrolizumab (Pem) and doxorubicin (Dox) in treating patients with metastatic/unresectable sarcoma.J Clin Oncol.2017;37(suppl 15; abstr 11009). doi: 10.1200/JCO.2019.37.15_suppl.11009

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More