Kim Assesses Multiple Regimens That Demonstrated Efficacy in NSCLC Trials
In a Targeted Oncology Case-Based Roundtable event Edward S. Kim, MD, MBA, discussed new regimens for the treatment of non-small cell lung cancer.
Edward S. Kim, MD, MBA

In a Targeted Oncology Case-Based Roundtable event Edward S. Kim, MD, MBA, the physician-in-chief at City of Hope and vice physician-in-chief at City of Hope National Medical Center, discusses new regimens for the treatment of non-small cell lung cancer.
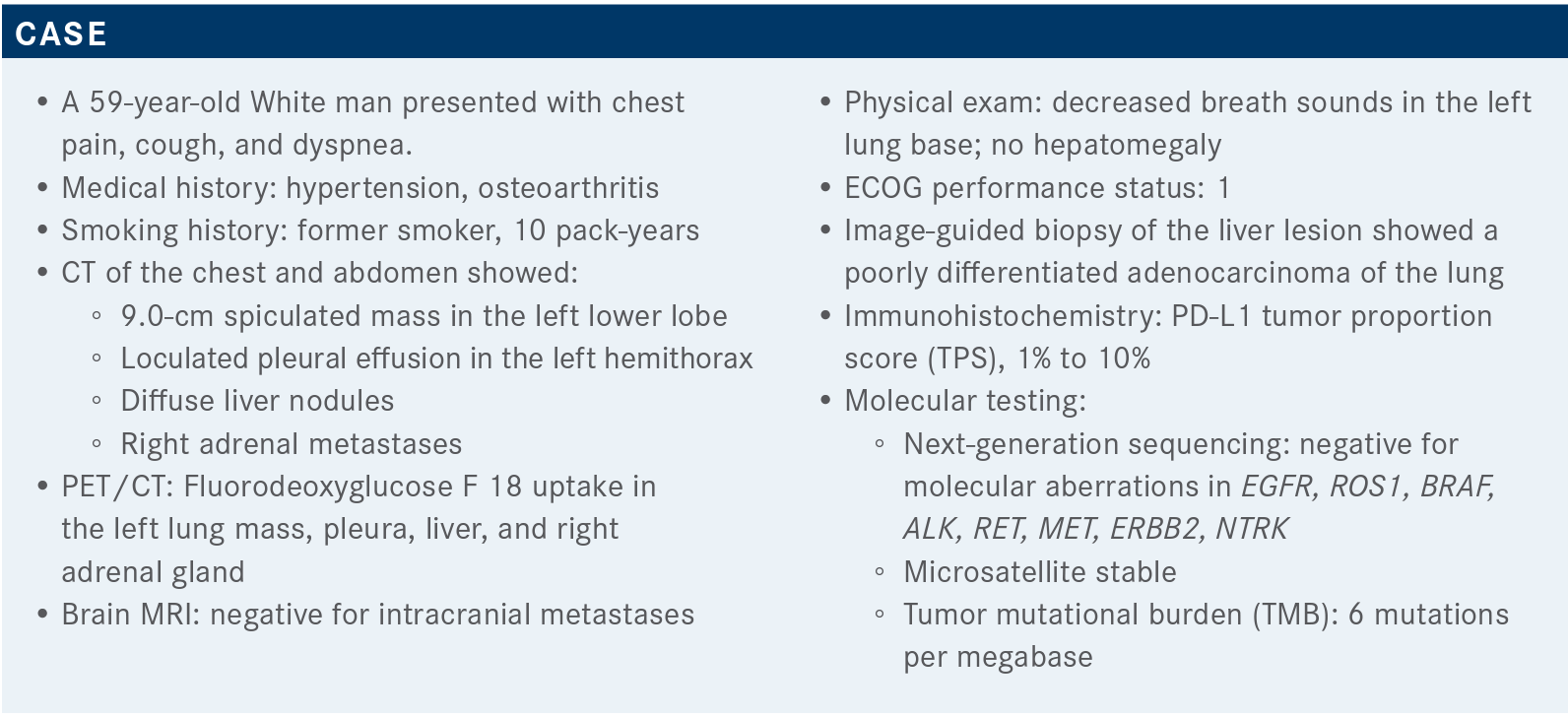
Targeted OncologyTM: What type of molecular testing would you obtain in a patient with nonsquamous non–small cell lung cancer (NSCLC)?
KIM: According to the current National Comprehensive Care Network [NCCN] guidelines [for frontline molecular testing of NSCLC], both liquid and tissue-based, testing absolutely needs to include KRAS, EGFR, ALK, ROS1, BRAF, NTRK1/2/3 fusions, METex 14 skipping variants, and RET; PD-L1 is also something that we try to get up front.1 The [preference] is always to try to get the tissue, to make sure we have a histologic diagnosis, which is something that the blood cannot always give you.
What does the NCCN recommend for patients like this with no driver mutations?
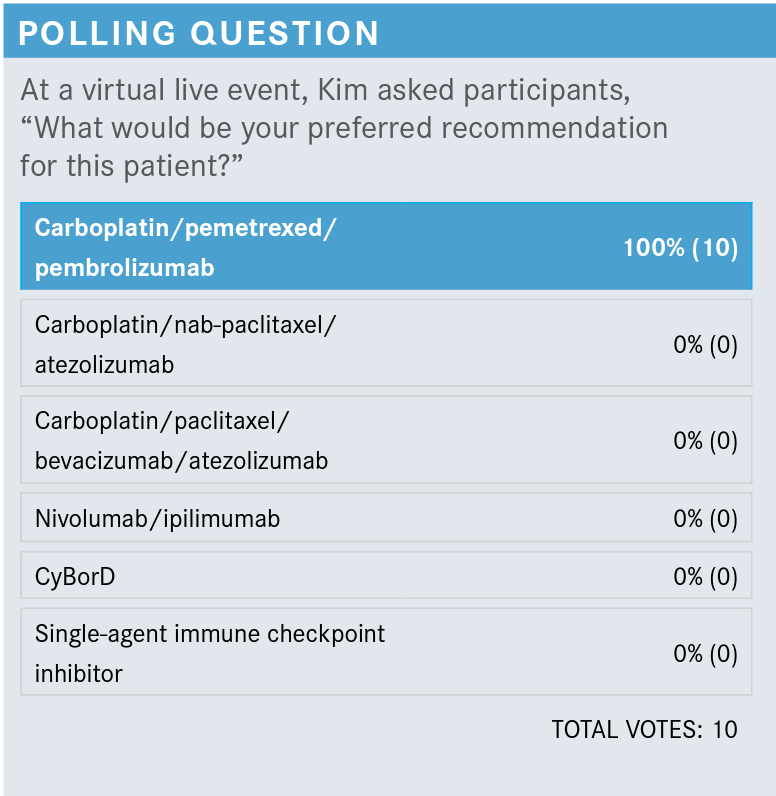
NCCN says that the preferred [category 1] regimen for first line in patients who don’t have these driver mutations and who have PD-L1 expression that ranges from 1% to 49% is a platinum agent [carboplatin or cisplatin] plus pemetrexed [Alimta] and pembrolizumab [Keytruda]. There are other recommended regimens that are also category 1: the regimen of carboplatin, atezolizumab [Tencentriq], bevacizumab [Avastin], and paclitaxel; and nivolumab [Opdivo], ipilimumab [Yervoy], pemetrexed, and a platinum agent. You also have the carboplatin, nab-paclitaxel [Abraxane], and atezolizumab regimen, and included [as “useful in certain circumstances”], the nivolumab plus ipilimumab regimen [category 1], and pembrolizumab [category 2B]. So, there are quite a few options for these adenocarcinomas not otherwise specified.
What is the evidence supporting the use of pembrolizumab with chemotherapy?
KEYNOTE-189 [NCT02578680] was a nice study of chemotherapy—pemetrexed and either carboplatin or cisplatin—plus or minus pembrolizumab. This was for untreated, advanced, metastatic, non-squamous NSCLC, with no driver mutations in EGFR or ALK. It did not require PD-L1 status, though it did [require the collection of] a sample for PD-L1 assessment.2
At the [approximately] 23-month median follow-up, the pembrolizumab combination with chemotherapy was superior from an overall survival [OS] standpoint. At 12 months, the OS rate for the pembrolizumab combination versus placebo was 70.0% versus 48.1%, respectively. At 24 months, the respective rates were 45.5% versus 29.9%. Who knew we were going to get almost 50% survival at 24 months? That’s pretty darn good. Median OS was 22 months [95% CI, 19.5-25.2] versus 10.7 months [95% CI, 8.7-13.6], [HR, 0.56; 95% CI, 0.45-0.70]. Very good, impressive data, and [this] has become the standard of care.3
How did PD-L1 expression influence efficacy?
Regarding PD-L1 expression, there was a real OS benefit for groups with PD-L1 expression that ranged from a TPS of less than 1%, all the way up to greater than 50%. It wasn’t just the [patients with high PD-L1 expression] who had a benefit, so that was reassuring. Among patients whose TPS was less than 1%, median OS was 17.2 months [95% CI, 13.8-22.8] in the pembrolizumab group versus 10.2 months [95% CI, 7.0-13.5] in the placebo group. When TPS ranged from 1% to 49%, median OS was 21.8 months [95% CI, 17.7-25.9] versus 12.1 months [95% CI, 8.7-19.4]. Finally, when TPS exceeded 50%, median OS was not reached [NR] in the pembrolizumab group [95% CI, 20.4-NR] and 10.1 months in the placebo group [95% CI, 7.5-NR].3
What are the data that support other regimens, and for which patient populations?
There is now a whole host of regimens that have joined the KEYNOTE-189 regimen. That doesn’t mean you’re using all of these, clearly, but they were placed on the NCCN guidelines.
[One such regimen is from] KEYNOTE-042 [NCT02220894], looking at metastatic, untreated NSCLC with a TPS of greater than or equal to 1% with no alternation in EGFR or ALK. This was a 1:1 randomization of pembrolizumab at 200 mg, as a single agent, every 3 weeks, versus carboplatin plus paclitaxel or carboplatin plus pemetrexed. This study looked at OS in groups with a TPS of greater than or equal to 50%, 20%, and 1% [to evaluate] the effect of PD-L1.4
When TPS was greater than or equal to 50%, there was a median OS of 20 months [95% CI, 15.4-24.9] versus 12.2 months [95% CI, 10.4-14.2] [HR, 0.69; 95% CI, 0.56-0.85; P = .0003]. When TPS was greater than or equal to 20%, OS was 17.7 months [95% CI, 15.3-22.1] versus 13.0 months [95% CI, 11.6-15.3] [HR, 0.77; 95% CI, 0.64-0.92; P = .0020] and when TPS was greater than or equal to 1%, the OS was 16.7 months [95% CI, 13.9-19.7] versus 12.1 months [95% CI, 11.3-13.3] [HR, 0.81; 95% CI, 0.71-0.93; P = .0018]. In the curves, there’s an early period where the curves cross [and the chemotherapy group shows better OS], but as you get past that 6-month period, [the data] seem to be very much in favor of the single-agent pembrolizumab.5
How did PD-L1 levels correlate with benefit in this study?
When they looked at patients with TPS scores of 1% to 49%, OS was much more similar [between the treatment groups]. Again, the [data showed early benefit in the chemotherapy group, and later benefit in the pembrolizumab group]. Median OS was 13.4 months [95% CI, 10.7-18.2] in the pembrolizumab group versus 12.1 months [95% CI, 11.0-14.0] in the chemotherapy group.4 This was a slight benefit, but certainly not [of] the magnitude that we saw with some of the other cutoffs; it seemed like the higher [PD-L1 levels] were driving the benefit.
What data support the use of atezolizumab and bevacizumab?
The IMpower150 study [NCT02366143] was a unique study, in that it was the only one that had previously allowed patients with sensitizing mutations for EGFR or ALK. It was in chemotherapy-naïve patients with non-squamous NSCLC; patients were tested for PD-L1 status [via immunohistochemical analysis].6,7
This was a 3-arm study. Arm A was atezolizumab with carboplatin and paclitaxel, followed by the atezolizumab maintenance. Arm B was atezolizumab, carboplatin, paclitaxel, and bevacizumab, followed by maintenance with atezolizumab plus bevacizumab. Arm C was carboplatin, paclitaxel, and bevacizumab, followed by bevacizumab maintenance. All these patients were treated with maintenance until the patient had either progression or adverse events [AEs].7
Arm C was the comparator, so Arm A and Arm B were [each] compared with Arm C separately. What they showed was, when you compared Arm B to Arm C, there was benefit in adding the atezolizumab on top of the triplet regimen. The stratified hazard ratio [HR] was 0.78 [95% CI, 0.64-0.96; P = .02].7
There was some crossover [of the curves], but the median OS between these 2 groups was 19.2 months [95% CI, 17.0-23.8] versus 14.7 months [95% CI, 13.3-16.9], so there was something meaningful with the 4-drug regimen.7
Can you talk about data in support of nivolumab and ipilimumab?
The CheckMate 227 trial [NCT02477826] had a patient population with stage IV or recurrent NSCLC; no gene alterations in the tissue were allowed, and both squamous and non-squamous [cancer was included]. Patients were stratified according to PD-L1 expression [greater than or equal to 1% versus less than 1%. These regimens entailed nivolumab and ipilimumab, chemotherapy, or single-agent nivolumab for patients with a PD-L1 level greater than or equal to 1%. Among those with PD-L1 levels less than 1%, the regimens were nivolumab and ipilimumab, chemotherapy, or nivolumab plus chemotherapy.8,9
When they [compared the] nivolumab plus ipilimumab combination with chemotherapy, among patients with a PD-L1 level of greater than or equal to 1%, the HR for OS at the 3-year update was 0.79 [95% CI, 0.67-0.93]. Again, [the curves do] cross at 6 months [at which point the benefit switches from chemotherapy to the nivolumab plus ipilimumab combination].10
When you look at patients with 1% to 49% [PD-L1 expression], there was no difference in median OS [HR, 0.94; 95%CI, 0.75-1.18], as opposed to [other PD-L1 subgroups]. The biggest benefit was among patients with PD-L1 greater than or equal to 50%; median OS was 21.2 months versus 14.0 months [HR, 0.70; 95% CI, 0.55-0.90]. Those middle scores of PD-L1 [didn’t see much benefit].9
Were there concerning AEs with the nivolumab plus ipilimumab combination?
We are always cognizant of AEs. This is what happens when you start going to 4 drugs, or, [as in this case], nivolumab and ipilimumab together. You expect to get some additional AEs when you have nivolumab [plus] ipilimumab. With the dosages that have been utilized, it’s much better tolerated, so it’s a little easier to give. When you look at the grade 3 and grade 4 toxicities, some were worse with nivolumab and ipilimumab, some were worse with chemotherapy. There were more treatment-related AEs [of any grade] leading to discontinuation with the nivolumab and ipilimumab [18.1%] than with chemotherapy [9.1%], and treatment-related AEs of grade 3 or 4 [that led to discontinuation] were 12.3% versus 4.9%, respectively, so those are things that we keep in mind.9
What other data shed light on nivolumab plus ipilimumab?
CheckMate 9LA [NCT03215706] was a study of advanced or recurrent NSCLC with no prior systemic therapy, no genomic alterations, and a good ECOG performance status, stratified by PD-L1 [expression] less than 1% versus greater than or equal to 1% and histology [squamous versus non-squamous]. [The treatment arm was] nivolumab, ipilimumab, and chemotherapy—2 cycles of chemotherapy, not concurrent; the control arm was chemotherapy for 4 cycles, and pemetrexed maintenance could be given to non-squamous patients. OS was the primary end point.11,12
There was a benefit in OS [for patients who received nivolumab and ipilimumab with chemotherapy, versus chemotherapy alone (HR, 0.66; 95% CI, 0.55-0.80)].12 Median OS was 15.6 months [95% CI, 13.9-20.0] versus 10.9 months [95% CI, 9.5-12.6], respectively, and response rate was 38% versus 25%, showing some benefit, again, in OS in the upfront setting.
[They also took] a more detailed look at [OS and] PD-L1 expression. When PD-L1 expression was less than 1%, the HR was 0.62 [95% CI, 0.45-0.85]. When PD-L1 expression was greater than or equal to 1%, the HR was 0.64 [95% CI, 0.50-0.82]. [When expression was] greater than or equal to 50%, the HR was 0.66 [95% CI, 0.44-0.99]. [Finally], in the intermediate [range of PD-L1 expression], (1% to 49%), there was still a benefit, with a HR of 0.61 [95% CI, 0.44-0.84].11
Chemotherapy had more treatment-related AEs than did the nivolumab and ipilimumab plus chemotherapy. [These results] show that you can disperse some of the AEs by not stacking the drugs on top of each other, and [instead] giving them in a sequential manner. I thought this was a clever trial from that standpoint. Now we have approvals for both of these regimens, [the nivolumab plus ipilimumab regimen,13 and nivolumab, ipilimumab, plus chemotherapy regimen].14
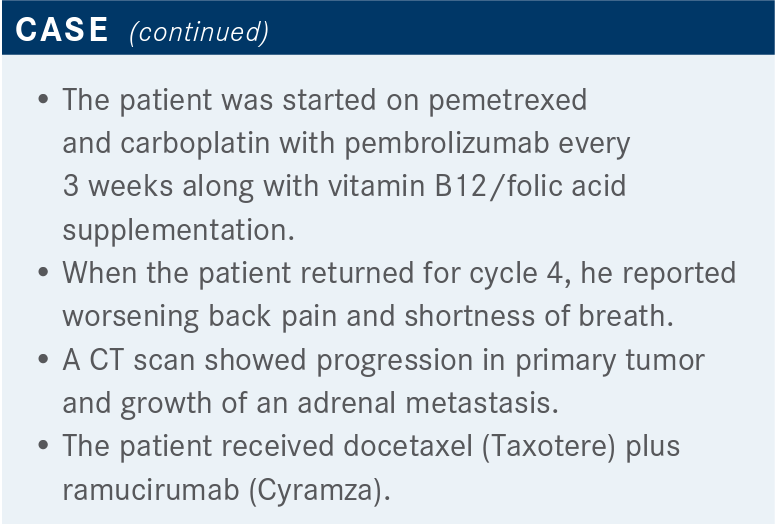
What are the data describing the efficacy and side effects of docetaxel (Taxotere) and ramucirumab (Cyramza)?
REVEL [NCT01168973] was [a study of docetaxel with either ramucirumab or with placebo]. [According to the design, patients had had] 1 platinum-based chemotherapy; prior bevacizumab was allowed, as were both [squamous and non-squamous] histologies.15 Ramucirumab is a VEGF-targeted drug; [it is] a little different than bevacizumab, and the study did allow prior [treatment with] bevacizumab. They did have some of the traditional VEGF exclusion criteria in this study, because there was a little bit of fear in that, but again, it’s a different drug than bevacizumab, so people were treated [until] progression.
[This study takes us back] to when we didn’t have a lot of biologic driver mutation data or subsets. Median OS was slightly better with ramucirumab, 10.5 months versus 9.1 months [HR, 0.86; 95% CI, 0.75-0.98; P = .02]. Progression-free survival improved from 3.0 months to 4.5 months [HR, 0.76; 95% CI, 0.68-0.86; P < .0001]. The objective response rate was probably the most robust [data point], 23% versus 14% [odds ratio, 1.89; 95% CI, 1.41-2.54; P < .0001].15
There was an exploratory [analysis]. They defined refractory [in terms of] the best response of progressive disease to first-line therapy, so these were patients who did not get stable disease or any type of response, and then progression. There were 360 patients like that.16 [The investigators] wanted to see if, indeed, being aggressive with this combination was helpful.
The efficacy breakdown was purely a post hoc analysis. The median OS was in favor of ramucirumab plus docetaxel, and whether duration of the first-line therapy was 4, 8, or 12 weeks, there was a benefit across the board; for example, HR at 12 weeks was 0.85 [95% CI, 0.68-1.05]. What it speaks to is that, if you see someone who’s in trouble, especially who’s having progression like this, maybe it’s okay to be a little more aggressive. I think finding a clinical trial would be nice, especially in patients who are refractory to immunotherapy, especially when they progress quickly.
We do know that there are some AEs. Treatment-emergent AEs of grade 3 or higher were more common in the ramucirumab group [79% vs 71%],15 as well as treatment-emergent AEs that were related to discontinuation [5% vs 4%], there were definitely higher numbers with the ramucirumab and docetaxel. 16 Docetaxel by itself is not a benign regimen; it does have AEs.
REFERENCES
1. NCCN. Clinical Practice Guidelines in Oncology. Non–small cell lung cancer, version 5.2021. Accessed June 28, 2021. https://bit.ly/3dY9QPN
2. Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al; KEYNOTE-189 Investigators. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078-2092. doi:10.1056/NEJMoa1801005
3. Gadgeel S, Rodríguez-Abreu D, Speranza G, et al. Updated analysis from KEYNOTE-189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non–small-cell lung cancer. J Clin Oncol. 2020;38(14):1505-1517. doi:10.1200/JCO.19.03136
4. Mok TSK, Wu YL, Kudaba I, et al; KEYNOTE-042 Investigators. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819-1830. doi:10.1016/S0140-6736(18)32409-7
5. Lopes G, Wu YL, Kudaba I, et al. Pembrolizumab (pembro) versus platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1%: open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 2018;36(suppl 18). doi:10.1200/JCO.2018.36.18_suppl.LBA4
6. Socinski MA, Jotte R, Cappuzzo F, et al. Overall survival (OS) analysis of IMpower150, a randomized Ph 3 study of atezolizumab (atezo) + chemotherapy (chemo) ± bevacizumab (bev) vs chemo + bev in 1L nonsquamous (NSQ) NSCLC. J Clin Oncol. 2018;36(suppl 15):9002. doi:10.1200/JCO.2018.36.15_suppl.9002
7. Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288-2301. doi:10.1056/NEJMoa1716948
8. Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093-2104. doi:10.1056/NEJMoa1801946
9. Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non–small-cell lung cancer. N Engl J Med. 2019;381(21):2020-2031. doi:10.1056/NEJMoa1910231
10. Ramalingam SS, Ciuleanu TE, Pluzanski A, et al. Nivolumab + ipilimumab versus platinum-doublet chemotherapy as first-line treatment for advanced non-small cell lung cancer: three-year update from CheckMate 227 part 1. J Clin Oncol. 2020;38(suppl 15):9500. doi:10.1200/JCO.2020.38.15_suppl.9500
11. Reck M, Ciuleanu TE, Cobo Dols M, et al. Nivolumab (NIVO) + ipilimumab (IPI) + 2 cycles of platinum-doublet chemotherapy (chemo) vs 4 cycles chemo as first-line (1L) treatment (tx) for stage IV/recurrent non-small cell lung cancer (NSCLC): CheckMate 9LA. J Clin Oncol. 2020;38(suppl 15):9501. doi:10.1200/JCO.2020.38.15_suppl.9501
12. Paz-Ares L, Ciuleanu T-E, Cobo M, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non-small-cell lung cancer (CheckMate 9LA): an international, randomised, open-label, phase 3 trial. Lancet Oncology. 2021;22(2):198-211. Published correction appears in Lancet Oncology. 2021;22(3):e92. doi:10.1016/S1470-2045(20)30641-0
13. FDA approves nivolumab plus ipilimumab for first-line mNSCLC (PD-L1 tumor expression ≥1%). FDA. Published May 15, 2020. Accessed July 8, 2021. https://bit.ly/3yGo5jY
14. FDA approves nivolumab plus ipilimumab and chemotherapy for first-line treatment of metastatic NSCLC. News release. US Food and Drug Administration. Updated May 27, 2020. Accessed June 29, 2021. https://bit.ly/2UCBZow
15. Garon EB, Ciuleanu TE, Arrieta O, et al. Ramucirumab plus docetaxel versus placebo plus docetaxel for second-line treatment of stage IV non-small-cell lung cancer after disease progression on platinum-based therapy (REVEL): a multicentre, double-blind, randomised phase 3 trial. Lancet. 2014;384(9944):665-673. doi:10.1016/S0140-6736(14)60845-X
16. Reck M, Paz-Ares L, Bidoli P, et al. Outcomes in patients with aggressive or refractory disease from REVEL: a randomized phase III study of docetaxel with ramucirumab or placebo for second-line treatment of stage IV non-small-cell lung cancer. Lung Cancer. 2017;112:181-187. doi:10.1016/j.lungcan.2017.07.038
