McKay Discusses Important Updates in Treatment, Management of Clear Cell RCC
During a Targeted Oncology case-based roundtable event, Rana R. McKay, MD, discussed updates to key trials in advanced clear cell renal cell carcinoma.
Rana R. McKay, MD
Associate Professor of Medicine
UC San Diego Health
Medical Oncologist
Koman Family Outpatient Pavilion
La Jolla, CA

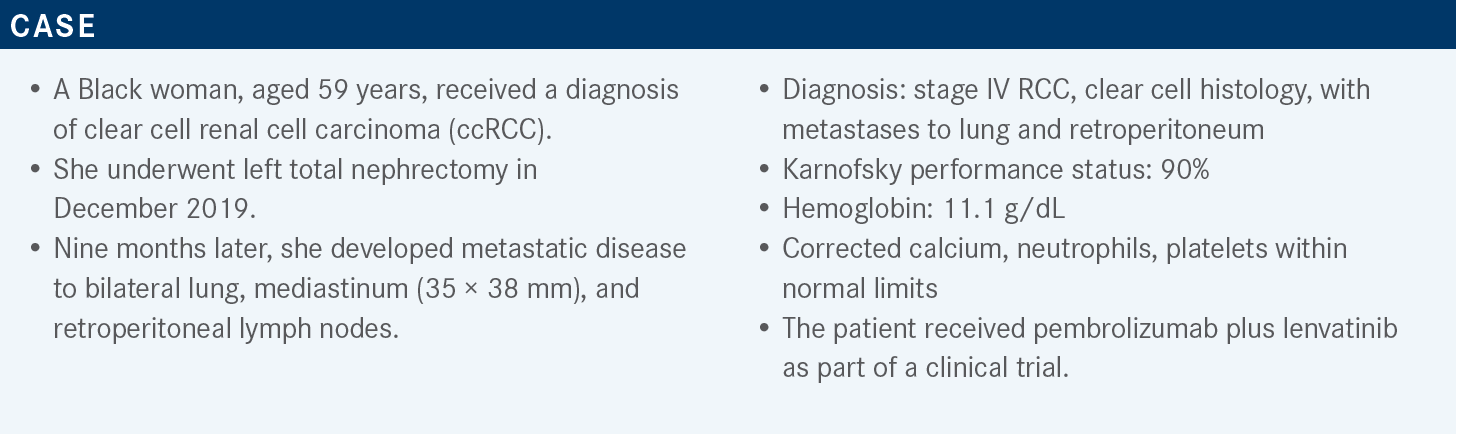
Targeted OncologyTM: Can you discuss the most recent updates in the guidelines for treating ccRCC?
McKAY: The most recent version of the National Comprehensive Cancer Network [NCCN] guidelines [are from June] of this year.1 We are trying to be better on the guidelines panel with breaking up the preferred regimens based on level 1 and phase 3 data.
For favorable-risk patients, preferred regimens include the IO [immunotherapy]/TKI [tyrosine kinase inhibitor] combinations, whether that be axitinib [Inlyta]/pembrolizumab [Keytruda], cabozantinib [Cabometyx]/nivolumab [Opdivo], or lenvatinib [Lenvima]/pembrolizumab. For the poor-[risk] and intermediate-risk patients, we have all the above options, with the addition of nivolumab plus ipilimumab [Yervoy], and the addition of cabozantinib, based on data from the CABOSUN trial [NCT01835158],2 for those patients who may not necessarily be candidates for IO therapy.
The other regimens under column 2 of the NCCN guidelines for favorable risk also include nivolumab/ipilimumab, so it’s not necessarily excluded from use in the favorable-risk patients but it’s not under the preferred regimens. Under some circumstances, active surveillance could certainly be an option for those favorable-risk individuals.
I feel with every passing meeting we need to keep updating information for immune checkpoint inhibitor combination trials [for patients with metastatic RCC]. For instance, CheckMate 9ER [NCT03141177] now has the largest population of patients who had poor-risk disease [compared with other trials].3 The JAVELIN Renal 101 trial [NCT02684006]4 is not [discussed as much], because that trial has not read out for overall survival [OS] yet. Even though it’s an FDA-approved regimen, I think in clinical practice that regimen’s not being used.
The CLEAR study [NCT02811861] included the least number of patients with poor-risk disease and the KEYNOTE-426 [NCT02853331] trial enrolled the highest proportion of patients who had favorable-risk disease.5-11 The median follow-up was 67.7 months in the CheckMate 214 trial [NCT02231749] that had the longest follow-up [and a median OS of 47 months (95% CI, 35.4-57.4) on nivolumab plus ipilimumab vs 26.6 months (95% CI, 22.1- 33.5) for patients on sunitinib ([Sutent] HR, 0.68; 95% CI, 0.58-0.81, P < .0001)].12,13 We’ve also got almost 4 years of follow-up from KEYNOTE-426 and then about 32 to 33 months from CheckMate 9ER and CLEAR, respectively.
All these regimens did demonstrate statistically significant improvement in OS, and the HR held steady right around 0.72 across these trials in the intent-to-treat populations. It is also important to look at the landmark OS at 12 months and 24 months that ideally, we would even have 36 months here, but we just don’t have that follow-up for the later studies.
Clearly, there are statistically significant improvements in OS across these data, and it is the durability that’s seen with the CheckMate 214 data [that’s so impressive]—that even at 30 months and after, we’re seeing that 70% hold steady over time, which I think is reassuring, providing the durability of nivolumab. For other trials there just isn’t as much follow-up yet, but hopefully we’ll continue to monitor the rates of patients who continue to be disease controlled without progression at 3, 4, 5 years out from treatment initiation.
I think the [progression-free survival] PFS data are superior, and I think the IO/TKI regimens induce a response quicker. The response rates are higher with those regimens, as compared with CheckMate 214 with nivolumab/ipilimumab. Then, as we look at complete response [CR] rates, I think these vary upward to 12% with CheckMate 214 [and] 16%, which is the highest, with the CLEAR trial, but keep in mind that this trial included the least number of patients with poor-risk disease and many patients who had favorable-risk disease, so it’s hard to totally compare.
The primary progressive disease [PD] rate is about 1 in 5 for CheckMate 214 with nivolumab/ipilimumab. The rates of primary PD with CheckMate 9ER and with CLEAR from nivolumab plus cabozantinib and lenvatinib plus pembrolizumab are less than 10%.
As you’re thinking about regimens to use, if you’ve got a patient who needs an immediate response to treatment [and] you need to get their disease controlled, you can’t afford to have them have a PD as best response. The nivolumab plus cabozantinib and lenvatinib plus pembrolizumab may be good regimens to use in that context, but for somebody [for whom] you’re worried about that almost-1-in-5 PD rate, that’s something to consider with the nivolumab/ipilimumab data.
What is the CR rate for high-dose IL-2?
The CR rate with high-dose IL-2 is less than 10%. When we used to select patients for high-dose IL-2, it was patients in the favorable-risk category as opposed to individuals in the intermediate[-risk] or poor-risk [categories]. If we think of high-dose IL-2, it’s somebody who had prior nephrectomy and they’re presenting with low-volume disease and perfect health; that was your optimal candidate for high-dose IL-2.
There could be a role for high-dose IL-2, but it’s been largely supplanted with the nivolumab/ipilimumab data, given the durability of the response. Durability of response is at 30% for nivolumab/ipilimumab, where you’re likely “curing” patients at the 30% mark—just under [one-]third of patients, but again, the primary PD rate is 1 in 5, and then everybody’s sort of in the middle.
Are there any ideal biomarkers you are excited about in this setting?
The most exciting thing right now is probably the RNA signatures. The IMmotion151 trial [NCT02420821]14 looked at atezolizumab [Tecentriq] plus bevacizumab [Avastin] vs sunitinib in the frontline setting, [and although that] trial was ultimately a negative study, there was some rich correlative work done doing [RNA sequencing] on the baseline biopsies, archival nephrectomy specimens, and clustering patients into 6 to 7 categories.
There are also signatures that seem associated with response to VEGF inhibition, [whereas other] signatures seem associated with response to IO. Thinking of a rational way to design a trial where you stratify therapy based on the signature is being explored now, but I think there’s no front-runner in the clinic, and PD-L1 status has not been very helpful with treatment selection for RCC.
Do you ever look at circulating tumor DNA magnitude decrease to look to counteract pseudoprogression?
Circulating tumor cells [CTCs] have been another challenging area in RCC because, unlike other solid tumor malignancies such as prostate cancer and breast cancer, which use epithelial cell adhesion molecule [EpCAM] capture to identify CTCs, RCC does not express EpCAM. The detection mechanism is different in RCC.
There are many research labs working on different captures, whether it be through CA9 and CA12 or the cytokeratins to try to identify the RCCs in circulation. I think Epic has a platform where they’re basing it solely off morphology, but I think CTC capture has been more difficult in RCC, and that classic CTC conversion that we see in prostate cancer, going from greater than 5 to less than 5, has not necessarily been validated in RCC treatment.
Can you highlight the results of the CLEAR trial?
This was a phase 3 trial that looked at frontline lenvatinib plus pembrolizumab, or lenvatinib plus everolimus [Afinitor], vs sunitinib.7 The patients who were enrolled in the trial were patients with ccRCC who were treatment naive with a Karnofsky performance status of 70 or higher. The patients had measurable disease; stratification factors were largely based on a region of the world where the patients were enrolled, and Memorial Sloan Kettering Cancer Center [MSKCC] risk stratification.
This was one of the only frontline trials to date that had 3 arms to which patients were getting randomized. The primary end point was PFS by independent review, based on RECIST, and secondary end points included survival, objective response, safety, and health-related quality of life.
Something key is the dosing of the lenvatinib. In the combination with pembrolizumab, the lenvatinib dose is at 20 mg, and in the combination with everolimus, lenvatinib dose is at 18 mg.
We don’t use monotherapy lenvatinib in RCC, but monotherapy dosing is at 24 mg. With the lenvatinib dose, the strategy on this trial has been to start high and down-titrate, as opposed to CheckMate 9ER where there was a more middle-of-the-road dose selected, but the dose of lenvatinib here was 20 mg in combination with pembrolizumab.
At a median follow-up of 26.6 months, the combination of lenvatinib plus pembrolizumab resulted in a statistically significant improvement in PFS over sunitinib, with HR of 0.39 [95% CI, 0.32-0.49; P < .001]. The median PFS for lenvatinib/pembrolizumab was at 23.9 months [95% CI, 20.8-27.7]—that’s the longest PFS we’ve seen across all the 4 trials. Additionally, the combination of lenvatinib plus everolimus did demonstrate a statistically significant improvement in PFS over sunitinib, with HR here of 0.65 [95% CI, 0.53-0.80; P < .001].
The lenvatinib/everolimus arm had a PFS of 14.7 months [95% CI, 11.1-16.7]. With regard to the sunitinib arm here, probably a little bit better than what we would see at 9.2 months [95% CI, 6.0-11.0], but that was the performance of the control arm. Broken down by subgroups, including MSKCC risk group for those patients with favorable-[risk], intermediate- [risk], and poor-risk disease, there was a favoring of lenvatinib/pembrolizumab over sunitinib, with the direction of the HR being less than 1 across the different subgroups.
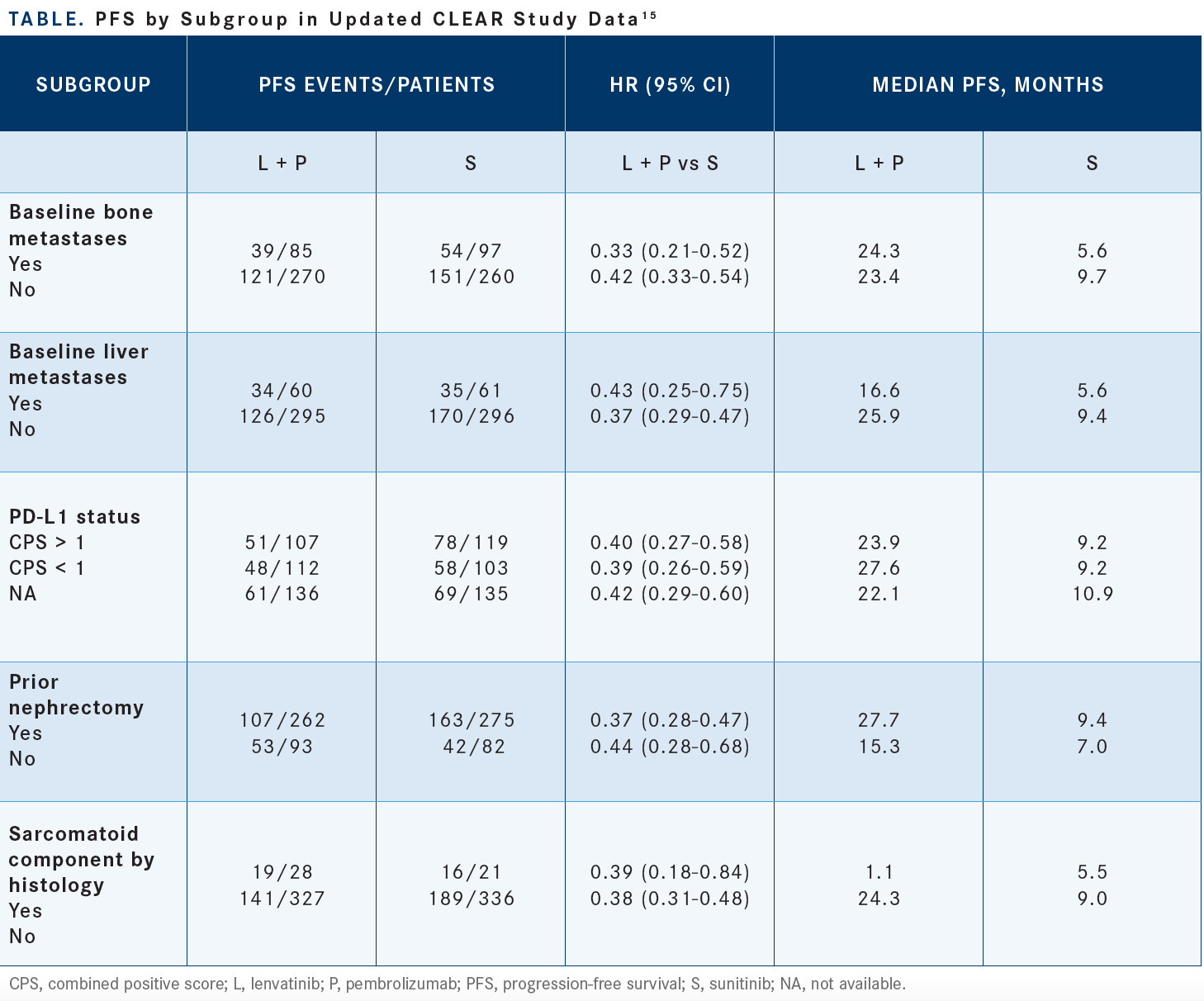
Updated subgroups, published in an abstract from the European Society of Oncology Meeting [2022]—including patients with the presence of baseline bone metastases, baseline liver metastases, PD-L1 status identified by their combined positive score, prior nephrectomy status, and the presence or absence of sarcomatoid histology—also saw a PFS benefit with lenvatinib and pembrolizumab over sunitinib [Table15].
[Looking at the] OS data at a median follow-up of 26.6 months, we see a statistically significant improvement in OS, with lenvatinib plus pembrolizumab vs sunitinib.7,9 The HR here is 0.66; that was also statistically significant [95% CI, 0.49-0.88; P = .005]. However, the median is not yet reached across all these groups. When we look at the combination of lenvatinib/everolimus vs sunitinib, this was not different than the sunitinib-treated patients. The HR here was 1.15, and the HRs did cross 1. The P value here was not significant, so there was no improvement in OS with frontline lenvatinib/everolimus, but we did demonstrate that with lenvatinib/pembrolizumab.
Updated data had a 33.7-month follow-up that showed the HR still demonstrated improvement over sunitinib but did drift upward a bit to 0.72 [95% CI, 0.55-0.93] from the initial reporting out of 0.66.7,9 The objective response rate [ORR] is the highest we’ve seen with this combination [lenvatinib/pembrolizumab] at 71%, 53.5% with lenvatinib/everolimus, and 36.1% with sunitinib.7,8 Again, the lenvatinib/pembrolizumab CR rate was at 16.1%, a primary PD rate of 5.4%. These are things to think about as you’re selecting regimens. Among patients who experienced a CR with lenvatinib plus pembrolizumab, at 24 months, 79% of patients maintained a CR, and at 36 months 74% of patients maintained a CR.
What was the safety profile observed in this study?
One thing to highlight is the grade 3 or higher adverse events [AEs], which with lenvatinib plus pembrolizumab was seen in 82.4% [of patients], 83.1% with lenvatinib/ everolimus, and 71.8% with sunitinib but with high rates of grade 3 toxicity.7 The AEs that resulted in dose reduction or dose modification were seen in 68.8% of patients treated with lenvatinib plus pembrolizumab.
The proportion of patients who needed to discontinue both drugs of the regimen, meaning permanently discontinue the whole regimen, was at 13.4%. Some AEs, like hepatotoxicity, were not at a frequency of greater than 20% of the population. The biggest AEs to keep in mind are diarrhea; the hypertension is key and stands out; the proteinuria is key, stands out; hand-foot syndrome [palmar-plantar erythrodysesthesia].
Can you discuss the dosing strategy for lenvatinib/pembrolizumab?
The recommended dosage for lenvatinib is 20 mg daily, with the pembrolizumab at 200 mg every 3 weeks, and that’s basically continued until disease progression or for up to 2 years. After completion of 2 years of combination therapy, lenvatinib can be administered as a single agent until PD. That’s how the trial was designed: that at the 2-year mark, based on investigator assessment, the pembrolizumab could be discontinued. The dosing strategy [of this treatment is] 20 mg, 14 mg, 10 mg, and 8 mg daily, and then, based on toxicity, whether it be persistent grade 2 or grade 3 toxicity, dose reducing as needed.
What are the highlights of the CheckMate 9ER data, and how has the trial influenced treatment management?
This study looked at nivolumab plus cabozantinib.3,5,6 This was for patients with ccRCC, any IMDC [International Metastatic RCC Database Consortium] risk, randomized to receive cabozantinib at 40 mg plus nivolumab. The nivolumab was given on [an every-2-week] schedule—and certainly it can be given on [an every-4-week] schedule—vs sunitinib.
[The primary end point was also PFS and] at the median follow-up of 18.1 months, showing a statistically significant improvement in PFS at 16.6 months vs 8.3 months, with HR of 0.51 [95% CI, 0.41-0.64; P < .001].5 Updated data from the 2021 American Society of Clinical Oncology Genitourinary Cancers Symposium at the 33-month median follow-up: the median PFS is at 16.6 months for the combination arm vs 8.3 months for the sunitinib arm with the HR holding steady at 0.56 [95% CI, 0.46-0.68].16
Were there any subgroups in this trial worth noting?
[There was a] subgroup analysis for PFS, looking at the region [patients were from]; IMDC risk including favorable, intermediate, and poor; PD-L1 status; age; gender; performance status; presence of bone metastases; and whether patients had a nephrectomy.5,6 Across all subgroups, PFS was favoring treatment with nivolumab/cabozantinib.
At the 33-month median follow-up, the median OS was at 37.7 months for the combination vs 34.3 months for sunitinib, with HR of 0.70 [95% CI, 0.55-0.90], and the 12-month landmark OS rate is at 70.3% compared with 60.3%, respectively.
The CR rate here was at 8% with a primary PD rate at 5.6%.3 The ORR is at almost 56% with the combination [95% CI, 50.1%-61.2%]. At the 33-month follow-up, the CR rate did increase from 8.0% initially to 12.4%. Some of these PRs converted into CRs with longer follow-up, and then the ORR holding steady at 55.7%.
The big point to highlight with AEs in this regimen is the rates of treatment discontinuation. The rates of somebody needing to discontinue either regimen at the initial data cutoff here was at 6.1%—very low rate of needing to discontinue this regimen, unlike the data we just saw. Treatment-related AE discontinuation rate at the 23.5-month follow-up for the [combination]—this was updated—was at 6.6%. That’s important, and the treatment-related AEs for grade 3 or higher at 65%, compared with 54% with sunitinib.
The major grade 3 or greater AEs to watch out for [from this study were] diarrhea [n = 6], hand-foot syndrome [n = 8], and hypertension [n = 11]. The grade 3 events are about on par with sunitinib; it’s just that there’s more grade 1/2 diarrhea, which is the big one [overall], and [aspartate aminotransferase] AST/ALT [alanine aminotransferase] elevation is something to keep considering.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Kidney cancer, version 4.2022. Accessed June 8, 2022. https://bit.ly/2TAx1m3
2. Choueiri TK, Hessel C, Halabi S, et al. Cabozantinib versus sunitinib as initial therapy for metastatic renal cell carcinoma of intermediate or poor risk (Alliance A031203 CABOSUN randomised trial): progression-free survival by independent review and overall survival update. Eur J Cancer. 2018;94:115- 125. doi:10.1016/j.ejca.2018.02.012
3. Powles T, Choueiri TK, Burotto M, et al. Final overall survival analysis and organ-specific target lesion assessments with two-year follow-up in CheckMate 9ER: nivolumab plus cabozantinib versus sunitinib for patients with advanced renal cell carcinoma. J Clin Oncol. 2022;40(suppl 6):350. doi:10.1200/ JCO.2022.40.6_suppl.350
4. Choueiri TK, Motzer RJ, Rini BI, et al. Updated efficacy results from the JAVELIN Renal 101 trial: first-line avelumab plus axitinib versus sunitinib in patients with advanced renal cell carcinoma. Ann Oncol. 2020;31(8):1030- 1039. doi:10.1016/j.annonc.2020.04.010
5. Choueiri TK, Powles T, Burotto M, et al; CheckMate 9ER Investigators. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829-841. doi:10.1056/NEJMoa2026982
6. Apolo AB, Powles T, Burotto M, et al. Nivolumab plus cabozantinib (N+C) versus sunitinib (S) for advanced renal cell carcinoma (aRCC): outcomes by baseline disease characteristics in the phase 3 CheckMate 9ER trial. J Clin Oncol. 2021;39(suppl 15):4553. doi:10.1200/JCO.2021.39.15_suppl.4553
7. Motzer R, Alekseev B, Rha SY, et al; CLEAR Trial Investigators. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289-1300. doi:10.1056/NEJMoa2035716
8. Grünwald V, Powles T, Kopyltsov E, et al. Analysis of the CLEAR study in patients (pts) with advanced renal cell carcinoma (RCC): depth of response and efficacy for selected subgroups in the lenvatinib (LEN) + pembrolizumab (PEMBRO) and sunitinib (SUN) treatment arms. J Clin Oncol. 2021;39(suppl 15):4560. doi:10.1200/JCO.2021.39.15_suppl.4560
9. Choueiri TK, Powles T, Porta C, et al. A phase 3 trial of lenvatinib plus pembrolizumab versus sunitinib as a first-line treatment for patients with advanced renal cell carcinoma: overall survival follow-up analysis (CLEAR study). Presented at: 2021 International Kidney Cancer Symposium; November 5-6, 2021; Austin, TX. Abstract E41.
10. Powles T, Plimack ER, Soulières D, et al. Pembrolizumab plus axitinib vs sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol. 2020;21(12):1563-1573. doi:10.1016/S1470-2045(20)30436-8
11. Rini BI, Plimack ER, Stus V, et al. Pembrolizumab (pembro) plus axitinib (axi) versus sunitinib as first-line therapy for advanced clear cell renal cell carcinoma (ccRCC): results from 42-month follow-up of KEYNOTE-426. J Clin Oncol. 2021;39(suppl 15):4500. doi:10.1200/ JCO.2021.39.15_suppl.4500
12. Albiges L, Tannir NM, Burotto M, et al. Nivolumab plus ipilimumab versus sunitinib for first-line treatment of advanced renal cell carcinoma: extended 4-year follow-up of the phase III CheckMate 214 trial. ESMO Open. 2020;5(6):e001079. doi:10.1136/esmoopen-2020-001079
13. Motzer RJ, Tannir NM, McDermott DF, et al. Conditional survival and 5-year follow-up in CheckMate 214: first-line nivolumab + ipilimumab (N+I) versus sunitinib (S) in advanced renal cell carcinoma (aRCC). Ann Oncol. 2021;32(suppl 5):S685-S687. doi:10.1016/j.annonc.2021.08.057
14. Rini BI, Powles T, Atkins MB, et al; IMmotion151 Study Group. Atezolizumab plus bevacizumab versus sunitinib in patients with previously untreated metastatic renal cell carcinoma (IMmotion151): a multicentre, open-label, phase 3, randomised controlled trial. Lancet. 2019;393(10189):2404-2415. doi:10.1016/S0140-6736(19)30723-8
15. Choueiri TK, Eto M, Kopyltsov E, et al. Phase III CLEAR trial in advanced renal cell carcinoma (aRCC): outcomes in subgroups and toxicity update. Presented at: ESMO Congress 2021; September 16-21, 2021; virtual. Accessed June 8, 2022. https://bit.ly/3b2v28K.
16. Motzer RJ, Choueiri TK, Powles T, et al. Nivolumab + cabozantinib (NIVO+CABO) vs sunitinib (SUN) for advanced renal cell carcinoma (aRCC): Outcomes by sarcomatoid histology and updated trial results with extended follow-up of CheckMate 9ER. J Clin Oncol. 2021;39(suppl 6):308. doi:10.1200/JCO.2021.39.6_suppl.308
Enhancing Precision in Immunotherapy: CD8 PET-Avidity in RCC
March 1st 2024In this episode of Emerging Experts, Peter Zang, MD, highlights research on baseline CD8 lymph node avidity with 89-Zr-crefmirlimab for the treatment of patients with metastatic renal cell carcinoma and response to immunotherapy.
Listen
Beyond the First-Line: Economides on Advancing Therapies in RCC
February 1st 2024In our 4th episode of Emerging Experts, Minas P. Economides, MD, unveils the challenges and opportunities for renal cell carcinoma treatment, focusing on the lack of therapies available in the second-line setting.
Listen
Conservative Management Is on the Rise in Intermediate-Risk Prostate Cancer
January 17th 2025In an interview with Peers & Perspectives in Oncology, Michael S. Leapman, MD, MHS, discusses the significance of a 10-year rise in active surveillance and watchful waiting in patients with intermediate-risk prostate cancer.
Read More
What Is Dark Zone Lymphoma, and Is It Clinically Relevant?
January 16th 2025Dark zone lymphoma includes aggressive B-cell lymphomas with shared molecular features. While some respond to escalated treatment, others remain resistant, highlighting the need for targeted approaches to improve outcomes.
Read More