Rabinowits Discusses Treatment Options in Medullary Thyroid Cancer
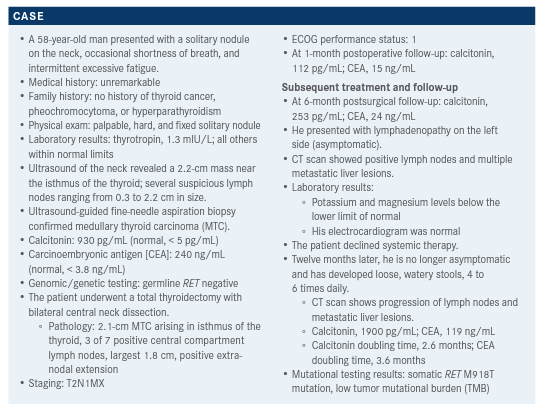
During a Targeted Oncology Case-Based Roundtable event, Guilherme Rabinowits, MD, discussed the case of a 58-year-old patient with medullary thyroid cancer.
Guilherme Rabinowits, MD

During a Targeted OncologyTM Case-Based Roundtable event, Guilherme Rabinowits, MD of the Medical Oncology at Miami Cancer Institute, Baptist Health South Florida, discussed the case of a 58-year-old patient with medullary thyroid cancer.
Targeted OncologyTM: How do you treat advanced or metastatic MTC that harbors a RET alteration?
RABINOWITS: The National Comprehensive Cancer Network [NCCN] guidelines1 [for recurrent or persistent MTC with distant metastases] talk about antiangiogenic multikinase inhibitors vandetanib [Caprelsa] and cabo-zantinib [Cabometyx], and now [RET-targeted therapies] selpercatinib [Retevmo] and pralsetinib [Gavreto] are recommended as well. The guidelines also recommend [pembrolizumab (Keytruda)] immunotherapy for patients with a high TMB.
When patients with metastatic MTC have RET alterations, does that influence your selection of therapy?
It’s important to know that not all RET mutations respond the same. You could use a RET inhibitor, but some patients with RET mutations show resistance to RET inhibitors. Not a lot of data [are really available on] that. But keep in mind that just because somebody has a RET mutation, that [doesn’t] mean that RET mutation is going to be very sensitive to RET inhibitors. However, the majority of mutations respond very well, particularly this M918T mutation that was mentioned in this patient. I think the data [we discuss here] will guide us.
The ZETA trial [NCT00410761] was a phase 3 trial with over 300 patients, designed to look at vandetanib vs placebo for patients with advanced or metastatic MTC.2 The hazard ratio for overall survival was not reached yet by the time of the analysis [HR, 0.89; 95% CI, 0.481.65]. Progression-free survival [PFS] curves suggest improvement of PFS with vandetanib vs placebo [HR, 0.46; 95% CI, 0.31-0.69; P < .001], and 6-month PFS [rates were] 91% vs 74%, respectively. Objective response rates [ORRs] were 45% vs 13%, respectively [odds ratio (OR), 5.48; 95% CI, 2.99-10.79; P < .001]. The disease control rates were 87% vs 71% [OR, 2.64; 95% CI, 1.484.69; P = .001]. The biochemical response rates were 69% vs 3% for calcitonin [OR, 72.9; 95% CI, 26.2-303.2; P < .001], and 52% vs 2% for CEA [OR, 52.0; 95% CI, 16.0320.3; P < .001].
How did RET alterations affect the efficacy of vandetanib?
Among patients with sporadic disease, those with the RET M918T mutation derived most of the benefit. This was in comparison with patients with no RET mutation and …patients with unknown RET mutation status. When treated with vandetanib, patients with the M918T mutation had a superior response to vandetanib with respect to PFS; the event rate was 34.7% in the M918T mutation–positive group, 38.9% in the M918T mutation–negative group, and 20.8% in the group with unknown M918T status. The M918T mutation–positive group also showed an ORR of 54.5%, while those who tested negative for the mutation had an ORR of 30.9% and those with unknown mutation status had an ORR of 33.3%.2 This suggests that most of the benefit [of vandetanib] is driven by RET inhibition.
The most common adverse effect [AE] of any grade was diarrhea, occurring in 56% of the patients. Other common AEs included rash, hypertension—a lot of these patients end up on hypertensive drugs—fatigue, headache, and decreased appetite, AEs commonly [caused by] tyrosine kinase inhibitors [TKIs]. Also, it is important to be aware of QT prolongation and make sure that you’re monitoring electrolytes and electrocardiogram results for patients who are at high risk of developing QT prolongation.
Did cabozantinib show particular efficacy in patients with altered RET?
The phase 3 EXAM study [NCT00704730] looked at cabozantinib [vs placebo] for advanced or metastatic MTC in over 300 patients. ORRs for cabozantinib vs placebo were 28% vs 0%, respectively [P < .001].3 Cabozantinib [was associated with] improvement in median PFS when compared with placebo [11.2 months vs 4.0 months; HR, 0.28; 95% CI, 0.19-0.40; P < .001]. Median overall survival improvement was not significant [stratified HR, 0.85; 95% CI, 0.64-1.12; P = .24].4 But those 2 drugs [vandetanib and cabozantinib] were approved based on PFS improvement and activity in these patients.
In a subgroup analysis of patients with unspecified RET mutation—positive, negative, or unknown status— cabozantinib showed a significant benefit for the RET mutation–positive group in terms of PFS but not overall survival.4
Subgroup analysis was also performed with respect to the M918T mutation. ORRs were 34% for the RET M918T mutation–positive and 20% for the RET M918T mutation–negative subgroups. With cabozantinib, the M918T mutation–positive group showed significantly improved PFS [HR, 0.15; 95% CI, 0.08-0.28; P < .0001]; the M918T mutation–negative group did not [HR, 0.67; 95% CI, 0.37-1.23; P = .19]. Additionally, the treated M918T mutation–positive group had a median overall survival of 44.3 months [vs 18.9 months with placebo (HR, 0.60; 95% CI, 0.38-0.94; P = .03)]. There was no significant overall survival benefit for the M918T mutation–negative group [HR, 1.12; 95% CI, 0.70-1.82; P = .63].
The most common AEs were diarrhea, decreased weight, palmar-plantar erythrodysesthesia syndrome, decreased appetite, nausea, and fatigue. We also see patients with a white discoloration of the hair, stomatitis, and increased alanine and aspartate transferase levels.
What data support the use of RET-specific therapies and how do these perform in patients with RET alterations other than M918T? How does prior therapy with cabozantinib or vandetanib influence efficacy? In the LIBRETTO-001 trial [of selpercatinib (NCT03157128)] there were 38 patients with non-MTC and 300 with metastatic MTC. All of them had a RET mutation, either a fusion mutation for those with non-MTC or a point mutation for [those with] MTC. There were 8 patients who were systemic therapy–naive and 19 [with RET fusion–positive MTC who] had been previously treated. There were 88 patients [with RET-mutant MTC] not previously treated with cabozantinib or vandetanib and 55 patients [with RET-mutant MTC] previously treated with cabozantinib, vandetanib, or both.
The majority of RET [point] mutations were M918T, [representing] 57% of the patients [with RET-mutant MTC].6 The majority of patients were men, with a median age of 57 years in the group previously treated with cabozantinib, vandetanib, or both, and 58 years in the cabozantinib-vandetanib–naive group. The median number of prior regimens was 2 in the group [whose] patients had received TKIs. [In this group], the percentage of patients who had received only cabozantinib was 24%; only vandetanib, 33%; and both cabozantinib and vandetanib, 44%.5
Among the patients with previously treated RET-mutant MTC, 9% had a complete response [CR] and 60% had a partial response [PR], for a 69% ORR [95% CI, 55%-81%]. Another 25% had stable disease [SD]. For patients with RET-mutant MTC who had not been previously treated, 11% had a CR and 61% had a PR, for a 72% ORR [95% CI, 62%-82%], and 23% [had] SD. Among previously treated patients with RET fusion–positive thyroid cancer, 5% had a CR and 74% had a PR, for a 79% ORR [95% CI, 54%-94%], with SD in 21%. Among the patients who had RET fusion–positive thyroid cancer that had not been previously treated, you have 12.5% with a CR and 88% with a PR. Median duration of response [DOR] and PFS for patients with previously treated RET-mutant MTC was not estimable [NE]. A median DOR of 22.0 months [95% CI, NE-NE] and a median PFS of 23.6 months [95% CI, NE-NE] were observed for patients with RET-mutant MTC that had not been previously treated. A median DOR of 18.4 months [95% CI, 7.6-NE] and a median PFS of 20.1 months [95% CI, 9.4-NE] were observed for patients who were previously treated with RET fusion–positive thyroid cancer. It’s pretty impressive activity and durable responses.
Treatment-related AEs occurred in 153 [patients]. Twenty-eight percent [of all AEs were treatment-related and] of grade 3; only 2% were grade 4, and any grade about 94%. The majority of patients had some AEs but [most] were grade 1 or 2. These included dry mouth, hypertension, diarrhea, fatigue, increased alanine and aspartate transferase levels, nausea, constipation, and peripheral edema.
Can you discuss other trials in this patient population? We can move now to the ARROW study [NCT03037385], which used pralsetinib in patients [with MTC]. This study looked at RET-mutant MTC with prior cabozantinib, vandetanib, or both; RET-mutant MTC with no prior systemic therapy; and RET-mutant MTC with prior systemic therapy other than cabozantinib and vandetanib. They looked at other RET-altered tumors also, but we’re looking at only the data on MTC.7,8
There was a median age of 59 years in the previously treated group and 61 years in the cabozantinib-vandetanib–naive group, which is normally what we see for those patients. The majority were male, White, and had excellent ECOG performance status.8 Seven percent of the patients who had prior cabozantinib, vandetanib, or both had central nervous system [CNS] disease currently or previously, and 14% of the patients who were cabozantinib and vandetanib naive also had CNS disease history.7,8 The median number of prior therapies was 2 among patients who had prior cabozantinib, vandetanib, or both, and 28% of the patients who were naive of cabozantinib and vandetanib had received 3 or fewer lines of therapy.8 Some of the [treatment]-naive patients had immunotherapy also, probably because of the TMB.
The ORR for patients who had [prior treatment with] cabozantinib, vandetanib, or both was 60% [95% CI, 46%-73%], and for patients who were naive of therapies, 66% [95% CI, 46%-82%]. You have almost a 2% CR rate for patients who had prior TKIs vs 10% CR for patients who were naive of prior TKIs. DOR has not been reached. A DOR of 6 months or greater was [observed in] 79% of patients with prior TKIs and 84% of patients naive of TKIs.
For the toxicity pattern of this therapy [among 138 treated patients] you can have musculoskeletal complaints—about 42% [for grades 1 to 4] but only 0.7% for grades 3 and 4. You can have gastrointestinal symptoms also; these were constipation, diarrhea, abdominal pain, xerostomia, stomatitis, and nausea, and the majority were of grade 1 to 2. Fatigue, edema, fevers, headaches, peripheral neuropathy, dizziness, dysgeusia, cough, dyspnea, and rash…can [all] happen, but they tend to be only grade 1 and 2. Hypertension also occurred; half the cases were grade 1 and 2 and the other half were grade 3 and 4, so keep [the risk of hypertension] in mind. There have been a few cases of tumor lysis syndrome in these patients, so keep that in mind as well. It was not common, [occurring in less than 15% of patients], but it can happen.
What are the triggers to initiate systemic therapy?
[For] systemic therapy for all differentiated thyroid cancers, we usually start [treatment] when [patients] become refractory. [Pralsetinib is one example;] according to the FDA, “On December 1, 2020, the FDA approved pralsetinib for adult and pediatric patients 12 years [of age] and older with advanced [or] metastatic RET-mutant MTC who require systemic therapy or RET fusion–positive thyroid cancer who require systemic therapy, and who are radioactive iodine–refractory.”9
REFERENCES:
1. NCCN. Clinical Practice Guidelines in Oncology. Thyroid carcinoma, version 1.2021. Accessed June 23, 2021. https://bit.ly/2UgzDfa
2. Wells Jr SA, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134-141. doi:10.1200/JCO.2011.35.5040
3. Elisei R, Schlumberger MJ, Müller SP, et al. Cabozantinib in progres-sive medullary thyroid cancer. J Clin Oncol. 2013;31(29):3639-3646. doi:10.1200/JCO.2012.48.4659
4. Schlumberger M, Elisei R, Müller S, et al. Overall survival analysis of EXAM, a phase III trial of cabozantinib in patients with radiographically progressive medullary thyroid carcinoma. Ann Oncol. 2017;28(11):2813-2819. doi:10.1093/annonc/mdx479
5. Wirth LJ, Sherman E, Robinson B, et al. Efficacy of selpercatinib in RET-altered thyroid cancers. N Engl J Med. 2020;383(9):825-835. doi:10.1056/NEJMoa2005651
6. Wirth L, Sherman E, Drilon A, et al. Registrational results of LIBRETTO-001: a phase 1/2 trial of selpercatinib (LOXO-292) in patients with RET-altered thyroid cancers. Paper presented at: European Society for Medical Oncology Congress 2019; September 27-October 1, 2019; Barcelona, Spain.
7. Hu M, Subbiah V, Wirth LJ, et al. Results from the registrational phase I/II ARROW trial of pralsetinib (BLU-667) in patients (pts) with advanced RET mutation-positive medullary thyroid cancer RET + MTC). Ann Oncol. 2020;31(suppl 4):S1084. doi:10.1016/j.annonc.2020.08.1401
8. Gavreto. Prescribing information. Genentech/Blueprint Medicines Corp; 2021. Accessed June 26, 2021. https://bit.ly/3duLFsa9. FDA approves pralsetinib for RET-altered thyroid cancers. FDA. December 1, 2020. Accessed June 26, 2021. https://bit.ly/3xlfoLG

Anticipating Novel Options for the RAI-Refractory DTC Armamentarium
May 15th 2023In season 4, episode 6 of Targeted Talks, Warren Swegal, MD, takes a multidisciplinary look at the RAI-refractory differentiated thyroid cancer treatment landscape, including the research behind 2 promising systemic therapy options.
Listen