Khan Reviews Later-Line Therapy Options for DLBCL With Subgroup Considerations
During a Targeted Oncology case-based roundtable event, Cyrus M. Khan, MD, discussed the data supporting the use of polatuzumab, bendamustine, and rituximab, tasfasitamab plus lenalidomide, and loncastuximab tesirine in patients with relapsed/refractory diffuse large B-cell lymphoma.
Cyrus M. Khan, MD
Hematologist
Allegheny Health Network Cancer Institute
Pittsburgh, PA

Targeted OncologyTM: What are the treatment options for patients with relapsed DLBCL?
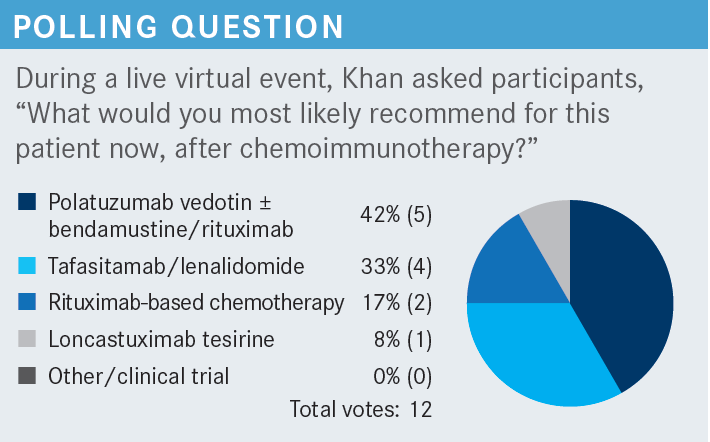
KHAN: The treatment options for these patients have expanded a lot over the last few years and gladly so. We’ve needed a lot of novel agents and treatments for patients, particularly in the older population and for high-risk patients.
According to the current NCCN [National Comprehensive Cancer Network] guidelines, second-line therapies for patients who are transplant eligible include a few salvage regimens. The most commonly used is R-ICE [ifosfamide, carboplatin, and etoposide ± rituximab], followed by GDP [gemcitabine, dexamethasone, and cisplatin or carboplatin ± rituximab] and DHAP [dexamethasone, cytarabine + carboplatin, cisplatin, or oxaliplatin ± rituximab]. Other recommended regimens are ESHAP [etoposide, methylprednisolone, cytarabine, and cisplatin ± rituximab], GemOx, and MINE [mesna, ifosfamide, mitoxantrone, and etoposide ± rituximab].1
Then of course for patients who are not transplant candidates, the preferred regimens include GemOx plus rituximab, pola-BR [polatuzumab vedotin-piiq (Polivy) with bendamustine (Treanda) and rituximab], and tafasitamab-cxix [Monjuvi] plus lenalidomide [Revlimid]. There are a few other recommended regimens as well. Finally, there are some regimens that are not FDA approved yet but can be useful in certain circumstances. For example, ibrutinib [Imbruvica] and R2 [lenalidomide and rituximab] are recommended for non-GCB [germinal center B-cell–like] DLBCL subtypes, and brentuximab vedotin [Adcetris] can be used for CD30-positive disease.1
For CAR [chimeric antigen receptor] T-cell therapy regimen options, it is important to control the disease a bit before collecting the MNCs [mononuclear cells]. Then there are a few options including GDP, ICE, GemOx, and pola-BR.1
Typically what we’ve done as a bridge therapy is pola alone because we know bendamustine is T-cell depleting, so you might have some problems during collection with pola-BR. GemOx is also a common bridging regimen. For eligible patients, an allogeneic hematopoietic cell transplant may be considered as consolidation post second-line therapy,1 and pretty tough disease control is needed.
There’s not a great graft-vs-lymphoma effect in DLBCL, so not an easy process for those patients. Then for third-line and subsequent therapy, we have 3 approved anti-CD19 CAR T-cell therapies: axi-cel [axicabtagene ciloleucel (Yescarta)], lisocabtagene maraleucel [Breyanzi], and tisagenlecleucel [Kymriah]. Loncastuximab tesirine [lonca (Zynlonta)], a monoclonal antibody-drug conjugate targeting CD19, is also an option, as well as selinexor [Xpovio], a selective nuclear export blocker.1
What data support the use of these options for patients with DLBCL after chemoimmunotherapy?
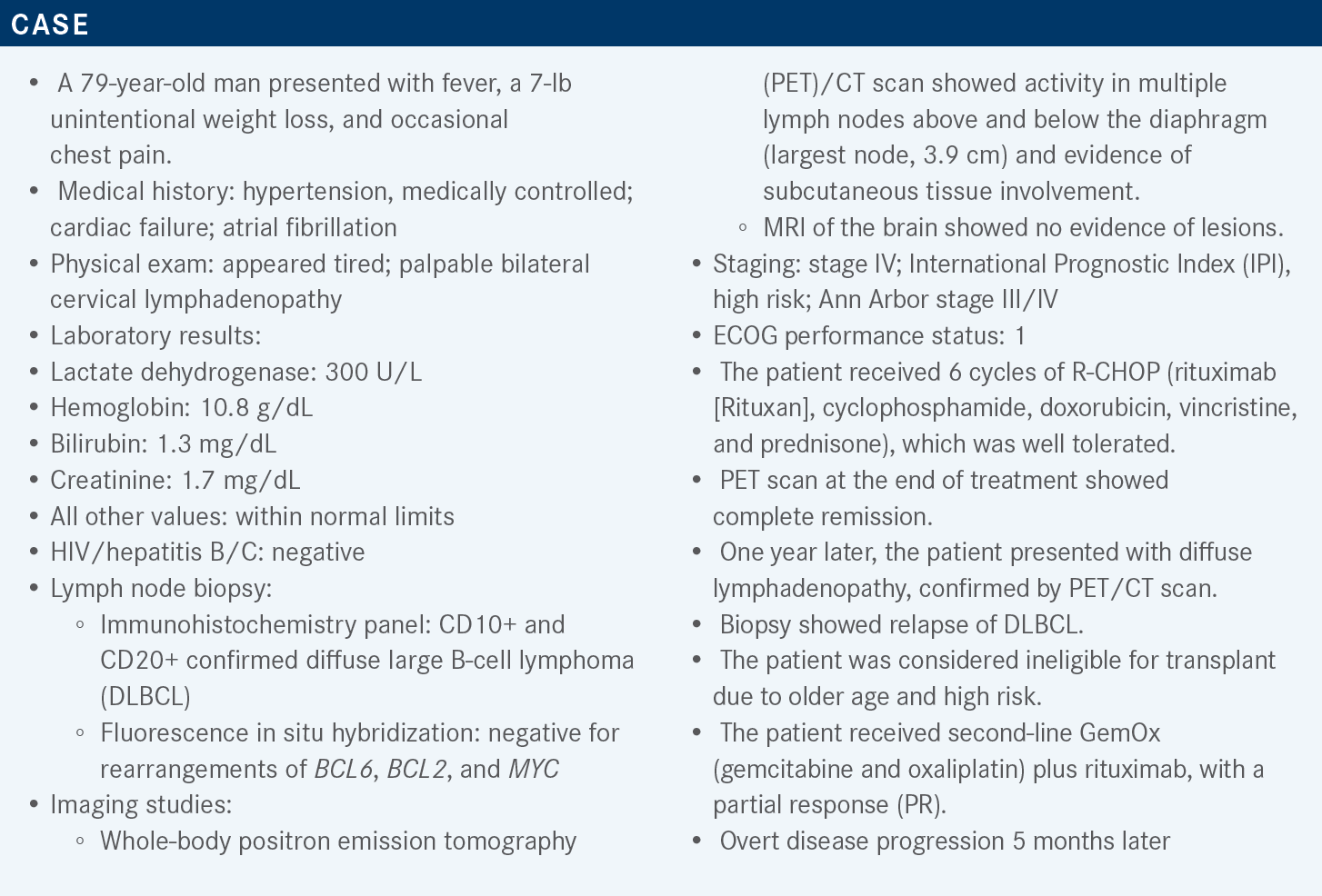
There are multiple studies investigating this question. For example, the phase 2 pola-BR study [NCT02257567] included a phase 1b safety run-in [n = 6], followed by randomized cohorts—pola-BR [n = 40] vs BR [n = 40]— and a single-arm pola-BR extension (n = 106) cohort for patients with relapsed or refractory [R/R] DLBCL. The idea was to investigate whether pola-BR worked together and whether the combination was toxic.2,3
An important point to note is that we have so many different novel agent combinations. Not all of them are equal and unfortunately none of them have been compared to each other, so we can’t compare across trials. On the other hand, at least whenever you have a patient, you can put them on a treatment that probably was reflected in one of the latest clinical trials.
Adult patients, aged 18 years or older, with biopsy-confirmed R/R DLBCL and an ECOG performance status score between 0 and 2 had to be transplant ineligible or have had treatment failure with prior transplant and have received at least 1 prior line of therapy to meet the inclusion criteria for this study.2,3 However, if patients underwent a prior allogeneic stem cell transplant, an autologous stem cell transplant within 100 days prior to cycle 1 day 1, had a history of transformed disease, grade 1 or higher peripheral neuropathy, or were eligible for an autologous transplant, then they were excluded from this study.
Pola-BR given is every 21 days for 6 cycles only. The polatuzumab dose is 1.8 mg/kg, and is given on day 1; the bendamustine dose is 90 mg/mg2 given by intravenous [IV] infusion on days 1 and 2, and the rituximab dose was the standard [375 mg/m2 on day 1 of each cycle].2,3 Remember that in all other lymphomas, we generally give BR every 28 days, however, in DLBCL the dosing is every 21 days. Polatuzumab is an antibody-drug conjugate against CD79B,2,3 and the active chemotherapy is monomethyl auristatin E, the same regimen used in brentuximab vedotin.
In the pooled data analysis [n = 152], the median age was 69 years, with a range of 24 to 94 years. Almost all patients had high-stage disease, with a median of 2 prior lines of therapy [range, 1-7]. There was an even distribution of percentage of patients with 1, 2, or [greater than or equal to] 3 prior lines of therapy. Most of the patients had a quick relapse [with duration of response (DOR) to their last treatment 12 months or less], and a lot of them were refractory to the last prior therapy. Some patients [18%] had a prior transplant, and 39% had a germinal center subtype. The median time to first response was 2 months [range, 1.8-5.3].2,3 This is sort of reflective of what we see in our clinics.
The independent review committee [IRC] assessed objective response in the randomized arm was 45% in the pola-BR cohort vs 17.5% in the BR cohort. So based on these results, naturally polatuzumab was added in the extension arm, which had an IRC overall response rate [ORR] of 41.5%, including complete responses [CRs] and PRs.2,3
The median IRC DOR was similar for the randomized and extension cohorts, at 10.9 months for the pola-BR arm, 10.6 [months] for the BR arm, and 9.5 months for the extension cohort. The median progression-free survival [PFS] was 9.2 months for pola-BR, only 3.7 months for BR, and 6.6 months for the extension cohort. The median follow-up was 48.9 months for pola-BR, 48.3 months for BR, and 15.2 months for the extension cohort.3
So quite a bit of follow-up. The median overall survival [OS] was 12.4 months in the pola-BR group vs 4.7 months only in the BR group. In the pola-BR extension cohort, the median OS was 12.5 months.3 That is about a year’s worth of survival for these patients. Again, these patients are beat up and have gone through a lot. Remember that in the SCHOLAR trial that came before all these newer agents, the median survival was about 6 months,4 so at least all these newer agents have incrementally improved upon the survival that we had historically.
As far as [adverse] events [AEs] are concerned, I think the general flavor that we get from pola-BR is cytopenias. So about half the patients [46.2%] experienced grade 3/4 neutropenia, 41% had thrombocytopenia, and 10.3% had febrile neutropenia, even in the BR arm.3
I think this is more a function of bendamustine. Then a few gastrointestinal [GI] issues that were mostly lower grade. There were also some cases of peripheral neuropathy, which can be caused by polatuzumab, but it was mostly all grades with no grade 3/4 events. The pola-BR group had a 33% discontinuation rate compared [with] only 10% in the BR group. In the pola-BR group, 13% of dose reductions were of BR and only 5% reductions of pola.3 So things that you might see if you used this regimen would likely be cytopenias and perhaps lower-grade neuropathy.
Have you used tafasitamab plus lenalidomide?
Tafasitamab is an Fc-enhanced anti-CD19 monoclonal antibody. Obviously, we’ve had CD20 monoclonal antibodies for a long time. The first anti-CD19 treatment was blinatumomab [Blincyto] for B-cell ALL [acute lymphoblastic leukemia]. We now have more antibodies against CD19, which is a good target to use because it’s underutilized in the frontline and perhaps even the second-line setting.
[Although] there was an increase in antibody-dependent toxicity and phagocytosis, there was also direct cell death and some encouraging activity in [patients with] NHL [non-Hodgkin lymphoma], leading to the approval of tafasitamab for indolent lymphomas.5,6 This was followed by studies of the combination of tafasitamab with lenalidomide, which has efficacy in some of these patients; there was T-and NK [natural killer]–cell activation and expansion, as well as direct cell death.6
This combination was further evaluated in the phase 2, single-arm, open-label, multicenter L-MIND trial [NCT02399085]. Eligible patients had to have had 1 to 3 prior lines of therapy, and transplant-eligible and primary refractory patients were excluded from this trial.6
Tafasitamab was given at a 12 mg/kg weekly for cycles 1 through 3. There was another infusion of a loading dose of tafasitamab on day 4 of the first week, but then it was just weekly infusions for the 3 cycles. For cycles 4 to 12, tafasitamab was given every 2 weeks. Lenalidomide was administered at 25 mg per day for 3 weeks [days 1-21], followed by a week off for 1 year. At the end of the year, if patients have stable disease or better, lenalidomide falls off and patients continue with maintenance tafasitamab every 2 weeks until progression or toxicity-related discontinuation.6
The median age was 72 years [range, 41-86]. About half the patients had a lower IPI risk score, and most [75%] had stage III to IV disease. The median prior therapy line was 2 [range, 1-4], with most [93%] having had 1 or 2 prior lines of therapy and not many [7%] having had 3 to 4. A minority of patients [19%] had primary refractory disease, about half were refractory to the last prior line of therapy, 11% received a prior transplant, and 10% had GCB.6
At the 35-month follow-up, 40% had a CR, 17.5% a PR, and 16.3% each had SD [stable disease] and PD [progressive disease]. The ORR [overall response rate] was 57.5%, with quite a good median DOR of 43.9 months. The median time to response was 2.1 months.7
The subgroup analysis showed similar responses. The Ann Arbor stage or age made no difference. Patients with low and low-intermediate IPI risks scores had slightly better responses than patients with higher IPI risk scores, which makes sense. Patients with a non-GCB phenotype had a better response.7 This is probably due to lenalidomide. Non-GCB patients are dependent on the B-cell receptor pathway, and lenalidomide downregulates NF-κβ [nuclear factor–κβ] and other pathways and has activity in the ABC subtype.
The response was 71% vs 49% for the patients with a GCB phenotype, respectively. There was not much difference based on refractoriness to rituximab, last line, and primary refractory disease. Patients with only 1 prior line of therapy had a 70% response rate vs 50% for patients with at least 2.7 So there are a few trends emerging, which help us choose the right regimen for patients.
The median PFS at a median of 33 months of follow-up was 11.6 months, and the median OS at a median of 42.7 months of follow-up was 33.5 months. PFS was best for patients who achieved a CR. When that was not reached, the median PFS was 7.4 months for patients with a PR and 2.1 months for patients who were progressing very poorly. Same thing for OS, NR for the complete responders, and almost 2 years [22.5 months] for partial responders.7 For those that it works for, it works very well and for quite some time. Pretty useful regimen for some patients at least.
There were some hematologic AEs, with the most common being neutropenia, anemia, and thrombocytopenia. In particular, 27% of patients had grade 3 neutropenia and 21% had grade 4. Some patients have a febrile neutropenia risk, about 10% with grade 3 and 2% grade 4.6
That is generally from lenalidomide, especially in the beginning. Those who have used it can probably appreciate the neutropenia that can be seen in the first few cycles. Growth factor and antimicrobial prophylaxis can be done for these patients. Another option is dose reductions; 25 mg/day can be a pretty hefty dose for some patients with DLBCL, perhaps older patients, heavily pretreated, if they have marrow infiltration.
The most common nonhematologic AEs were fatigue, GI issues, cough, pyrexia, peripheral edema, urinary tract infection, and decreased appetite.6 But there weren’t many grade 3 and 4 [AEs]. The only thing that generally we look for is cytopenias in the beginning. Even infusion reactions, not that many patients have it. In fact, you don’t even have to give the premeds if they haven’t had an infusion reaction by infusion No. 3.
The rate of serious AEs was 51%, and that of treatment-related discontinuation was 12%. The rate of TEAEs [treatment-emergent AEs] leading to death was 13%. Almost half of patients [45.7%] had at least 1 dose reduction of lenalidomide, perhaps from the neutropenia. About two-thirds of the patients [77.5%] were able to continue on the 20-mg per day lenalidomide dose.
Neutropenia is the main AE, with grade 3/4 events during the tafasitamab-and-lenalidomide combination phase, up to 12 cycles, with a median exposure of 6.5 months. In the next phase, patients go on to tafasitamab monotherapy [n = 37]. The median exposure for the extension group was 8.7 months. During this phase, there is neutropenia as well as other issues, but not as robust as in the beginning.6
How do you use loncastuximab tesirine for your patients?
All responders have never used it, which makes sense [because] this is an even newer regimen than the other ones that we discussed. Lonca is another anti-CD19 drug conjugate. The CD19 antibody delivers SG3199, a cytotoxic DNA minor groove interstrand crosslinking a PBD [pyrrolobenzodiazepine] dimer payload as the inhibitor.8
[Supporting data come from] the single-arm, phase 2 LOTIS-2 clinical trial [NCT03589469]. The eligibility criteria were similar to the previous studies [discussed]: adult patients with R/R DLBCL with at least 2 previous lines of therapy; a biopsy to show that the patient was still CD19 positive if a prior anti-CD19 therapy was used; ECOG performance status of 0 to 2; transplant-eligible patients were allowed; patients who received an autologous stem cell transplant 30 days prior or an allogeneic stem cell transplant 60 days prior were also permitted to enroll.8
This is a single-agent drug. The first 2 cycles were given at a 0.15-mg/kg dose. Afterward and up to cycle 12—a 1-year treatment—the dose was 0.075 mg/kg. Follow-up was done for 3 years.8
The median age was 66 [range, 56-71], and most of the patients had DLBCL. Hybrid B-cell lymphoma was allowed, so patients with double- and triple-hit disease were allowed in this trial, including double/triple expressors [14%], double/triple hit [10%], and 20% had transformed disease. Two-thirds of the patients [77%] had stage III or IV disease, 33% had a GCB phenotype, and 67% had either non-GCB or other phenotype. Patients had 2 [43%], 3 [24%], or more than 3 [32%] prior lines of therapy. In terms of treatment history, 68% had relapsed after the first line of therapy and 17% were refractory to all prior lines of therapy.
About a quarter of enrolled patients [25%] had received prior transplant therapies, of which 9% had CAR T-cell therapy prior to receiving Lonca on this trial.8 This was one of the first anti-CD19–directed therapies used after CAR T, so we can appreciate how those responses might have been. From a total of 145 patients, the ORR was 48% [95% CI, 39.9%-56.7%], 24 patients each for CRs and PRs. The median time to first response was 41 days [IQR, 38-44], so pretty quick. Of the 35 CRs, 57% had maintained the CR at data cutoff, so we’ll have newer data going on longer. Most responders had a response by 2 cycles, and the median [number of] cycles was about 4.5.8
The most updated median DOR was 13.4 months. For the patients who were in CR, the median DOR had not been reached, while at the time of the initial data cutoff, it was 13.4 months. Patients with CRs do pretty well as far as the curves are concerned.9
In the subgroup analysis, there are a few trends emerging. Patients with transformed or de novo disease responded almost equally. There were some differences between patients who had double- or triple-hit disease compared with those who did not, but patients did respond pretty well, even if they had transformed disease. Cell of origin and expression didn’t really matter. Even the hybrid B-cell lymphomas responded too, which is a particularly difficult population to study, as we’ve all experienced.
Most of the patients with R/R status after the first, last, or any lines did well. Another important feature was whether prior transplant and CAR-T therapy made a difference in response. Prior transplant and CAR-T therapy also didn’t seem to matter, so pretty good addition to our armamentarium for treatment of these particularly problematic patients that can be useful in a lot of these situations.9
What is interesting in this study is that patients were tracked even if they continued on to later lines of therapy, including 15 patients who received CD19-directed CAR-T therapy with an ORR of 46.7% and 9 who received stem cell therapy as consolidation.8,9 You can certainly take patients to CAR T even after receiving loncastuximab, and stem cell transplant can obviously be used to stabilize the disease. These subsequent treatments not only can improve lead progressive treatments, but can also serve as a segue into further lines of therapy for some patients.
Challenging subgroups include high-grade [HG]BCL and post–CAR-T therapy. As far as HGBCLs are concerned, 11 patients had CR. Compare that to the [patients with] DLBCL, 24.4% had a CR, and 26% had a PR. Again, pretty good responses for those patients. Time to first response was similar between the 2 groups [approximatley 40 days]. However, HGBCL took longer to get to a CR, approximately double the time than that for [patients with] DLBCL.
For patients who went on Lonca after CAR T-cell therapy relapse [n = 13], the response to CAR T-cell therapy was about 54% CRs, 15% PRs, and 30% no response. These patients then went on to receive Lonca after CAR T-cell therapy, and [about 45% achieved either a CR or PR].9 The most common AEs were B-cell neutropenia [26.2%], thrombocytopenia [17.9%], GGT [γ-glutamyl transferase] increase [17.2%], and some anemia [10.3%]. Treatment discontinuation occurred in about 17.9% of patients, and most commonly was either because of surface edema, localized edema, or GGT increase. There was no increased toxicity in the older population, which is why dexamethasone [4 mg twice a day] is generally given as a premedication [a day before loncastuximab], and patients shouldn’t go out in the sun either.
Treatment delays and dose adjustments were allowed. Patients with weight gain of more than 1 kg from day 1 of cycle 1 or with edema/pleural effusions received standard doses of spironolactone. Peripheral edema was seen in about 16% of the patients, with not much difference [seen] between patients [older than] 65 years and those [younger than] 65 years.8
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. B-cell lymphomas, version 4.2021. Accessed June 6, 2021. https://bit.ly/3geoS5N
2. Sehn LH, Herrera AF, Flowers CR, et al. Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma. J Clin Oncol. 2020;38(2):155-165. doi:10.1200/JCO.19.00172
3. Sehn LH, Hertzberg M, Opat S, et al. Polatuzumab vedotin plus bendamustine and rituximab in relapsed/refractory DLBCL: survival update and new extension cohort data. Blood Adv. 2022;6(2):533-543. doi:10.1182/ bloodadvances.2021005794
4. Crump M, Neelapu SS, Farooq U, et al. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood. 2017;130(16):1800-1808. doi:10.1182/blood-2017-03-769620
5. FDA grants accelerated approval to tafasitamab-cxix for diffuse large B-cell lymphoma. FDA. Updated August 3, 2020. Accessed June 16, 2022. https:// bit.ly/3b8A5nT
6. Salles G, Duell J, González Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988. doi:10.1016/S1470-2045(20)30225-4
7. Duell J, Maddocks KJ, González-Barca E, et al. Long-term outcomes from the phase II L-MIND study of tafasitamab (MOR208) plus lenalidomide in patients with relapsed or refractory diffuse large B-cell lymphoma. Haematologica. 2021;106(9):2417-2426. doi:10.3324/haematol.2020.275958
8. Caimi PF, Ai WZ, Alderuccio JP, et al. Loncastuximab tesirine in relapsed or refractory diffuse large B-cell lymphoma (LOTIS-2): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6):790-800. doi:10.1016/ S1470-2045(21)00139-X
9. Caimi P, Ai WZ, Alderuccio JP, et al. Duration of response to loncastuximab tesirine in relapsed/refractory diffuse large B-cell lymphoma by demographic and clinical characteristics: subgroup analyses from LOTIS 2. J Clin Oncol. 2021;39(suppl 15):7546. doi:10.1200/JCO.2021.39.15_suppl.7546
Gasparetto Explains Rationale for Quadruplet Front Line in Transplant-Ineligible Myeloma
February 22nd 2025In a Community Case Forum in partnership with the North Carolina Oncology Association, Cristina Gasparetto, MD, discussed the CEPHEUS, IMROZ, and BENEFIT trials of treatment for transplant-ineligible newly diagnosed multiple myeloma.
Read More