Barr Evaluates BTK Inhibitors for Treating Frontline CLL
During a virtual Case Based Peer Perspectives event, Paul M. Barr, MD, reviewed the case of a 71-year-old woman with newly diagnosed chronic lymphocytic leukemia and the role of BTK inhibitors in the frontline setting.
Paul M. Barr, MD

During a virtual Case Based Peer Perspectives event, Paul M. Barr, MD, associate professor, Department of Medicine, Hematology/Oncology, medical director Cancer Center, Clinical Trials Office, University of Rochester Medical Center, Rochester, NY, reviewed the case of a 71-year-old woman with newly diagnosed chronic lymphocytic leukemia and the role of BTK inhibitors in the frontline setting.
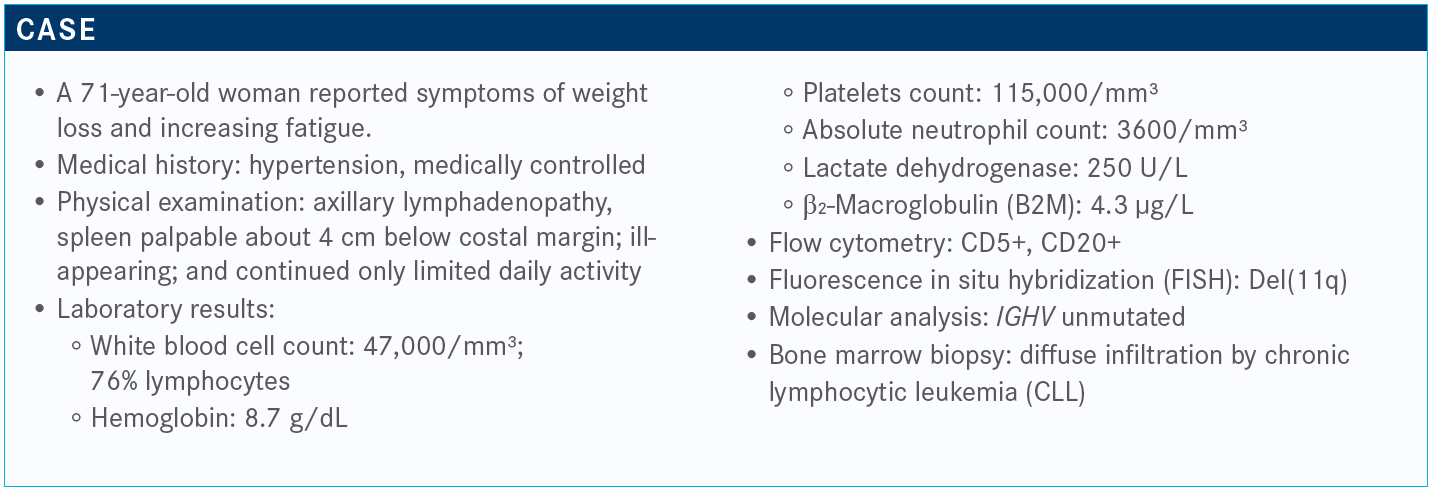
Targeted Oncology™: What do the National Comprehensive Cancer Network (NCCN) guidelines say about collecting prognostic information in a patient such as this?
BARR: The NCCN guidelines,. in terms of testing, mirror the iwCLL [International Workshop on Chronic Lymphocytic Leukemia] guidelines.. Before treatment, most agree that a FISH panel is important to look for deletion 11q [del(11q)] and deletion 17p [del(17p)]. IGHV mutational status is also helpful. Some would say that if you’re going to use a novel agent, it may not be that helpful. Nonetheless, just consider it like a standard board answer. We would normally get IGHV mutational status. The most recent update [indicates] that we should be doing TP53 mutation testing in all patients before treatment because that’s just as bad as a del(17p). It’s becoming easier and easier to perform, but it’s not always universally available. It is something to keep in mind before you start a new treatment.
I think conventional karyotyping, which is encouraged, is not always reliable. Larger mutation panels are technically still considered experimental, but there are more data evolving that [show] they’re going to be helpful over time.
Is there a link between TP53 mutations and del(17p)?
Around 80% of the time, if a patient has a del(17p), they are also going to have the other allele mutation. Most of the time they go hand in hand, but small percentages of the time you can have just 1 allele either deleted or mutated.
The reason to do the mutation testing is to find that relatively small percentage of patients who have a mutation and an arguably poor prognosis when they didn’t have a del(17p).
I think this is representative of what we would see if we had a larger poll around the country. Ibrutinib [Imbruvica] has been around the longest. The nice thing is we have options for our patients.
Right now, in 2020, what’s standard frontline therapy for CLL?
[According to the] NCCN guidelines, ibrutinib [Imbruvica], acalabrutinib [Calquence], and venetoclax [Venclexta] are all preferred regimens for patients who are frail, as well as for patients who are younger, based on recent randomized studies. You can see there are myriad other recommended regimens, but…ibrutinib is the category 1 recommendation.
What data support the use of single-agent ibrutinib in patients with untreated CLL?
The RESONATE-2 study [NCT01722487] was a randomized clinical trial, now with more than 5 years of follow-up, and this led to the approval of ibrutinib in the first-line setting.. It compared ibrutinib with chlorambucil…in patients older than 65 years who were not candidates for aggressive chemoimmunotherapy. It did not include any patients with del(17p) in this study.
It’s not a surprise to anyone that the PFS [progression-free survival] is better with ibrutinib than chlorambucil [HR, 0.146].⁴ We know that ibrutinib can sustain remissions for a long time, but there is a continuous rate of relapse. At 5 years, about 70% of patients are still without progression [versus 12% with chlorambucil].
How do patients with poor prognostic features do with ibrutinib therapy?
With chemoimmunotherapy, patients with IGHV-mutated disease always responded better. But with ibrutinib, they seem to overcome the poor prognostic potential of IGHV status. When you look at [the Kaplan-Meier curves for PFS], the unmutated population seems to respond just as well as mutated, which is encouraging.
We’ve seen across 3 randomized studies that patients with del(11q) who are on ibrutinib seem to perform better than those without del(11q). The BTK [Bruton tyrosine kinase] inhibitors seem to be performing well in those patients for reasons we don’t quite understand. But we’ve seen this again, the same phenomenon in 3 randomized studies. Hopefully that makes sense, but the major take home is that for these 2 poor prognostic markers, ibrutinib seems to overcome them.
What other clinical trials examine ibrutinib against chemotherapy?
The E1912 study [NCT02048813] compared ibrutinib, in this case plus rituximab [Rituxan], against FCR [fludarabine, cyclophosphamide, and rituximab]. FCR was given for 6 cycles. Ibrutinib was given until disease progression or is being given until disease progression [in those still responding]. During the study design phase, we decided to include 6 cycles of rituximab in the early days, and this was for younger patients. These are patients who have limited comorbidities, are younger than 70 years, and are in overall good condition. The primary end point was PFS.⁵
To me, this was one of the most fascinating studies to see the results play out. Ibrutinib provided a better PFS than FCR [HR, 0.39; 95% CI, 0.26-0.57; P < .0001], and the benefit was mostly realized in IGHV-unmutated patients [HR, 0.28; 95% CI, 0.17-0.48; P < .0001].
What really shocked me was the survival benefit in the study. The patients who received ibrutinib and rituximab had better overall survival [OS] compared with FCR [HR, 0.34; 95% CI, 0.15- 0.79; P = .009]. This is why the NCCN guidelines have replaced chemoimmunotherapy with the novel agents. Some would argue that a low-risk patient still might be served well with FCR. If you have a young patient who has a positive IGHV mutation, it’s still reasonable to have a conversation given the excellent long-term outcomes with FCR, but I rarely see those patients. Most of the patients who need treatment have risk factors. They have IGHV unmutated, they have del(11q), or some other risk factor.
Because of that study, ibrutinib and rituximab was approved.⁶ In young patients, that’s what I’m going to use.
Which regimen would you prefer for an older patient?
This ALLIANCE study [NCT01886872] looked at patients who are older. Some have said that based on this study, rituximab doesn’t add a whole lot to ibrutinib. This was a randomized, phase 3 trial comparing 3 arms in patients older than 65 years, but the patients had to have an adequate creatinine clearance and adequate liver function. They compared ibrutinib versus ibrutinib and rituximab versus BR [bendamustine and rituximab], which was given for 6 cycles. Both of the ibrutinib arms continue ibrutinib until progressive disease.⁷
Both ibrutinib arms have shown superiority in terms of PFS over BR. This was presented a couple years ago and is not new. Again, the 2 ibrutinib curves for PFS are overlapping, suggesting no real benefit to rituximab in this older population. There was no overall survival benefit in this study, and there’s a lot of speculation why that may be. There are competing causes of death in older patients.
In terms of AEs [adverse effects], there were more hematologic toxicities, more cytopenias, with BR. But there were more nonhematologic toxicities with the ibrutinib arms, such as A-fib [atrial fibrillation], hypertension, low-grade bleeding.
What other BTK inhibitors would you consider?
Acalabrutinib [from] the ELEVATE TN study [NCT02475681] in treatment-naive patients was designed in a similar manner [to ALLIANCE], but the results are a bit different.⁸
Acalabrutinib was developed to be a more specific BTK inhibitor and to have less off-target effects. It is potent and binds the enzyme. They chose a twice-a-day dosing schedule to achieve maximal occupancy of BTK. It is focused on the BTK enzyme with much fewer off-target effects, attempting to provide a more specific efficacious drug with [fewer adverse] effects.
This study in treatment-na.ve patients enrolled those older than 65 years, similar to the ALLIANCE study and to RESONATE 2. They did include del(17p). There were 3 arms, acalabrutinib and obinutuzumab [Gazyva], acalabrutinib alone, or obinutuzumab plus chlorambucil.
From what we’ve seen before, it’s not a shocker that…the 2 acalabrutinib PFS curves handily beat the obinutuzumab and chlorambucil curve. Patients start to relapse pretty quickly [with obinutuzumab plus chlorambucil]. The study wasn’t designed to compare acalabrutinib versus acalabrutinib and obinutuzumab; but if you analyze it statistically, somewhat post hoc, there is a statistical difference. It does look as though, with only about 2 years of follow-up, adding obinutuzumab provides a better PFS.
Now, it’s not clear if it’s because of the BTK inhibitor or it’s because of the CD20 antibody. Is acalabrutinib a better partner or is obinutuzumab a better CD20? No one’s going to be able to answer that question with this study, but it does make you want to watch this over time and potentially consider obinutuzumab for some patients when you’re using acalabrutinib.
The other point to make is when you add the CD20 antibody, you get deeper responses. There’s a higher CR [complete response] rate, 23% for patients who got acalabrutinib and obinutuzumab versus 1% with acalabrutinib monotherapy.
I’m interested in thinking about what the differences are between the acalabrutinib AEs and what we see with ibrutinib. There’s about a 4% rate of A-fib [with acalabrutinib alone]. We’re not randomizing against ibrutinib here, but if you compare against the ibrutinib studies, it does seem as though there’s a lower rate of A-fib. You could say the same about any-grade hypertension, which is about 4% to 7%. That does seem lower [than with ibrutinib], albeit with only 2 years of follow-up. The bleeding rates are similar at roughly 40%, but the major bleeding remained low. Significant bleeding is in the 1% to 2% range.
Are there data supporting the use of a BCL2 inhibitor in this patient population?
The CLL14 trial [NCT02242942] was updated this year in 432 patients, conducted through the German CLL group. This study compared chlorambucil and obinutuzumab with venetoclax and obinutuzumab. The major diff erence here is this is a defi ned treatment course. This is 1 year of therapy. The BTK inhibitors are largely given until disease progression. This is 1 year of chlorambucil and 6 cycles of obinutuzumab compared with 6 cycles of obinutuzumab and 1 year of venetoclax.⁹
The study enrolled patients with a higher CIRS [Cumulative Illness Rating Scale] scores and impaired creatinine clearance, but there was no age cutoff. [Because they tried] to enroll patients with comorbidities, the median age was around 72 years….Most of the patients had a CIRS score of greater than 6.
The PFS curves, not surprisingly, favor venetoclax/obinutuzumab versus chlorambucil plus obinutuzumab [HR, 0.33; 95% CI, 0.22-0.51; P < .001]. As we’ve seen before, right at the 12-month mark, the chlorambucil and obinutuzumab PFS curve starts falling off. As soon as those patients finish treatment, the progressions start. It looks similar to an ibrutinib curve that we saw at 2 years. This is what led to the approval of venetoclax and obinutuzumab in the first-line setting.10
One of the most interesting points about venetoclax is we’re getting deeper remissions when MRD [minimal residual disease] negativity [is achieved]. It’s not standard of care to test MRD just yet in all of our patients, but it will be in the future. We saw with FCR MRD-negative rates of about 30% to 50%. In this study, with 1 year of the venetoclax combination, 76% were MRD negative. In the bone marrow, 57% were MRD negative, which suggests that this is a platform to build on and can serve patients well.
Do you agree with this treatment decision? Would you add rituximab to ibrutinib for this patient?
That’s a reasonable strategy. The counterpoint, some would say, is that in older patients, rituximab didn’t add much. I think we have ground to stand on with either strategy.