Ganguly Details Treatments for Standard-Risk Multiple Myeloma
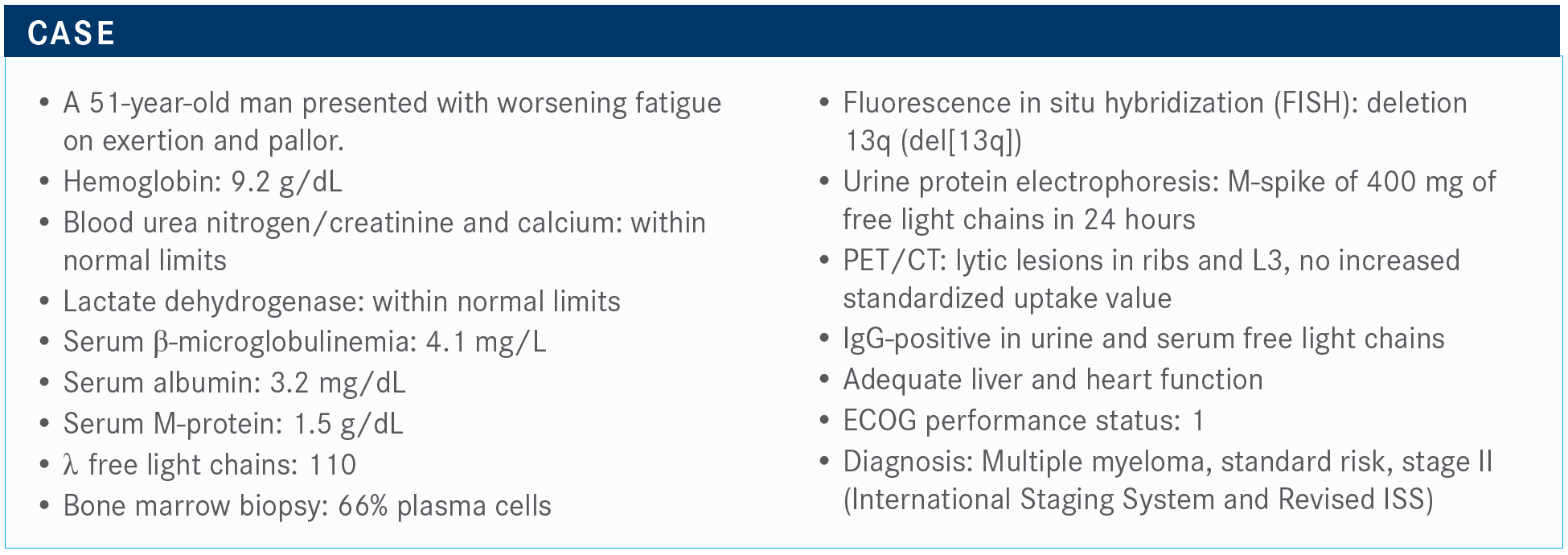
Siddhartha Ganguly, MD, reviewed the case of a 51-year-old man with standard-risk multiple myeloma.
Siddhartha Ganguly, MD

Siddhartha Ganguly, MD, professor of Medicine, deputy director, Hematologic Malignancies and Cellular Therapeutics, director, Lymphoma/Myeloma Program, University of Kansas Medical Center, Kansas City, KS, reviewed the case of a 51-year-old man with standard-risk multiple myeloma.
Targeted Oncology™: What proportion of patients with newly diagnosed multiple myeloma are young, fit, and transplant-eligible?
GANGULY: It is in the eye of the beholder. [We owe it to] every patient to be referred at least 1 time to a transplant physician to be told [whether they are transplant-eligible].
I have transplanted [patients who are] up to 81 years old, so age is not a barrier. We can go to transplant, especially when we know trial after trial has shown that transplant improves, definitively, progression-free survival [PFS] and sometimes even overall survival. We would refer most of the patients to a transplant center.
Unfortunately, that is not the landscape of the United States. We need to improve the health access and delivery, and [we need to] address disparities [in who receives referrals].
What therapy regimens would you consider for use in this patient?
I would like to stick to the category 1 [regimens outlined in the National Comprehensive Cancer Network guidelines], and that is RVd [lenalidomide (Revlimid), bortezomib (Velcade), and dexamethasone].1 In certain situations, I would say CyBorD [cyclophosphamide, bortezomib, dexamethasone] also is an option, especially in patients with renal failure and amyloidosis. If I had a patient admitted to the hospital [who] had a problem getting Revlimid approved, I would maybe start with CyBorD and then change it over to RVd when we have the medicine approved.
Would you consider using daratumumab (Darzalex) in the upfront setting?
Daratumumab [dara] as an upfront therapy is only approved with a dara-VTd [bortezomib, thalidomide (Thalomid), and dexamethasone], and I don’t think that we use it in the United States.. Dara-VTd is approved for transplant-eligible patients, but I don’t think that anybody uses it. For [patients who are] really sick, I’ve used a VTd base, especially in a plasma cell leukemia.
Can you summarize findings that have led to the use of standard therapy options in a transplanteligible patient?
The well-known IFM/DFCI2009 [NCT01191060], is the trial between RVd followed by transplant or RVd with a delayed transplant. It clearly showed improved PFS [for] the transplant side [0.65; P < .001].3 The FORTE trial [NCT02203643] did not show any major difference between KRd [carfilzomib (Kyprolis), lenalidomide, dexamethasone] plus transplant versus KRd for 12 cycles [KRd12],4 but it does have some nuances that I will discuss. CASSIOPEIA [NCT02541383] is a trial of dara-VTd versus VTd, but I don’t use it in my practice.2
The GRIFFIN trial [NCT02874742] is the most recent [trial involving daratumumab],5 and this may be a game changer in the future for our patients with newly diagnosed multiple myeloma that is high risk.
Just a summary for IFM/DFCI2009, [in] patients who receive the RVd alone and then continued on the RVd and lenalidomide maintenance compared with RVd and early transplant, the complete response [CR] rate was higher in the transplant group, 59% versus 48%. Minimal residual disease [MRD] was much higher with the transplantation compared to the nontransplantation [79% vs 65%].3
What is the importance of MRD in this setting?
MRD is important; we all practice by MRD. You can clearly see patients who attained MRD negativity at the start of the maintenance; and 1 year after maintenance, they maintained the PFS far better than patients who were MRD positive.
That is a debate that is raging right now. Unless someone shows me strong data that MRD negativity—and persistence of the MRD negative, which is a better predictor than [a single] snapshot of an MRD negativity—I have no data to suggest not to take them to the transplant or to stop the maintenance. Even with MRD-negative patients, there is no plateau.
What data for carfilzomib in patients who are transplant eligible changed your mind about using RVd?
The efficacy between the KRd-transplant versus KRd12 are pretty much equivalent [according to results of the FORTE trial].4 In certain situations, I would recommend [using it]. In those patients who were in the KRd12 arm and followed to early relapse, losing MRD negativity was far higher than with KRd-transplant, again bringing us to the point that a [single] snapshot of MRD negativity is probably not giving you the whole picture. It is a persistence of the MRD negativity that is more important.
The ASCO [American Society of Clinical Oncology Annual Meeting] plenary session of the ENDURANCE trial [NCT01863550] presented by Shaji Kumar, MD, is a large trial comparing RVd versus KRd. It did answer 1 question between the RVd and KRd, and there was noninferiority [for PFS]. That means RVd is noninferior; however, KRd had more cardiopulmonary and renal toxicity.6 These patients were not high risk. [Translocation] t(4;14) and TP53 were not included. In standard-risk or intermediate-risk patients, RVd stays as a standard of care. I think the paradigm is RVd followed by transplant followed by lenalidomide maintenance remains the standard of care in 2020 for newly diagnosed multiple myeloma.
Can you talk about the CASSIOPEIA trial that led to Dara-VTd being approved?
Let’s talk about quadruplet therapy, VTd plus dara…showing that dara-VTd is superior to VTd alone. This was a large European trial of randomized VTd or dara-VTd, transplant, then consolidation, then a second randomization of observation versus daratumumab maintenance. Clearly, the responses are much higher in the daratumumab arm compared with the non-daratumumab arm [92.6% vs 89.9%]. The stringent complete remission [sCR] rate was 29% versus 20%. The CR rate was 0% with MP, melphalan/prednisone…so we have come a long way.
PFS is far better with dara-VTd compared with VTd [HR, 0.47; 95% CI, 0.33-0.67; P < .0001], but more importantly are the [data] that show, as we keep treating patients from induction to the transplant to end of consolidation to maintenance, our response rate continues to improve. This is exactly what we see also in the GRIFFIN trial. The same thing happens, the CR rate and overall response continue to deepen.
Please review results of the GRIFFIN trial.
GRIFFIN is dara-RVd versus RVd in transplant-eligible patients. The schema is very clear; remember, this is a transplant trial with induction, transplant, consolidation, and maintenance. The maintenance is randomized between dara-Revlimid versus Revlimid alone.
The primary end point [sCR] was met at the end of the consolidation. This is a phase 2 randomized study, not a phase 3. It is not a regulatory study, so the criteria for the significance was not as stringent. It’s a 1-sided, not a 2-sided P value, which was .068 and considered to be .1. With a .060 1-sided P value, the sCR of 42% with the dara-RVd was much more than 32% with the RVd.
The responses deepened over time, both in the dara-RVd and the RVd groups, but the difference in the odds ratio continued to remain sensitive. At the clinical cutoff, we get around 60% of sCR in the dara-RVd arm compared with about 45% [with RVd]. CR or better was 80% in the dara-RVd and 60% in the RVd
We are getting 60% MRD negativity with dara-RVd. Of all evaluable patients, [the rate is] 70% MRD negative compared with 32% with RVd. It’s important to follow the trend…and monitor for sustainability of the MRD negativity at the end of induction, transplant, consolidation, and at the beginning of maintenance, clinical cutoff, and then follow-up. If the MRD negativity is persistent, that clearly shows improvement in the survival.
What are the adverse effects [AEs] associated with the GRIFFIN regimen for the patients with multiple myeloma?
I personally have experience with GRIFFIN. The most common AE was cytopenia. We will do a dose reduction of Revlimid, if we need to, and we also use growth factors. We used levofloxacin, acyclovir, and fluconazole in patients.
Infection was more common with dara-RVd. Infusionrelated reactions were around 40% on the daratumumab arm, but predominantly grade 1 or 2. If you see most of the daratumumab studies, the grade 3/4 infusion reactions are in the single digits of 3% to 4%.
What is your preferred route of daratumumab administration?
Subcutaneous daratumumab [daratumumab and hyaluronidasefihj (Darzalex) Faspro] is now approved, and that’s a good thing for our patients and also for us and our nurses.7 The message [from the trials that led to it being] approved is still the same. The message is subcutaneous daratumumab is noninferior to intravenous [IV] daratumumab. Number 2 is that infusion reactions are less, albeit not 0, with subcutaneous daratumumab. Number 3 is the [onset] of the infusion reaction, at least of the first injection, could be likely delayed compared with IV daratumumab.
For example, I do my subcutaneous daratumumab on a patient at 8 AM. For the first infusion, we would not let the patient go home for several hours to make sure the patient does not get a delayed reaction. Now, if it does not happen in the first injection, the second injection wait time is less…and eventually would be just an in-and-out [appointment].
Which clinical trials show noninferiority of subcutaneous daratumumab when compared with IV daratumumab?
The COLUMBA study [NCT03277105] used subcutaneous daratumumab, which is mixed with hyaluronidase and given quickly, 5 to 6 minutes of injection. The primary end points were overall response [and] our trough concentration.8
The time needed for the infusions [was much less with subcutaneous daratumumab]. However, after that 5-minute infusion, compared with the 7 hours of infusion of the IV, the patient waited. Unfortunately, in our new cancer center, we do not have a separate waiting area for the patients where they can be monitored. Either they are in the same chair or they are sent home. We cannot just ask them to wait in the waiting area where there is no monitoring of the vitals or an RN [registered nurse] looking after the patients.
That means the patients—if any of the subcutaneous injection is completed—are in the chair for several hours even after the first infusion. Don’t think that the patient is in the cancer center for 5 minutes with subcutaneous administration. I don’t think that’s what is real. This is only the infusion time. You are not cutting the time from 7 hours to 5 minutes by subcutaneous daratumumab.
Infusion reactions were milder and occurred primarily at the first administration in both arms. But if you look at the number, daratumumab IV was 34.5% and daratumumab subcutaneous was 12.7%, so it was significant. However, remember grade 3/4 infusion reactions are not very common, those are just in the single digits. Cytopenias, chills, and dyspnea were comparable between the subcutaneous versus IV arms.
References
1. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 4.2020. National Comprehensive Cancer Network. May 8, 2020. Accessed July 30, 2020. https://bit.ly/30Vt1lO
2. FDA approves daratumumab for transplant-eligible multiple myeloma. FDA. September 26, 2019. Accessed July 29, 2020. https://bit.ly/2Ey0vzp
3. Attal M, Lauwers-Cances V, Hulin C, et al. Lenalidomide, Bortezomib, and Dexamethasone with Transplantation for Myeloma. N Engl J Med. 2017;376(14):1311-1320. doi:10.1056/NEJMoa1611750
4. Gay F, Cerrato C, Petrucci MT, et al. Efficacy of carfilzomib lenalidomide dexamethasone (KRd) with or without transplantation in newly diagnosed myeloma according to risk status: Results from the FORTE trial. J Clin Oncol. 2019;37(suppl 15):8002. doi: 10.1200/JCO.2019.37.15_suppl.8002
5. Voorhees PM, Kaufman JL, Laubach JP, et al. Daratumumab, lenalidomide, bortezomib, & dexamethasone for transplant-eligible newly diagnosed multiple myeloma: GRIFFIN [published online April 23, 2020]. Blood. doi:10.1182/blood.2020005288
6. Kumar S, Jacobus SJ, Cohen AD, et al. Carfilzomib, lenalidomide, and dexamethasone (KRd) versus bortezomib, lenalidomide, and dexamethasone (RVd) for initial therapy of newly diagnosed multiple myeloma (NDMM): Results of ENDURANCE (E1A11) phase III trial. J Clin Oncol. 2020;38(suppl 18):LBA3. doi:10.1200/JCO.2020.38.18_suppl.LBA3
7. FDA approves daratumumab and hyaluronidase-fihj for multiple myeloma. FDA. May 1, 2020. Accessed July 30, 2020. https://bit.ly/313sL4w
8. Mateos M-V, Nahi H, Legiec W, et al. Efficacy and safety of the randomized, openlabel, non-inferiority, phase 3 study of subcutaneous (SC) versus intravenous (IV) daratumumab (DARA) administration in patients (pts) with relapsed or refractory multiple myeloma (RRMM): COLUMBA. J Clin Oncol. 2019;37(suppl 15):8005. doi:10.1200/ JCO.2019.37.15_suppl.8005
9. Chari A, San-Miguel J, McCarthy H, et al. Subcutaneous daratumumab plus standard treatment regimens in patients with multiple myeloma across lines of therapy: PLEIADES study update. Blood. 2019;134(suppl 1):3152. doi:10.1182/blood-2019-123560