McCloskey Explores Merits of Targeted Treatments and HMAs in MDS
The options for targeted therapy and treatment with hypomethylating agents was discussed during a virtual Case Based Peer Perspectives event, which highlighted the case of a 75-year-old male patient with myelodysplastic syndromes. The discussion was led by James K. McCloskey II, MD.
The options for targeted therapy and treatment with hypomethylating agents was discussed during a virtual Case Based Peer Perspectives event, which highlighted the case of a 75-year-old male patient with myelodysplastic syndromes (MDS). The discussion was led by James K. McCloskey II, MD, a medical oncologist, Division of Leukemia, Adult Blood and Marrow Stem Cell Transplantation Program, John Theurer Cancer Center, at Hackensack Meridian Health.
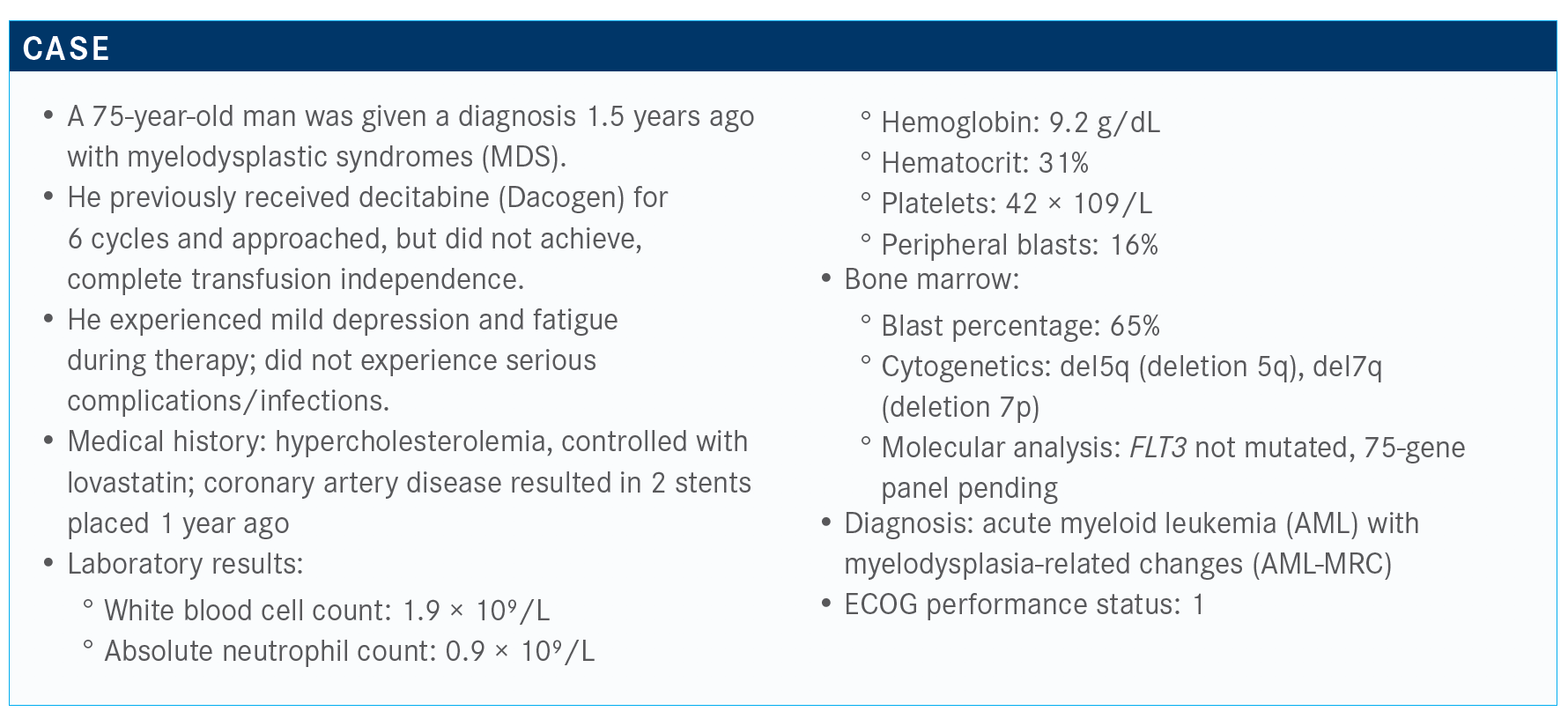
Targeted Oncology™: What are the treatment regimens for the patient who isn’t a candidate for induction therapy, according to the National Comprehensive Cancer Network (NCCN) guidelines?
MCCLOSKEY: For patients who are not candidates for induction therapy, the NCCN suggests venetoclax [Venclexta] in combination with HMA [hypomethylating agents] or LDAC [cladribine plus low-dose cytarabine], HMA alone, glasdegib [Daurismo] in combination with LDAC, LDAC alone, and Mylotarg [gemtuzumab ozogamicin].¹
What was the rationale for developing the liposomal combination of daunorubicin and cytarabine (Vyxeos) for this patient population?
This is a liposomal formulation of daunorubicin and cytarabine. I think the take-home point [regarding] the design of the drug is that the mechanism of action does not promote less toxicity but more effectiveness.
In preclinical models, we [found] that if we can administer anthracycline and cytarabine specifically in a 1:5 ratio, this is when we get the most potent antileukemic effect. The drug was designed to deliver that ratio and maintain that ratio in circulation.
The drug was approved based on a phase 3 randomized study [NCT01696084] that evaluated newly diagnosed patients with either treatment-related or secondary AML.² These were…
patients between the ages of 60 and 75. The patients were deemed fit for intensive therapy, so their ECOG performance status was 0 to 2.
For this case, the patient’s cardiac events are concerning, although we don’t know the circumstances under which he underwent stent placement. Otherwise, he’s fitting into this
category of patient. He specifically had MDS with prior HMA exposure. He’s 75, [which is] the upper age limit for patients in the study.
In this phase 3 trial, patients were randomized into treatment either with CPX-351 [n = 153] or 7 + 3 [n = 156]. They then were followed for treatment response. The patients who achieved a
remission at any point and were eligible for transplant proceeded to transplant. Patients who failed to respond could receive salvage therapy. And those patients who achieved a response could go on to consolidation. At any point during the trial, patients could proceed to transplant.
An important consideration is that patients did not receive HiDAC [high-dose cytarabine] consolidation. They received 5 + 2, which is a European approach to treatment.
The FDA recommended the dosing description for the agent be 44 mg of daunorubicin and 100 mg/m² of cytarabine. This formulation emphasizes the presence of the anthracycline.
What was the approval of this regimen based on?
The drug was approved based on overall survival data and investigators reported improved CR [complete response] rates. In the trial, 37% of patients experienced CR in the Vyxeos arm
compared with 25% of patients in the control arm. If you consider CRis [complete remission with incomplete hematologic recovery], that’s 47% for the Vyxeos arm compared with 33% for the control arm.
This did result in improved overall survival. Overall survival in the Vyxeos arm was 9.56 months compared with 5.95 months in the standard of care arm 7 + 3 [HR, 0.69; P = .003]. Patients who
were treated with Vyxeos achieved the survival benefit whether they were in the older age group, between 70 and 75, or patients under the age of 75. Even those older patients did receive the
survival benefit.
How does this affect consolidation and transplant?
If we follow the data out, it appears that Vyxeos improved outcomes both during consolidation with chemotherapy but also with patients who proceeded to stem cell transplant.³
I think it’s important to note that this is post hoc analysis of the data, so these weren’t predefined groups. They were biased by the fact that these are responders.
Survival for patients who underwent consolidation with Vyxeos was 25 months compared with 8.5 months for 5 + 2. As we start to look at those patients who responded, we really see a significant benefit there. Looking at the impact [of Vyxeos] on transplant, among the patients who had a transplant, investigators reported more success getting folks to transplant in the
Vyxeos arm: 49 patients in the Vyxeos arm compared with 32 patients in the control arm.
For patients who went to transplant in remission, it didn’t matter which treatment regimen they received. The patients who received Vyxeos appeared to do better, with a median overall survival of 24 months compared with 12 months.
How does the safety profile of Vyxeos compare with standard induction?
I think most of the toxicities reported with Vyxeos are similar to what we expect to see with induction. In fact, the toxicities across the board are comparable, with no significant difference
in cardiac toxicity and similar rates of infectious complications despite a delayed count recovery.
As you know, Vyxeos does often come with the downside of having delayed count recovery, but interestingly, we did not see increased risk of death from infection during that time. In terms of serious adverse effects, these 2 regimens are similar.
How was the dose for venetoclax determined?
The phase 1 study [NCT02203773] led by Dr DiNardo and colleagues evaluated venetoclax up to 800 mg in combination with both decitabine and Vidaza [azacitidine].⁴ It’s important to note that all the patients in the trial were HMA naïve.
We did recently receive notice that the phase 3 data, published in Blood, which evaluated venetoclax plus azacitidine versus azacitidine alone, did meet its primary end point.⁵ What was striking was the remarkable response rate. For the elderly patient population who are unfit for transplant, the CR and CRi rates were 60% or 70%.
In terms of toxicity, there were few grade 3 and 4 toxicities, and not as many issues as we saw with the induction therapy that I previously mentioned.
But there were some concerns: 32% rate of febrile neutropenia, 12% pneumonia, 10% bacteremia. These occurred in a patient population that was less fit than the folks we just discussed and a little older in general.
What treatment options are available for patients with AML and high-risk MDS?
You might consider glasdegib, which we evaluated in clinical trials. We have used this in limited numbers of patients following the drug’s approval.
"We did recently receive notice that the phase 3 data, published in Blood, which evaluated venetoclax plus azacitidine versus azacitidine alone, did meet its primary end point. What was striking was the remarkable response rate. For the elderly patient population who are unfit for transplant, the CR and CRi rates were 60% or 70%.” –James K. McCloskey II, MD
If you’re not familiar with glasdegib, it’s an inhibitor of the hedgehog pathway that targets the leukemia stem cell. It was studied in the BRIGHT study [NCT01546038].⁶ This was a phase
2 randomized trial of patients with AML and high-risk MDS. Patients were randomized to either LDAC alone or LDAC in combination with glasdegib in a 2-to-1 fashion.d in the BRIGHT study [NCT01546038].⁶ This was a phase 2 randomized trial of patients with AML and high-risk MDS. Patients were randomized to either LDAC alone or LDAC in combination with glasdegib in a 2-to-1 fashion.
The trial did include patients who had prior exposure to HMAs and, in fact, a substantial portion of these patients had been treated previously with HMA. The drug was approved based on the survival data around the same time as venetoclax. So glasdegib plus LDAC yielded an 8.8 months overall survival compared with LDAC alone for 4.9 months. I think as you start to get into the nitty-gritty of things, now that we have a lot of options in AML, there was a difference in
response based on cytogenetic risk stratification.
Patients with good and intermediate risk exhibited a more significant response, a better improvement in overall survival, 12 months compared with 4.8 months in the LDAC arm [HR, 0.427; 80% CI, 0.300-0.609; P = .0008].⁵ Patients with high-risk MDS and AML had a blunted response. Median OS for glasdegib was 4.7 months compared with 4.9 months for LDAC arm [HR, 0.633; 80% CI, 0.430-0.934; P = .0640].
The response data for glasdegib were not as impressive compared with venetoclax responses that I discussed earlier. The investigators reported a CR rate of 17% and CRi rate of 6.5%. They reported an overall response rate of 26% compared with 5% for LDAC alone. And I think that this is a good point to consider as we look at new agents for AML. It’s always a point of conversation, especially in these older, more frail patients. How do we consider both a survival benefit and
CR rate in a more elderly patient? If they could live with their disease and be relatively symptom-free, how important is that CR?
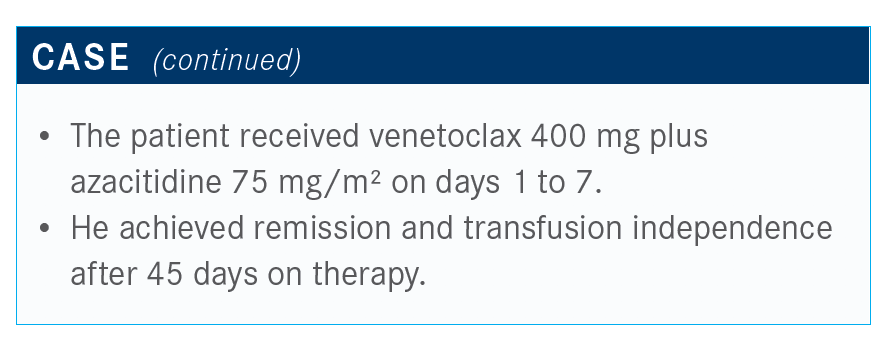
For this patient, is HMA still a consideration?
The patient was treated with venetoclax in combination with azacitidine. If the investigators followed the clinical trial regimen, this patient would not have been eligible for HMA.
But I think certainly, like many, depending on the patient and how much HMA they have received, we might consider still using HMA in combination with venetoclax as a salvage therapy. And the patient does have a response with a remission and is transfusion independent after 45 days on treatment.
Would you consider a bone marrow transplant for him?
We tend to use bone marrow transplants quite frequently, I think, because in our experience, almost all of these patients have very serious cytopenias eventually. We have found it helpful to do bone marrow transplants to document a response. However, if you have a patient who is doing great [and] the counts are beautiful, then maybe not.
Maybe that bone marrow transplant is not as helpful if the patient has had a full hematologic response. In general, our experience has been that many of these patients, especially like this patient we’re discussing, they’re likely to end up cytopenic at the end of their first cycle of treatment. And so then we’re left really scratching our heads. Are they cytopenic because there is disease in the bone marrow? Or are they cytopenic because they’re aplastic?
References:
1. NCCN Clinical Practice Guidelines in Oncology. Acute myeloid leukemia, version 3.2020. NCCN. Accessed July 29, 2020. https://bit.ly/3jSYRs3
2. Lancet JE, Uy Gl, Cortes JE, et al. Final results of a phase III randomized trial of CPX-351 versus 7+3 in older patients with newly diagnosed high risk (secondary) AML. J Clin Oncol. 2016;34(suppl 15):7000. doi: 10.1200/JCO.2016.34.15_suppl.7000
3. Kolitz JE, Strickland SA, Cortes JE, et al. Consolidation outcomes in CPX-351 versus cytarabine/daunorubicin-treated older patients with high-risk/secondary acute myeloid leukemia. Leuk Lymphoma. 2020;61(3):631-640. doi:10.1080/10428194.2019.1688320
4. Dinardo CD, Pratz KW, Potluri J, et al. Durable response with venetoclax in combination with decitabine or azacitidine in elderly patients with acute myeloid leukemia (AML). J Clin Oncol. 2018;36(suppl 15):7010. doi:10.1200/JCO.2018.36.15_suppl.7010
5. DiNardo CD, Pratz K, Pullarkat V, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019;133(1):7-17. doi:10.1182/blood-2018-08-868752
6. Cortes JE, Heidel FH, Hellmann A, et al. Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemiaor high-risk m yelodysplastic syndrome. Leukemia. 2019;33(2):379-389. doi:10.1038/s41375-018-0312-9

Survivorship Care Promotes Evidence-Based Approaches for Quality of Life and Beyond
March 21st 2025Frank J. Penedo, PhD, explains the challenges of survivorship care for patients with cancer and how he implements programs to support patients’ emotional, physical, and practical needs.
Read More