Gasparetto Addresses Triplet Versus Doublet Induction Options in Multiple Myeloma
During a virtual Case Based Peer Perspective event, Cristina Gasparetto, MD, discussed the case of a geriatric male diagnosed with stage II multiple myeloma.
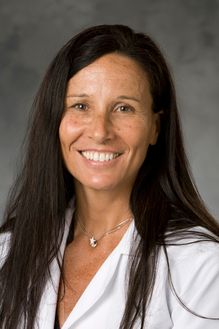
During a virtual Case Based Peer Perspective event, Cristina Gasparetto, MD, professor of Medicine, Director, Multiple Myeloma Program, Duke University School of Medicine Durham, NC, discussed the case of a geriatric male diagnosed with stage II multiple myeloma.
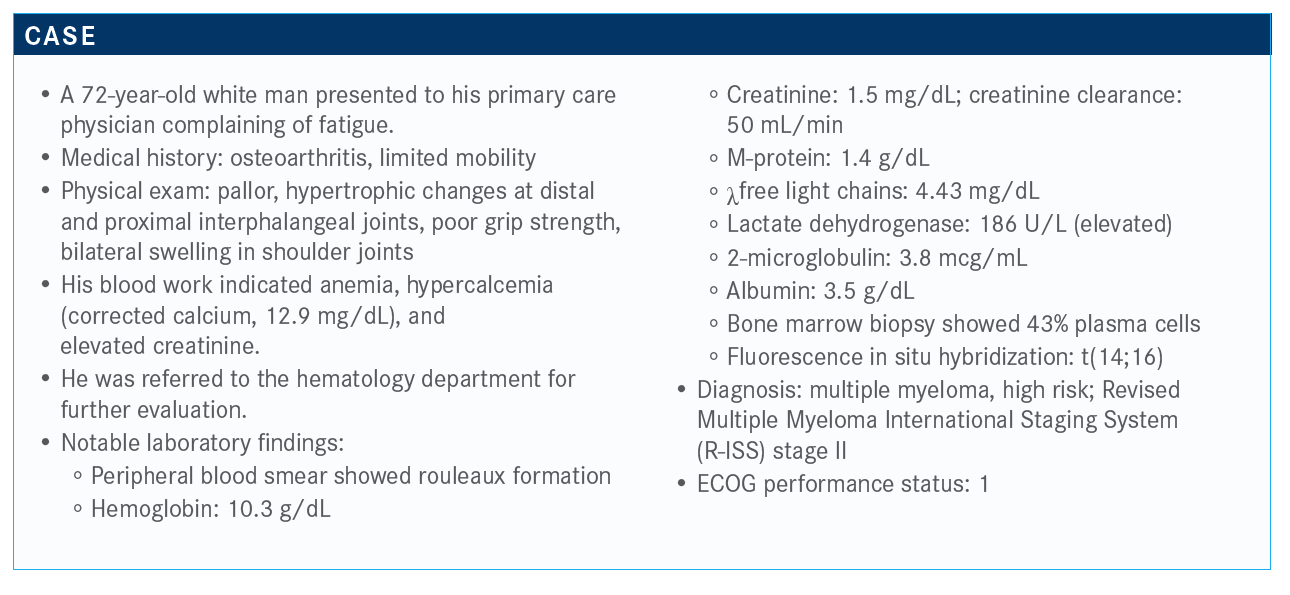
Targeted OncologyTM: Would you say that this patient is eligible for transplant? Why or why not?
GASPARETTO: He’s 72 [years old], and the problem with this patient is he does not have a lot of comorbidities, except osteoarthritis and low mobility. So can he survive transplant?
I think that at 72, some patients are in great shape. The outcome of transplant for this population of patients is comparable to the younger population. But, when you are dealing with patients [who are] frailer and more unfit, that is a different situation. It looks like this patient [might be considered] unfit, so can we bring him to the next level with induction and transplant or forget about the transplant.
The geriatric assessment is going to be important because patients, if they’re fit, have to receive optimal treatment [as with] younger patients; for the unfit and the frail, we have to do our best to deliver therapy. If you look at [the] overall survival [OS] of older patients, it’s inferior, but I don’t think there is anything different in the biology of the disease. It has more to do with the fact that we are unable to deliver enough therapy to these patients.
Do you have an age limit for transplant eligibility? I know at Duke we don’t, but I tend to stop around 76 years. But there are some exceptions; good performance status is important, [as is] adequate organ function and absence of lots of amyloidosis. Of course, transplant for amyloidosis is well established, but if you have a patient with cardiac involvement, you definitely need to be a little bit more cautious when you make the decision to transplant.
There is a study that was presented [recently of] daratumumab [Darzalex] and CyBorD [cyclophosphamide, bortezomib (Velcade), dexamethasone] versus CyBorD in amyloidosis showing tremendous results with additional data for this disease [NCT03201965].1 The daratumumab/CyBorD [regimen] clearly performed better.
You need to see the patient and decide if they are able to sustain therapy. And if the patient is [able], I don’t have any objection to treating the patient aggressively. But some of these patients, unfortunately, are incapable. You can have a 50-year-old in a wheelchair with oxygen with TPN [total parenteral nutrition]. I’m sorry, but I couldn’t proceed to transplant even if [this patient] was 50. Of course, it’s all [about] the comorbidities and other medical issues.
What is your impression of these options?
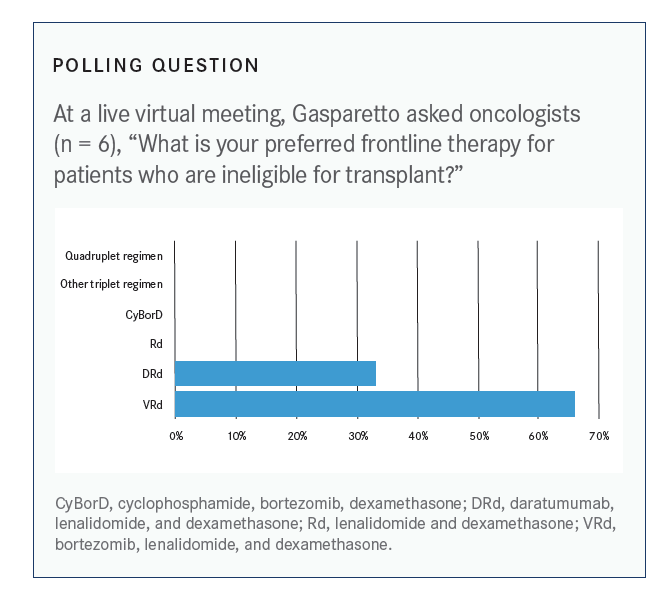
The MAIA trial [NCT02252172, made] a big splash when it was presented as a plenary session at the 2018 American Society of Hematology Annual Meeting showing [effi cacy and] lots of patients achieving deep responses [with the DRd regimen (daratumumab, lenalidomide [Revlimid], and dexamethasone) with a complete response rate of 47.6%], including minimal residual disease [MRD].2 I think we do have more and more data showing that the triplets are important. But are our patients who are nontransplant eligible able to sustain VRd [bortezomib, lenalidomide, and dexamethasone] for a prolonged period of time? Do we aim for MRD for this population of patients?
Should treatment be considered here instead of transplant?
This is a discussion [to have with the patient]. I generally do not close the door to transplant with many patients. But with the data that we have with the addition of daratumumab particularly, we’re performing well. I think we really need to have a conversation with these patients [about] the pros and the cons.
If you gave the patient VRd, would he require a dose reduction of lenalidomide?
Absolutely. I think that in the elderly, we need to make a proper dose adjustment because of the creatinine clearance. I don’t think the patients older than 70 years are capable of tolerating the bortezomib twice a week. I always go to weekly [administration] because of the toxicity.
There was an interesting paper…several years ago talking about dose modification in [older patients]. And even when we do maintenance, we have to make the proper adjustment to the dexamethasone dose also. That’s the reason why sometimes patients do not perform well, because we’re trying to minimize the toxicities and deliver fewer drugs; therefore, finding the best combination is key.
What are the other frontline treatment options for such patients who may not be eligible for transplant?
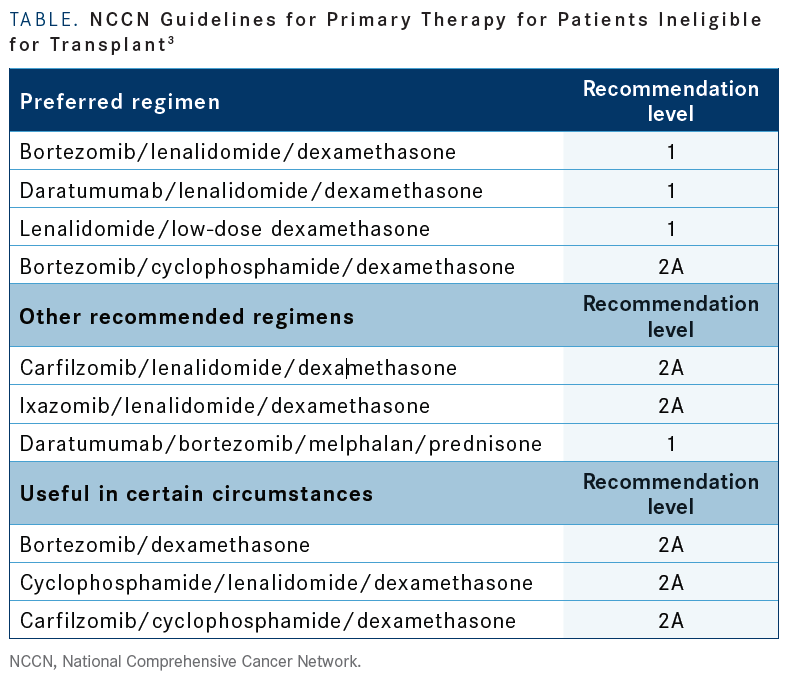
These are the NCCN [National Comprehensive Cancer Network] Guidelines [TABLE].3 Remember, there was a press release stating that the ixazomib [Ninlaro]/lenalidomide/dexamethasone regimen for transplant-ineligible [patients with newly diagnosed multiple myeloma] did not meet the progression-free survival [PFS] primary end point [in the TOURMALINE MM2 phase 3 trial (NCT01850524)], which was a comparison with lenalidomide/ dexamethasone [35.3 vs 21.8 months; HR, 0.83; P = .073].4
There are different combinations. [In terms of] category 1 [recommendations, there are] the bortezomib/lenalidomide/ dexamethasone regimen [and] the daratumumab regimen from the MAIA study, of course, as well as the lenalidomide/dexamethasone combination.
aThe category 1 recommendation is based upon high-level evidence; there is a uniform NCCN consensus that the intervention is appropriate. Category 2A is based upon lower-level evidence; there is a uniform NCCN consensus that the intervention is appropriate.
Which factors do you consider when choosing an induction therapy regimen for a patient such as this one?
I think that when you consider initial treatment for your patient, [you must] always remember the initial treatment is important because you are able to achieve a deeper response and durability. The duration of response may last for several years. You want to lay all your cards up front because when the patient relapses, it’s a done deal. If you look at the OS of patients [who are] refractory, progressing on daratumumab, you are talking about 6 months or less. Here you have to take into consideration the fact that you want to treat your patient aggressively, but you are dealing with older patients. You want [to consider]: the convenience; the logistics; the infusion time; cost to patients; genetics of the myeloma; the commute; other patient comorbidities, particularly renal dysfunction and cardiovascular; the performance status; and safety and toxicity. Sometimes, the decision is even more complicated because you want to reach a goal, you want to maintain quality of life and you know that your patient has to be able to stay on therapy for a prolonged period of time.
What would your choice be for an induction regimen for a patient such as this and what is the data for it? For many years and still now, I [have thought that] the lenalidomide/ dexamethasone is still a good induction [regimen] for frail patients. However…a triplet is definitely the way to go strong out of the gate. The SWOG S0777 trial [NCT00644228], presented by Brian Durie, MD, compared VRd with Rd. If you look at the median age of these patients, it was a little bit younger than I expected. Only 43% were above 65 years, so there were more than 50% of younger patients. [There was an] intent to transplant in 68%. The primary end point was PFS. OS, overall response, and safety were secondary.5
It was clear that the primary end point was met with the triplet, 41 months versus 29 months with the doublet [HR, 0.742; 96% CI, 0.594-0.928; P = .003]. But again, remember, if you have an 88-year-old patient who is frail, he probably is not going to be able to tolerate your triplet and you may be content with your doublet. But it’s clear that 3 drugs are better than 2.6
The [median] OS [had] not yet been reached with a median follow-up of 84 months for the VRd arm versus 69 months for the Rd arm [HR, 0.709; 96% CI, 0.543-0.926; P = .0114].
[In terms of] the adverse events [with VRd versus Rd, there’s more] pain. It’s a little bit harder on quality [of life]. You have more [grade 3 or greater] neurological toxicity with peripheral neuropathy, up to 33%; some grade 3 pain [12%]; and sensory events [23%]. There is gastrointestinal toxicity [22%] and the peripheral neuropathy. You are attacking the myeloma more aggressively but losing a bit on quality of life.5
Is there any way to manage those toxicities for a patient at higher risk? We can modify the regimen to have better tolerability by giving the bortezomib weekly, adjusting the lenalidomide, and adjusting the dexamethasone. A modified VRd [regimen] with weekly Velcade still showed an overall response rate of 87%; 88% in the induction and 75% in the salvage setting. Still, the peripheral neuropathy [rate] of 11.6% is less than what we see with the biweekly administration and [fewer] dose reductions. If you have an older patient, probably going out of the gate with the biweekly [administration of bortezomib] is not recommended. And we have data to support the weekly [bortezomib] in this situation.7
What other treatment options are available in this setting? The MAIA study is an important study [that asked]: Can we improve the backbone of lenalidomide/dexamethasone by using a different drug? [There was] less peripheral and neurological toxicity with the more tolerable daratumumab. This study was [presented in a] plenary session showing the daratumumab/lenalidomide/dexamethasone combination in newly diagnosed, nontransplant-eligible patients, more than 700, [was superior in terms of PFS]. There was stratification based on the age [of] 75 years.2
Ninety-nine percent of patients were over 65, so we are talking about the nontransplant-eligible patients. The PFS was 71 months compared with 56 for the Rd arm. We have the median OS that was not yet reached in both arms [HR, 0.78; 95% CI, 0.56-1.1], and we have [the] overall response [rate that] was a little bit better with the daratumumab, 93% versus 81% [P < .0001]. The stringent complete response rate [was 30% with daratumumab/Rd versus 12% with Rd alone] and the MRD-negativity rate was 24% for the daratumumab/Rd versus 7% with the doublet [P < .0001]. Because of that, this regimen was approved in this setting and I think it’s one of the most important regimens in this setting.8
But the patients that didn’t do as well were the patients with high-risk disease. My recommendation is if you have a standardrisk, transplant-ineligible patient, this could be a good regimen. But, if you have a patient with high-risk cytogenetics, like the case presentation with a (14;16) translocation, you want to keep the proteasome inhibitor in your algorithm. Daratumumab/Rd [is appropriate] for the standard-risk myeloma.
If you look at the patients on the doublet who were able to achieve the MRD negativity, they did not do as well, but it was only 7%. The MRD is again coming back as a goal of therapy and primary end point when you initiate induction for [patients with] newly diagnosed [illness].
With the addition of daratumumab to our combination, we see more myelosuppression, so be very careful in this population of patients. Particularly, there’s more grade 3/4 neutropenia. Therefore, there’s a higher risk of pneumonia and other upper respiratory infection.
The rate of deep vein thrombosis or pulmonary embolism was about the same at [12% with daratumumab versus 13% without], so patients should receive proper anticoagulation with aspirin or other [agents] if they’re allergic or intolerant. The number of second primary malignanc[ies] was about the same in both arms.
What are your thoughts on the case at this point?
He was treated with the doublet. The lenalidomide was adjusted based on the creatinine clearance, and that’s important because, if not, it accumulates and is going to cause a lot of myelosuppression.
How long would you leave your patient on this regimen?
Particularly with the (14;16) translocation, I think that the exposure to a proteasome inhibitor would be important. I would… switch to a maintenance therapy and continue until the time of progression.
Would you ever consider a doublet of bortezomib/dexamethasone?
If we see the patient is intolerant to lenalidomide, you could, in an older patient, choose a doublet with bortezomib, particularly based on the cytogenetics. If you have t(4;14) or t(14;16), I think it’s more important than the IMiD [immunomodulatory drug]. But because they’re high risk, I generally like to use the triplet anyway. But…some patients can’t tolerate IMiDs, and there are some of these patients, definitely. And remember, you also have your CyBorD. My patient today on dialysis had a difficult time with the lenalidomide, even after we adjusted to 5 mg per day. She was switched to Vd, but the CyBorD data are also important in this population of patients. The daratumumab/Velcade/dexamethasone regimen will be important, too. Now we have the CASTOR study [NCT02136134] in first relapse showing phenomenal results, too, particularly in patients with renal insufficiency.
What is your approach to maintenance therapy?
The data on continuation of maintenance are accumulating. There [were results] presented at ASCO [American Society of Clinical Oncology Virtual Scientifi c Program] of the StaMINA study [NCT01109004] with longer follow-up, showing [that] the patients who were able to continue maintenance until progression with an average of 3.6 years did the best with a longer PFS [P = .0004] and [similar] OS.9 One of the messages of ASCO is never stop maintenance, but the risk of secondary malignancy is a concern.
REFERENCES
1. Palladini G, Kastritis E, Maurer MS, et al. Daratumumab plus CyBorD for patients with newly diagnosed AL amyloidosis: safety run-in results of ANDROMEDA. Blood. 2020;136(1):71-80. doi:10.1182/blood.2019004460
2. Facon T, Kumar SK, Plesner T, et al. Phase 3 randomized study of daratumumab plus lenalidomide and dexamethasone (D-Rd) versus lenalidomide and dexamethasone (Rd) in patients with newly diagnosed multiple myeloma (NDMM) ineligible for transplant (MAIA). Blood. 2018;132(suppl 1):LBA-2. doi:10.1182/blood-2018-120737
3. NCCN. Clinical Practice Guidelines in Oncology. Multiple myeloma, version 4.2020. Accessed August 5, 2020. https://bit.ly/3gwpLUO
4. Takeda provides update on TOURMALINE-MM2 phase 3 trial. News release. Takeda; March 10, 2020. Accessed August 5, 2020. https://bit.ly/3gIC14N
5. Durie BGM, Hoering A, Abidi MH, et al. Bortezomib with lenalidomide and dexamethasone versus lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma without intent for immediate autologous stem-cell transplant (SWOGS0777): a randomised, open-label, phase 3 trial. Lancet. 2017;389(10068):519-527. doi:10.1016/S0140-6736(16)31594-X
6. Durie BGM, Hoering A, Sexton R, et al. Longer term follow-up of the randomized phase III trial SWOG S0777: bortezomib, lenalidomide and dexamethasone vs. lenalidomide and dexamethasone in patients (Pts) with previously untreated multiple myeloma without an intent for immediate autologous stem cell transplant (ASCT). Blood Cancer J. 2020;10(5):53. doi:10.1038/s41408-020-0311-8
7. Rodriguez C, Lantz J, Akbar F, Lantz L, Dressler E. Assessing effi cacy and tolerability of a modifi ed lenalidomide/bortezomib/dexamethasone (VRd-28) regimen using weekly bortezomib in multiple myeloma. Clin Lymphoma Myeloma Leuk. 2019;19(10) (suppl):E217-E218. doi:10.1016/j.clml.2019.09.362
8. Facon T, Kumar S, Plesner T, et al; MAIA Trial Investigators. Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med. 2019;380(22):2104-2115. doi:10.1056/NEJMoa1817249
9. Hari P, Pasquini MC, Stadtmauer EA, et al. Long-term follow-up of BMT CTN 0702 (STaMINA) of postautologous hematopoietic cell transplantation (autoHCT) strategies in the upfront treatment of multiple myeloma (MM). J Clin Oncol. 2020;38(suppl 15):8506. doi:10.1200/JCO.2020.38.15_suppl.8506